[B] 1.28 Disturbances in keratinization Flashcards
Cytoplasmic filaments
Prekeratin
Keratohyalin granula
- Autophagocytosis
- Granular formation
Odland’s granules
Granula bordered by membranes
In the hornifying epithelium
- In the skin
- Modified appendix of the epithelium
- Hoof & horn
- Forestomachs
- Oesophagus
- On pars oesophagica (stomach)
- Mouth cavity
- Differs btw. species
- On the back of the tongue
Give the process of keratinisation
- Cytoplasmic filaments
- Pre-keratin synthesis
- Keratohyalin-granula
- Amorphic electrondens granula
- Odland-granula formation

Disturbances in keratinisation
- Hyperkeratosis
- Hypokeratosis
- Rare
- Wasting diseases
- Starvation
- Parakeratosis
- Dyskeratosis
- Keratinisation of the str. spinosum
Hyperkeratosis - Local
- Intense epithelial hyperplasia
- Intense keratinisation in the str. corneum
- Cornu cutaneum
- Hard pad disease
Systemic hyperkeratosis causes
- Vitamin A deficiency
- Toxicoses: Chlorinated naphthalene
Summarise the forms of keratinisation disturbances
- Hyperkeratosis
- Congenital - Acquired
- Local - Generalised
- Hypokeratosis
- Parakeratosis
- Dyskeratosis
Characteristics of hyperkeratosis
- No desquamation
- Thicker superficial layer
Local hyperkeratosis
- Mechanical cause
- Chronic inflammation/circulatory disturbance
- Malformation
- Trophoneuroticus disturbance
Local hyperkeratosis:
- Mechanical cause
- Callositas
- Tyloma/ Callus
Local hyperkeratosis:
- Chronic inflammation/circulatory disturbance
Pachydermia
Local hyperkeratosis:
- Malformation
Cornu cutaneum
Local hyperkeratosis:
- Trophoneuroticus disturbances
Hard pad disease
Generalised hyperkeratosis
- A-avitaminosis
- Chloronaphthalene intoxication
- Biotin deficiency (turkey)
- Toxical floor (piglets)
-
Ichthyosis congenita
- Recessive genetical lethal factor

Parakeratosis
- Hornifying layer thicker
- Nuclei still present close to the surface
- Skin oedema
- Chronic inflammation (skin & rumen)
- Zn-deficiency (Pigs skin)
Parakeratosis - Cellular level
- Lack of granules
- Retained nuclei of epithelial cells in the stratum corneum
Hyper- and parakeratosis of the rumen leads to…
Liver abscessation
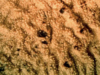
Steps of hyper- & parakeratosis of the rumen → Liver abscessation
- Hyper- & parakeratosis - Locus minoris resistenciae
- Colonising pathogenic bacteria
- Chronic inflammation
- Bacteria in the propria → V. portae → liver
- Purulent (pussy), ichorous and/or necrotising inflammation
Dyskeratosis
- Keratinisation starts in the stratum spinosum
- Secondary lesion
- Rare


