Other Papulosquamous Disease Flashcards
the ___ ___ eruption appears and consists of multiple discrete oval, erythematous, and scaly plaques and patches oriented along most commonly on the trunk and upper extremities. The face, palms, and soles are usually spared.
Pityriasis rosea
what is the characteristic patch of pityriasis rosea
a solitary scalypink plauq called the herald patch first appears on the trunk, with ensuing eruption appearing days to weaks later.
which areas are spared in pityriasis rosea
the face, palms and soles are usually spared, the trunk is most heavily affected in pityriasis rosea
pityriasis rosea is thought to be associated with systemic reactivation of human herpes virus ____ and ____
pityriasis rosea is thought to be associated with systemic reactivation of human herpes virus 6 and 7
for PR:Look for salmon-colored oval or circular patches and plaques with an associated fine collarette of scale. The condition usually begins with one larger truncal plaque or patch (the ___ ___). Then, after several days or weeks, new patches and plaques form along skin fold lines on the trunk – classically, this may appear in a ___ ___distribution.
Look for salmon-colored oval or circular patches and plaques with an associated fine collarette of scale. The condition usually begins with one larger truncal plaque or patch (the herald patch). Then, after several days or weeks, new patches and plaques form along skin fold lines on the trunk – classically, this may appear in a “Christmas tree” distribution.
Lichen planus (LP) is a condition in which ____ T lymphocytes attack____ _____s in the skin, mucous membranes, hair follicles, and/or nail units. The etiology is unclear, but viruses, medications, or contact allergens have all been implicated. LP is most common in adults in the fourth to sixth decades of life, but it may occur at any age. There is no known predilection for either sex or ethnicity.
Lichen planus (LP) is a condition in which autoreactive T lymphocytes attack basal keratinocytes in the skin, mucous membranes, hair follicles, and/or nail units. The etiology is unclear, but viruses, medications, or contact allergens have all been implicated. LP is most common in adults in the fourth to sixth decades of life, but it may occur at any age. There is no known predilection for either sex or ethnicity.
in LP, what is the characteristic lesion? where is the lesion located?
patients present with pruritic, flat-topped, pink to purple papules that are localized most commonly along the wrists, shings and presacral area. . Oral LP may occur on mucosal surfaces apposed to amalgams and other dental restorative materials.
outline some medications that can lead to lichen planus
Culprits include captopril, enalapril, labetalol, propranolol, methyldopa, calcium channel blockers, NSAIDs, chloroquine, hydroxychloroquine, quinacrine, thiazide diuretics, etanercept, infliximab, penicillamine, quinidine, and gold salts.
the koebner phenomemnon is hallmark for ___ and ____
LP and psoriasis. koebner phemonon is when trauma causes new lesions
describe the mucous membrane involvement of LP
lacy and netlike white plaques with a violaceous base. distinctly different than thrush.
Painful erosions and ulcers may also be seen, as well as atrophic, bullous, pigmented, and papular forms. Lesions may also be seen on the conjunctivae, the vulva, vagina, glans penis, anus, tonsils, larynx, and throughout the gastrointestinal tract.
treatment for lichen planus
• For drug related LP, withdraw any potential offending medication.
• Use antihistamines for pruritus
• Systemic corticosteroids can be used as a second-line treatment or in those with severe
disease
• Oral metronidazole has been used with limited success for chronic LP. The MOA however is
unknown
- Systemic retinoids are generally well tolerated and used in lower doses
- Phototherapy has also been used in some cases but there is photo-aggravated LP
Pityriasis rubra pilaris (PRP) is characterized by an acute cutaneous eruption that is often accompanied by pruritus and/or pain. Classic cutaneous lesions include ___ __ on an erythematous base coalescing to form large orange-red plaques but with characteristic ___ of sparing. PRP commonly begins on the ___ and rapidly spreads in a ____ direction and has the potential to quickly
Pityriasis rubra pilaris (PRP) is characterized by an acute cutaneous eruption that is often accompanied by pruritus and/or pain. Classic cutaneous lesions include follicular papules on an erythematous base coalescing to form large orange-red plaques but with characteristic islands of sparing. PRP commonly begins on the scalp and rapidly spreads in a craniocaudal direction and has the potential to quickly
key feature of pityriasis rubra pilaris
orange-red palmoplantar keratoderma and sparing of the mucous membranes.It is an uncommon condition and its main feature lies in its clinical resemblance to psoriasis.
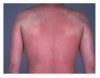
_____ is typically defined as diffuse redness of the skin affecting more than 90% of the body surface. The causes of erythroderma are manifold, and the more common causes include psoriasis, atopic dermatitis, idiopathic erythroderma, cutaneous T-cell lymphoma, and drugs. Drugs are the causative factor of erythroderma in 16% and 19% of cases as shown in 2 studies.
erythroderma
which drugs can cause erythroderma
allopuranol, dapsone, phenytoin, diltiazem, carbamazepine, ampilcillin, omeprazole, vanco

pityriasis rosea

herald patch- PR

herald patch: PR

LP

LP
which phenomena is occuring

linear koebner phenomena– LP plaques in repsonse to scratching/trauma

oral mucosal involvement of LP
this condition started at the base of the skull

PRP: acute cutaneous eruption accompanied by pain and pruritis. Erythematous Pap unless. Islands of sparing. Commonly starts on scalp, moving down (cranio-caudal). Very uncommon condiiton
pityriasis rubra pilaris

Orange red- Palma/plantar keratoderma and sparing of the mucus membranes. It is uncommon. Resembles psoriasis. Characteristic of PRP