Mini Symposium: Multi-system Autoimmune Disease Flashcards
(52 cards)
what are some Connective Tissue Diseases?
◦Systemic Lupus Erythematosus
◦Scleroderma
◦Sjogren’s syndrome
◦Auto-immune myositis
◦Mixed connective tissue disease
what are examples of Systemic vasculitis?
◦Giant cell arteritis
◦Granulomatosis polyangiitis (Wegeners)
◦Microscopic polyangiitis
◦Eosinophilic granulomatosis polyangiitis (Churg-Strauss)
how is a diagnosis made?
Cardinal clinical features: History & Exam
Bedside investigations
Immunology
Imaging
Tissue diagnosis
Exclusion of differential diagnosis
What are some mimics?
Drugs - cocaine, minocyline, PTU
Infection - HIV, endocarditis, Hepatitis, TB
Malignancy - lymphoma
Cardiac myxoma
Cholesterol emboli
Scurvey
what is Systemic lupus erythematosus?
Lupus is a condition that affects the immune system. It can cause problems with your skin, joints, kidneys and other organs
Systemic lupus erythematosus (SLE) – lupus – is a long-term condition causing inflammation to the joints, skin and other organs. There’s no cure, but symptoms can improve if treatment starts early
what is the epidemiology of SLE?
UK Prevalence: 28/100,000
UK incidence: 4/100,000
Female:Male 9:1
Onset: 15-50 years
Significant ethnic diversity:
Afro-Caribbeans>Asian>Caucasian
what is SLE aetiology?
Genetic factors – high concordance rate of SLE in monozygotic twins, Sibling risk of developing SLE is 30-fold higher than in the general population, polygenic mode of inheritance
Hormonal factors
Environmental factors – ultraviolet light, drugs, infections
what is SLE pathogenesis?
Immune response against endogenous nuclear antigens (break in immunological tolerance)
Immune complex formation
Complement activation
Tissue injury
where can SLE effect?
Clinical presentation is varied
Different organs that may be involved in lupus

what is the classification criteria? (any 4)
1) Malar rash (butterfly rash)
2) Discoid rash (raised, scarring, permanent marks, alopecia)
3) Photosensitivity
4) Oral ulcers
5) Arthritis (2 joints at least) - Non erosive, bilateral
6) Serositis (pleurisy or pericarditis)
7) Renal (significant proteinuria or cellular casts in urine)
8) Neurological (unexplained seizures or psychosis)
9) Haematological (low WCC, platelets, lymphocytes, haemolytic anaemia)
10) Immunological (anti ds-DNA, SM, cardiolipin, lupus anticoagulant, low complement)
11) ANA
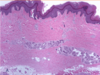
photos showing SLE: Skin manifestations
DDx butterfly: rosacea, mitral stenosis
Discoid: Scaly centre, dark rim
Malor rash and discoid rash

in someone with SLE what is one of the first things you should do?
urine analysis
use this to check renail involvement - make sure there isnt any
lupus nephritis

when would you consider a diagnosis of SLE?
Usually seen in women of child bearing age
Constitutional symptoms of fever, weight loss, malaise, severe fatigue
Skin rash and/or stomatitis
Arthritis
Pleuritic chest pain
Renal disease
cytopenia - Cytopenia occurs when one or more of your blood cell types is lower than it should be
what autoantibodies are involved in SLE?
ANA – antinuclear antibodies
Seen in 95% of SLE
Not specific for SLE
Seen in many inflammatory, infectious and neoplastic diseases
Seen in 5% to 15% of healthy population
what are ANA?
antinuclear antibodies (ANA)
our immune system normally makes antibodies to help you fight infection. In contrast, antinuclear antibodies often attack your body’s own tissues — specifically targeting each cell’s nucleus
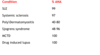
what are some Conditions where +ve ANA
is unhelpful?

in different condiitons what % of ANA is present?
what are osme other autoantibodies that many be seen in SLE?
Anti -ds DNA:
Seen in 60% of patients with SLE
Highly specific for SLE
Low titre rarely seen in other inflammatory conditions
Strongest clinical association is with nephritis
Anti -Sm (Smith):
Seen in 10% to 30% of SLE patients
Highly specific for SLE
Anti–Ro:
Risk of foetal congenital heart block
Neonatal lupus
Antiphospholipid antibodies:
Anti-cardiolipin, lupus anticoagulant
arterial/venous thrombosis
miscarriages
what is Systemic sclerosis?
Systemic scleroderma, or systemic sclerosis, is an autoimmune rheumatic disease characterised by excessive production and accumulation of collagen, called fibrosis, in the skin and internal organs and by injuries to small arteries
connective tissue disease characterised by fibrosis of the skin and internal organs
what are the different Classification of scleroderma?
Localised scleroderma
Systemic sclerosis (SSc):
- Limited cutaneous systemic sclerosis (CREST)
- Diffuse cutaneous systemic sclerosis
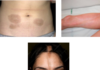
what si the difference between localised and systemic scleroderma?
Localised scleroderma (also known as morphoea or morphea) only affects the skin. In some cases it can spread to the tissues underneath the skin, such as muscles and bones. Systemic sclerosis affects the skin but may also involve the body’s internal organs
(pictures showing localised scleroderma)
what is the epidemiology of systmeic scleroderma?
UK Prevalence: 24/100,000
UK Incidence: 10/1,000,000
Onset: 30-50 years
Female : Male 3:1
what is the aetiology of systemic scleroderma?
Environmental:
- Silica
- Solvents
- Viral infections
Genetic predisposition
What is the pathogenesis of scleroderma?
Vascular damage (microcirculation)
Immune system activation/Inflammation
Fibrosis
















