5/19 UWorld Flashcards
(49 cards)
Describe how ethylene glycol affects the kidneys
- Ethylene glycol (anti-freeze) is absorbed from the GI tract and metabolized into glycolic acid (toxic to renal tubules - acute tubular necrosis) and oxalic acid (calcium oxalate cyrstals)
What is the function of the protein produced by Staph Aureus
Protein A is a component of Staph cell wall
It binds antibodies at Fc region, preventing complement from binding, and thus preventing opsinization and phagocytosis
Describe the defect causing mitochondrial myopathy
o Maternal inheritance only from mitochondrial DNA
o Without properly functioning mitochondria, cells cannot use oxidative phosphorylation to produce ATP
o Brain and skeletal muscle will be affected first due to high metabolic demand
Classic presentation and hallmark finding in mitochondrial myopathy
o Presentation:
§ Myopathy (muscle weakness, myalgia)
§ Lactic acidosis (due to impaired aerobic glycolysis)
§ Nervous system dysfunction (neuropathy, seizures)
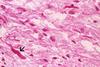
§ ***Muscle biopsy shows ragged red fibers (due to accumulation of diseased mitochondria)
Describe the funciton of IFN-a and IFN-b
- Secreted by virally-infected cells
- Act locally on uninfected cells to prime them for viral defense
- Bind to receptors in infected and neighboring cells, causing transcription of antiviral enzymes capable of halting protein synthesis
Describe how the enzymes transcribed by IFN-a and IFN-b to halt protein transcription only work on infected cells and not uninfected cells
These enzymes are only active in the presence of double stranded RNA, which forms in infected cells as a result of viral replication
So normal protein synthesis can still occur in uninfected cells and is selectively inhibited in virally infected cells
What is the MOA of statins
- Statins inhibit HMG CoA reductase, and thus prevent endogenous cholesterol production
- In response to decreased hepatic cholesterol synthesis, hepatocytes will increase LDL receptor expression on their surface, thus clearing LDL from circulation
MOA of Cholestyramine
Sketchy - Cho”lobster”amine
- Is a bile acid resin that bind bile acids in the intestinal lumen and prevent recycling of bile acids back to the liver
- The bind to bile acids and then bring them to the colon to be excreted
- Because there is a decrease in bile acids, the liver must promote synthesis of new bile acids (derived from cholesterol), depleting the liver cholesterol stores
- Liver will compensate by upregulating expression of LDL receptors, thus drawing LDL out of circulation
MOA of Ezetimibe
Sketchy = Z-shaped eel
Binds cholesterol in the GI tract, preventing their absorption (vs. Cholestyramine which binds bile acids)
MOA of fibrates
Sketchy = Gemfibrozil jellyfish
- Decreases serum VLDL (35-50%) and decreased triglycerides by activating PPAR-alpha at liver and peripheral tissues
- When activated, PPAR-alpha upregulates LPL at extra-hepatic sites
- This means increased hydrolysis of chylomicron and VLDL TG’s at peripheral tissues – aka decreased serum TGs
MOA of niacin
Sketchy = Lock Niacin monster
- Mechanism of action:
- Unknown
- Raises HDL (30%)
- Most effective drug for increasing serum HDL
- Decreases HDL cholesterol transfer and delaying HDL clearance
- Decreases VLDL, and thus decreased TG
MOA of fish oil
- Lowers TG by decreasing production of VLDL and Apo-B
- What is the drug of choice for anaerobic bacteria above the diaphragm vs. below the diaphragm
- Above = Clindamycin
- Below = Metronidazole
What are Nissl substances and where are they found
Nissl substances are found within RER of neurons
Seen in cell bodies and dendrites
Not in axons - axons do not contain RER
Describe the histopathologic changes seen in acute neuronal injury (red neuron)
- Due to transient severe insult that leads to cell death
- Histopathologic changes:
- Shrinkage of cell body
- Pyknosis of the nucleus
- Loss of Nissl substance
- Eosinophilic cytoplasm
Describe the histopathologic changes seen in axonal regeneration
- Enlargement of cell body
- Eccentric nucleus
- Enlargement of the nucleolus
- Dispersion of Nissl substance
Describe the histopatholic changes seen in neuronal atrophy
- Due to progressive degenerative disease
- Histopathologic changes:
- Loss of neurons and functional groups of neurons
- Reactive gliosis
Review rule of 4’s
What is the cause and effect of reperfusion injury
- Occurs when blood flow is returned to an ischemic area, causing increased killing of cells
- Due to:
- Oxygen free radical generation
- Severe, irreversible mitochondrial damage described as “mitochondrial permeability transition”
- Inflammation, which attracts neutrophils that cause additional injury
- Activation of complement pathway
- Leads to cell membrane damage
What is a common cause of isolated systolic HTN
Age-related increased arterial stiffening leading to decreased compliance of aorta and other major arteries
What apolipoprotein increases risk for Alzheimer’s and which decreases risk
ApoE2 decreases risk
ApoE4 increases risk
In what tumor do you see pseudopallisading cell arrangement
Glioblastoma multiforme
Tumor surrounding central necrosis
THINK:
- Pseudopallisading looks like a star = astrocyte
- Central area is necrotic/dead so this must be an old people tumor – astocyte tumor of adults = glioblastoma multiforme

What CNS tumor do you see fried egg apperance?
Oligendroglioma
What CNS tumor do you see Rosenthal fibers?
Pilocytic astrocytoma
Rosenthal fibers = eosinophilic corkscrew fibers
THINK: Chris Rossman putting the star (astrocytes) on the top of a child’s (tumor of children) christmas tree, so it has a swirly base (corkscrew fibers)