CVPR Week 6: Control of ventilation Flashcards
Objectives

CNS respiratory centers location
Medulla and Pons
Basic elements of the respiratory control system
7 listed
- Pain/emotional stimuli
- Higher brain centers - voluntary control
- Stretch receptors in the lungs
- Irritant receptors in the lungs
- Muscle/joint receptors in the lungs
- Central chemoreceptors
- Peripheral chemoreceptors

Central chemoreceptors detect?
increased CO2
increased [H+} concentration
Peripheral chemoreceptors detect?
- decreased O2
- increased CO2
- increased [H+]
Where are central chemoreceptors
in cerebrospinal fluid and sense CO2 and H+
Where are the peripheral chemoreceptors?
carotid and aortic bodies
Controller of the respiratory control system
Brainstem medulla and pons respiratory centers
Sensors of the respiratory control system?
Central and peripheral chemoreceptors
Controlled variables of respiratory control system?
PaCO2
PaO2
Arterial pH
Effectors of the respiratory control system
Muscles of respiration
Identify respiratory control system components


Innervation of central chemoreceptors
Direct central connections
Innervation of peripheral chemoreceptors
- vagus nerve for aortic bodies
- glossopharyngeal nerve for carotid bodies
Muscles of respiration innervation
- Respiratory somatic motor neurons
The role of the muscles of respiration in the respiratory control system
innervated by respiratory motor neurons that alter respiration to induce changes in blood gasses PaCO2, PaO2 and arterial pH
Basic respiratory rhythm generator location
Medulla

if the spinal cord is severed just below the pons but above the medulla
basic respiratory rhythm is preserved
if the spinal cord is severed just below the medulla
all breathing stops
Neurons active in the respiratory cycle
Groups of medullary neurons are active in either the inspiratory or the expiratory phase of the respiratory cycle
Medullary neurons active during inspiration
Dorsal respiratory group
When are the ventral respiratory group active
during inspiration and expiration
Dorsal respiratory group location
within the nucleus of the tractus solitarius (NTS)
The dorsal respiratory group receives information from?
receives afferent information from the vagus and glossopharyngeal nerves
The dorsal respiratory group is active during?
The inspiratory phase of the respiratory cycle
The dorsal respiratory group project to?
ventral respiratory group (VRG) and to inspiratory motor neurons
The ventral respiratory group is located in?
The VRG is located in the nucleus ambiguous (NA) and the nucleus retroambiguus (NRA)
The ventral respiratory group afferents from
(DRG) Dorsal respiratory group
The ventral respiratory group efferents to
motor neurons active both in inspiration and expiration
The respiratory centers of the pons
The pons contains centers (pontine respiratory groups) (PRG) that apparently receive vagal afferent information and project to the medulla thereby modifying medullary output.
PRG AKA
Pontine respiratory groups
Pontine respiratory groups receive afferents from?
vagal afferent information
Pontine respiratory groups efferents to?
the medulla thereby modifying medullary output
Pontine respiratory groups input is most likely? and results in?
information from lung mechanoreceptors (Pneumotaxic center) and results in fine-tuning of ventilation
Lung mechanoreceptor center location
The pneumotaxic center which resides in the upper 1/3 of the pons and the apneustic center in the lower pons
Higher centers of respiratory control
- Cerebral centers are capable of over-riding ventilatory control
- For example, we can voluntarily hold our breath thereby interrupting normal respiratory rhythm
Chemical control of ventilation
The most potent stimulus for ventilation is arterial CO2 tension
The ventilatory response to CO2 can be most easily demonstrated by having a subject breathe air containing this gas as shown in the figure to the right
The most potent stimulus for ventilation control is?
Arterial CO2 tension
The ventilatory response to CO2
- The ventilatory response to CO2 can be most easily demonstrated by having a subject breathe air containing this gas
- respiratory volume/min increases as PaCO2 increases

Where are the chemosensitive areas?
they are on the ventral surface of the medulla

Chemosensitive areas AKA
Central chemoreceptors
Central chemoreceptors location
located on the ventral surface of the medulla

Peripheral chemoreceptor location
located in carotid and aortic bodies
Central chemoreceptors relationship to DRG and VRG
distinct from the DRG and VRG but DO communicate directly with the DRG
Central chemoreceptors sensory mechanism
- Central chemoreceptors lie in proximity to arteries and are bathed in cerebrospinal fluid (CSF)
- CO2 is very permeable across the Blood-brain barrier and therefore diffuses from the blood into the interstitial fluid around the central chemoreceptors
- Here the CO2 reacts with water to form bicarbonate ion (HCO3-) and H+
- These receptors are stimulated by H+ formed in the CSF by CO2 diffusing across the blood-brain barrier and not blood-borne H+
CO2 + H2O equation

