MSK Infections Flashcards
osteomyelitis is an infection of bone characterized by ___ ___ desrtuction and __ of new bone.
Infection of
bone
characterized
by progressive
inflammatory
destruction and
apposition of
new bone
JAMA. 2008;299(7):858. doi:10.1001/jama.299.7.858

possible mycobacteria, spirochetes, and viruses that might contribute to an MSk infection

main routes of MSK spread
- hematogenous
- contigous through bone or bursa
- direc trhough sskin

risk factors of an MSK infection
- immunocompromised patients
- extremes of age
- systemic conditions (diabetes, rheumatoid arthritis, cirrhosis, HIV, chronic renal disase, malignancy)
- Obestiy
- Alcohol or tobacco abuse
- malnutrition
- medications– immunosuppressants like corticosteroids, DMARDS, biologics
- previous surgery
- vascular insufficiency
- peripheral neuropathy
empric vs definitive antibiotic therapy
empiric therappy is more broad spectrum
Pediatric osteomyelitis
most often due to
___seeding of bacteria to
___ region
- why is it more common in peds?
Pediatric osteomyelitis
most often due to
hematogenous
seeding of bacteria to
metaphyseal region
-More common in first
decade of life due to
rich metaphyseal
blood supply and
immature immune
system
pathology of osteomyelitis
slugglish blood flow in metaphyseal capillaries give bacteria to lodge in the region.
purulence develops in conjuction with
- osteoblast necrosis
- osteoclast activation
- release of inflammatory mediators and blood vessel thrombosis.

in kids, osteomyleitis happsn in long bones like the humerus, fibula, femur. it also occurs in hands and feet. what is the most common hematogenous site of adult osteomyelittis
most common in vertebrae. Spine and ribs in dialysis patients. sometimes in areas of injection for IV drug abusers.
maybe the foot regions due to ulvers caused by diabetes.
outline patient characteristics who might get these rare organisms as a joint infection
- salmonella
- pseudomonas
- bartonella
- fungal osteomyelitis
- tuberculosis

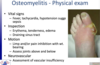
how is osteomyelitis classified?
based on timing: acute = wihtin 2 weeks, subacute, chornic
T/F You can xray all types of osteomyeltis
false. in acute osteomyelitis you won’t see x ray changes yet. bone changes evident 14-21 days after onset.
- there’s new periosteal bone formation, with osteolysis and formatoin of nidus.

what type of diagnostic imaging should you get if you suspect osteomyelitis
- bone scan (when xrays normal and MRI not an option. highly sensitive but not specific)
- WBC scan/gallium scan. performed in conjunction with bone scan 18-72 hours after. increases specifictiy
what types of lab investigations should you do if you suspect osteomyelitis
serum studies (WBC, CRP, ESR, blood culture)
microbiology (bone aspiration and bone biopsy)
non operative therapy for osteomyelitis
can be done in acute settings when the disease is early and there’s no evidence of subperiosteal abscess of abscess within bone. begin with empiric therapy and convert to organism speecific antibiotics if organism identified.
- typically treat with IV antibiotics for 4-6 weeks.
usually for chronic cases you need surgical debridement and possible amputation. or if theres a huge abscess forming. would need this in vonjunction with IV antibiotics.
common joint for septic arthritis in children
most commonlly involves the hip. primarily seeding of synovial membrane from infection in adjacent metaphyseal bone. also can affect the hosuler knee ankle and elbow.
most common joint for septic arthritis in adults
uslaly the knee in over 50% of the cases.
hip> shoulder> elbow> ankle> SC joint
Causes irreversible
cartilage destruction
– cartilage injury can occur
within 8 hours – caused by release of
proteolytic enzymes from
inflammatory cells
organism that can cause septic arthritis when bitten by a human
eikenella corrodens.
what Xray findings would indicate a septic arthritis
- joint space widening or evident effusion
- might see soft tissue swelling
- periarticular osteopenia
what other imaging modalities would you do for osmeone with septic arthritis in addition to XRAY
ultrasound
Mri

lab investigations for septic arthritis


this person might have conorrhea because a gram negative stain cocci formation is indicative of NG

management of septicarthritis
unlike osteomyelitis where early infections can be treated with Abx alone, SA IS CONSIDERED A SURGICAL EMERGENCY THAT REQUIRES URGENT SURGICAL I AND D AND IV ABX.
– Due to chondrolytic effect of pus – Need to remove damaging enzymes – Reduces intra-articular pressure decreases epiphseal
ischemia in hip
• IV ab therapy
– Initiate empiric therapy then transition to organism-
specific therapy based on sensitivities
what is the golden period of an open wound
the time after injury that wound can be closed without increasing risk of infection.







