Lower Limb Nerve Injuries Flashcards
(118 cards)
Organisation of Lower Limb nerves
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between … and L2)
- Below - cauda … - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)

Organisation of Lower Limb nerves
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and …)
- Below - … equina - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L…/L4 - below spinal cord end)
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)

Organisation of Lower Limb nerves
- Lower limb nerves starts in … horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - … puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)

Organisation of Lower Limb nerves
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - lumbar puncture go below end of spinal cord (lie laterally, … crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)
- Lower limb nerves starts in anterior horn cell within spinal cord (spinal cord stops between L1 and L2)
- Below - cauda equina - lumbar puncture go below end of spinal cord (lie laterally, iliac crest - 1 or 2 spaces above would be L3/L4 - below spinal cord end)

Cauda equina vs conus lesions


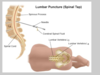
Landmarks for lumbar puncture
- Below end of … … - lie laterally, find iliac … - 1 or 2 spaces above = below spinal cord which will be around L3,L4 (spinal cord ends at …)
- Below end of spinal cord - lie laterally, find iliac crest - 1 or 2 spaces above = below spinal cord which will be around L3,L4 (spinal cord ends at L1/L2)
Cauda equina vs conus medullaris


Cauda equina vs conus medullaris


Cauda equina vs conus medullaris


Causes of Cauda equina
- Disc …
- … fracture
- T…
- Disc herniation
- Spinal fracture
- Tumours
3 causes of cauda equina are…
- Disc herniation
- Spinal fracture
- Tumours
Causes of Conus medullaris
- Disc …, T..
- … conditions (e.g. Chronic Inflammatory Demyelinating Polyradiculopathy ,Sarcoidosis)
- … (E.g. CMV, HSV, EBV, Lyme, TB)
- Disc herniation, tumour,
- Inflammatory conditions (e.g. Chronic Inflammatory Demyelinating Polyradiculopathy ,Sarcoidosis)
- Infection (E.g. CMV, HSV, EBV, Lyme, TB)
Causes of Conus medullaris (4)
- Disc herniation
- Tumour
- Inflammatory conditions (Chronic Inflammatory Demyelinating Polyradiculopathy Sarcoidosis)
- Infection (e.g. CMV, HSV, EBV, Lyme, TB)
This shows a …

L5/S1 disc herniation compressing cauda equina
Nerve Root Entrapment – ‘sciatica
- Compression- Disc- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L…, S… n. root impingement
- L… n. root – exits between L…/ S…vertebral bodies S… n. root exits between S… / S… vertebral bodies
- Pain may be felt in dermatome (sharp/ superficial) or myotome (deep ache)
- Compression- Disc- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L5, S1 n. root impingement
- L5 n. root – exits between L5/ S1 vertebral bodies S1 n. root exits between S1 / S2 vertebral bodies
- Pain may be felt in dermatome (sharp/ superficial) or myotome (deep ache)

Nerve Root Entrapment – ‘sciatica
- Compression- Disc- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L5, S1 n. root …
- L5 n. root – exits between L5/ S1 vertebral bodies S1 n. root exits between S1 / S2 vertebral bodies
- Pain may be felt in … (sharp/ superficial) or … (deep ache)
- Compression- Disc- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L5, S1 n. root impingement
- L5 n. root – exits between L5/ S1 vertebral bodies S1 n. root exits between S1 / S2 vertebral bodies
- Pain may be felt in dermatome (sharp/ superficial) or myotome (deep ache)

Nerve Root Entrapment – ‘sciatica
- Compression- …- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L5, S1 n. … impingement
- L5 n. root – exits between L5/ S1 vertebral bodies S1 n. root exits between S1 / S2 vertebral bodies
- Pain may be felt in dermatome (s…/ s…) or myotome (… ache)
- Compression- Disc- posterior central, lateral Bone- osteophyte Ligaments
- Small canal- stenosis
- Sciatica – usually L5, S1 n. root impingement
- L5 n. root – exits between L5/ S1 vertebral bodies S1 n. root exits between S1 / S2 vertebral bodies
- Pain may be felt in dermatome (sharp/ superficial) or myotome (deep ache)

Lower Limb Root Lesions - reflex and sensory loss
- Lower limb dermatomes more variable than upper limb
- L1 … area
- L2 front of … (front pocket)
- L3 front of …
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of knee
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1

Lower Limb Root Lesions - reflex and sensory loss
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of knee
- L4 front- inner/ … leg
- L5 … leg, … of foot, inner …
- S1 … toe, rest of …, back of leg
- S2 thigh to top of … (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of knee
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1

Lower Limb Root Lesions - reflex and sensory loss
- Lower limb dermatomes more variable than upper limb
- L1 … area
- L2 front of thigh (… pocket)
- L3 front of knee
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 … to top of buttock (… pocket)
- S3-S5 … rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of knee
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1

Lower Limb Root Lesions - reflex and sensory loss
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of …
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round …/ …
- … jerk L4, … jerk S1
- Lower limb dermatomes more variable than upper limb
- L1 inguinal area
- L2 front of thigh (front pocket)
- L3 front of knee
- L4 front- inner/ medial leg
- L5 outer leg, dorsum of foot, inner sole
- S1 little toe, rest of sole, back of leg
- S2 thigh to top of buttock (back pocket)
- S3-S5 concentric rings round anus/ genitalia
- Knee jerk L4, Ankle jerk S1

Lower Limb Root Lesions - weakness
- L1/2 … flexion
- L3/4 … extension
- L4 … inversion
- L5 Knee flexion Ankle …
- Toe extension
- Foot inversion and eversion
- S1 Knee flexion
- Ankle plantar flexion
- Toe flexion Foot eversion
- L1/2 Hip flexion
- L3/4 Knee extension
- L4 Foot inversion
- L5 Knee flexion Ankle dorsiflexion
- Toe extension
- Foot inversion and eversion
- S1 Knee flexion
- Ankle plantar flexion
- Toe flexion Foot eversion
Lower Limb Root Lesions - weakness
- L1/2 Hip flexion
- L3/4 Knee extension
- L4 Foot inversion
- L5 … flexion … dorsiflexion
- … extension
- Foot … and …
- S1 Knee flexion
- Ankle plantar flexion
- Toe flexion Foot eversion
- L1/2 Hip flexion
- L3/4 Knee extension
- L4 Foot inversion
-
L5 Knee flexion Ankle dorsiflexion
- Toe extension
- Foot inversion and eversion
- S1 Knee flexion
- Ankle plantar flexion
- Toe flexion Foot eversion
Lower Limb Root Lesions - weakness
- L1/2 Hip flexion
- L3/4 Knee extension
- L4 Foot inversion
- L5 Knee flexion Ankle dorsiflexion
- Toe extension
- Foot inversion and eversion
- S1 … flexion
- Ankle … flexion
- Toe … Foot …
- L1/2 Hip flexion
- L3/4 Knee extension
- L4 Foot inversion
- L5 Knee flexion Ankle dorsiflexion
- Toe extension
- Foot inversion and eversion
-
S1 Knee flexion
- Ankle plantar flexion
- Toe flexion Foot eversion



















