Buffering system of CSF
- CSF is much less buffered than plasma thus small changes in CO2 tension result in significant H+ formation
- However, the buffering system can undergo changes and the buffering capacity of this compartment can change
Blood-brain permeability to H+
The blood-brain barrier is very IMpermeable to H+ and so central chemoreceptors are affected by PaCO2 changes
Peripheral chemoreceptors sense?
PaCO2
The importance of central vs peripheral chemoreceptors in CO2 reception
- Central chemoreceptors are responsible for 80% of the response
- Peripheral chemoreceptors are responsible for 20% of the response
Peripheral chemoreceptors sensory mechanism of CO2
- peripheral receptors respond directly to PaCO2
Carotid bodies location
the carotid body chemoreceptors lie at the carotid bifurcation
Aortic bodies location
The aortic bodies are distributed within the wall of the aortic arch and nearby vessels
Carotid bodies send afferent information to?
the brainstem via the carotid sinus nerve which is a branch of the glossopharyngeal nerve
Aortic bodies send afferent information to?
the brainstem via the aortic nerve, a branch of the vagus nerve
Mechanism of arterial PCO2 regulation
- Note the inverse relationship between alveolar CO2 and alveolar ventilation
- This relationship is the basis for the feedback control of the system
- For example if CO2 production were to increase, thereby momentarily increasing arterial PCO2 the response of this reflex would be to increase alveolar ventilation to restore CO2 toward control
Chemical control of ventilation by O2
another stimulus for ventilation is low oxygen or hypoxia
Chemoreceptors location for Oxygen
Peripheral chemoreceptors: carotid and aortic bodies
Central chemoreceptors: None
central chemoreceptor response to hypoxia
- No response, if the glossopharyngeal and vagus nerves are severed, hypoxia does not increase ventilation
- In fact, ventilation is decreased due to depression of the central respiratory centers by hypoxia
Peripheral chemoreceptor sensory mechanism for O2
the peripheral chemoreceptors are stimulated by decreases in PaO2 and hypoxia elicits an increase in firing rate of these receptors
Peripheral chemoreceptor ventilatory response for O2
- The ventilatory response to decreasing O2 is non-linear and approaches hyperbolic
- However, due to the shape of the Hb-O2 dissociation curve it is not linearly related to PaO2
- Interestingly, if ventilatory response to hypoxia is plotted against O2 content or Hb-saturation instead of PaO2 the the relationship is linear
- Thus ventilation is proportionally related to the amount of oxygen in arterial blood and not the partial pressure of O2

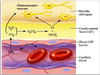
Mechanisms of O2 chemoreception
Most of the work involving PO2 chemoreception has focused on the carotid bodies since they are more easily studied than the aortic bodies
Cellular composition of the carotid body
4 listed
- Type I cells
- Type II cells
- afferent fibers of the carotid sinus nerve
- Endothelium
Type I cells of the carotid bodies AKA
Glomus cells
Glomus cells AKA
Type I cells of the carotid bodies
Glomus cells function
O2 sensor
Glomus cells features
- numerous mitochondria
- extensive rough endoplasmic reticulum
- Vesicles containing putative neurotransmitters (NT)
Type II cells of carotid bodies features
- not innervated
- may play a supporting role for Type I cells
Afferent fibers of the carotid sinus nerve features
synapse with Type I cells
Endothelium of the carotid bodies features
Highly vascular and has the highest blood flow/g tissue of any organ
What organ has the highest blood flow/g tissue of any organ?
The endothelium of the carotid bodies
Type II cells of the carotid body
- not innervated
- may play a supporting role for type I cells
Afferent fibers of the carotid sinus nerve synapse
synapse with Type I cells
The response of type I carotid body cells to hypoxia
- Respond to changes in O2 partial pressure
- hypoxia elicits an increase in firing rate of these receptors
- The proposed mechanism for the chemosensitive behavior of these cells is thought to be due to a hypoxia-induced reduction in glomus cell K+ conductance
- The resulting membrane depolarization mediates Ca2+ influx through L-type Ca2+ channels (VGCC) release of NT onto afferent nerve terminals of the CSN and increased action potential frequency in the CSN
- The specific K+ channel involved and the mechanism by which hypoxia inhibits these channels is debated and a focus of current research
Proposed neurotransmitters of the carotid bodies
The carotid bodies produce a wide variety of neurotransmitters currently ACh and ATP are the primary neurotransmitters released by hypoxia that excite afferent nerves

Afferent information from the carotid bodies travel to?
via the glossopharyngeal nerve to the medulla
Arterial PO2 regulation system

Arterial PO2 regulation controller
Medullary respiratory centers
Arterial PO2 regulation chemoreceptors
peripheral only
Arterial PO2 regulation values monitored
Arterial PO2
Arterial PO2 regulation effector pathway
Respiratory motor neurons
Arterial PO2 regulation effectors
muscles of respiration
Chemical controllers of ventilation
3 listed
- PaCO2
- PaO2
- arterial pH
Arterial pH ventilation control chemoreceptors location
- Peripherally only as primarily the carotid bodies
- Central peripheral chemoreceptors do not apply to arterial pH detection because the blood-brain barrier is impermeable to H+ and thus arterial pH is not centrally sensed
Arterial pH ventilation control stimulus and responses
These receptors sense pH of arterial blood
where acidemia (lower than normal arterial pH) causes increased ventilation resulting in increased CO2 removal
and
alkalemia (higher than normal pH) causes reduced ventilation resulting in reduced CO2 removal thereby increasing CO2 retention
Acute respiratory compensation for acid-base derangements
where acidemia (lower than normal arterial pH) causes increased ventilation resulting in increased CO2 removal
and
alkalemia (higher than normal pH) causes reduced ventilation resulting in reduced CO2 removal thereby increasing CO2 retention
Mechanism of carotid body pH chemoreception
- recent evidence supports roles for various ion channels in the response of glomus cells to acidic stimuli
- One group of likely candidates are the family of acid-sensing ion channels (ASICs) that are activated by diminished pH and conduct Na+ into the cell thereby eliciting depolarization leading to Ca2+ entry through voltage-gated Ca2+ channels and hence neurotransmitter release

Arterial pH control of the ventilation system

Arterial pH ventilation control controllers
Medullary respiratory centers
Arterial pH ventilation control sensors
Peripheral only chemoreceptors
Arterial pH ventilation control values monitored
arterial pH
Arterial pH ventilation control effector pathway
Respiratory motor neurons
Arterial pH ventilation control effectors
muscles of respiration
Effects of long-term derangements in blood gases on ventilatory control
Chronic alterations result in other organ system changes such as renal compensation, CSF buffering changes
Alveolar ventilation is inversely related to?
Alveolar and arterial PCO2
Chronic CO2 retention causes
can occur in serious cases of chronic obstructive lung diseases
Chronic CO2 retention compensations
- Renal compensation
- Buffering of CSF
Explain renal compensation in Chronic CO2 retention
- A decrease in arterial pH stimulates the kidneys to produce bicarbonate which raises arterial pH back to near normal levels
- the relationship between the bicarbonate concentration within the blood is provided by the Henderson-Hasselbach equation
Henderson-Hasselbalch equation for arterial pH
pH = pKa + log ([HCO3-/[CO2])
Buffering of CSF in Chronic CO2 retention
- Over several days bicarbonate will move down its concentration gradient from the blood to the CSF
- This move into the CSF greatly increases the buffering capacity of the CSF reducing the sensitivity of the central chemoreceptors
- Thus the CO2 ventilatory drive is impaired and these patients depend almost exclusively on the hypoxic ventilatory drive to maintain ventilation
Supplemental O2 therapy in Chronic CO2 retention
- If this hypoxic ventilatory drive is abolished due to therapy with 100% O2 such patients may develop severe hypoventilation and CO2 retention/acidemia since the only remaining stimulus for ventilation has been removed
- Supplemental O2 may additionally lead to CO2 retention in these patients by eliminating HPV thereby causing greater V/Q mismatch. Nevertheless, many COPD patients, even those with CO2 retention can tolerate normal O2 therapy.
**************************************************************************
Effects of high altitude on ventilation types
2 listed
- Effects of acute hypoxia
- Effects of chronic hypoxia
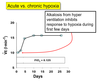
Acute hypoxia by altitude
- With ascent to high altitude, inspired PO2 decreases and ventilation is increased due to hypoxic stimulation of peripheral chemoreceptors
- However, since alveolar ventilation is increased, arterial PaCO2 is decreased and therefore the CO2 ventilatory drive is suppressed
- as a result arterial pH increases as a result of decreased PaCO2 which further blunts the ventilatory response to hypoxia
- Thus although overall ventilation is increased due to hypoxic drive, the ventilatory response is somewhat blunted by hypocapnia and alkalemia
Chronic hypoxia by altitude
- With long-term hypoxia the kidneys will adjust for this respiratory alkalemia by eliminating bicarbonate from the blood and thus raising arterial pH to near normal which takes one of the brakes off of ventilation that existed with acute hypoxia
- Over several days bicarbonate moves from the CSF to the blood down its concentration gradient, thus making CSF less well buffered which makes the central chemoreceptors more sensitive to arterial PaCO2 and the CO2 ventilatory drive will be ncreased. Therefore, ventilation is greater several days after arrival at high altitude compared to the initial response
- Upon return to low altitude, ventilation will persist at a level greater than that observed prior to ascent. The reason for this is that the CSF will remain less well buffered for some time and therefore the CO2 ventilatory drive will be greater than that prior to altitude exposure
Acute vs chronic hypoxia