Bone and Soft Tissue Tumours Flashcards
bone tumours can be what 2 types?
- Benign
- Malignant - primary or secondary
Primary – originate in bone
Secondary – originate elsewhere in the body and embolise to bone
soft tissue tumours can be of what 2 types?
- Benign
- Malignant
Bone tumours:
- benign tumours of skeleton ________
- malignant primary tumours of skeleton ____
- bony secondaries very _______
- bone tumour in patient >50y likely to be ________
common
RARE
common
metastatic
what is a sarcoma?
•Malignant tumours arising from connective tissues
where can a sarcoma spread?
- Spread along fascial planes
- Haematogenous spread to lungs
- Rarely to regional lymph nodes (except rhabdomyosarcomas, epithelioid sarcomas & synovial sarcomas)
what is the name for benign and malignant:
what is the name for benign and malignant:
Bone-forming tumours
benign: osteoid osteoma, osteoblastoma
malignant: osteosarcoma
what is the name for benign and malignant:
Cartilage-forming tumours
benign: enchondroma, osteochondroma
malignant: chondrosarcoma
what is the name for benign and malignant:
Fibrous tissue tumours
benign: fibroma
malignant: fibrosarcoma, malignant fibrous histiocytoma (MFH)
what is the name for benign and malignant:
Vascular tissue tumours
benign: haemangioma, aneurysmal bone cyst
malignant: angiosarcoma
what is the name for benign and malignant:
Adipose tissue tumours
benign: lipoma
malignant: liposarcoma
what is the name for benign and malignant:
marrow tissue tumours
malignant: Ewing’s sarcoma, lymphoma, myeloma
what is the name of some other tumours?
Benign, are locally destructive and can rarely metastasise - Giant Cell tumours (GCT)
what are some tumour like lesions?
benign: simple bone cyst, fibrous cortical defect
what is the Incidence of primary bone tumours in UK (per million population per year)?
Osteosarcoma - 3 per million popu./yr
Chondrosarcoma - 2 ..
Ewing’s tumour - 1.5 ..
Malig. fibrous histiocytoma - <1 ..
what is the commonest primary malignant bone tumour in younger patient?
Osteosarcoma
what is the commonest primary malignant “bone” tumour in older patient?
Myeloma
what would be seen in a history?
- Pain
- mass
- Abnormal x-rays - incidental
- Bone Tumours - PAIN
what may the pain be like in a bone tumour?
- Activity related
- progressive pain at rest & night
must take pain seriously
• Benign tumours may present with activity related pain if large enough to weaken bone e.g.Osteoid Osteoma
what should be examied in a presenting patient?
- General health
- measurements of mass
- location
- shape
- consistency
- mobility
- tenderness
- local temperature
- neuro-vascular deficits
you should be aware of swelling which is what?
- Rapidly growing
- Hard, fixed, craggy surface, indistinct margins
- Non-tender to palpation, but assoc. with deep ache, esp. worse at night
- BEWARE – may be painless
- Recurred after previous excision
= NASTY - suspicious of malignant tumour (primary or secondary) until proven otherwise
what investigation are we going to do?
- Plain x-rays - most useful for bone lesions
- Calcification - synovial sarcoma
- Myositis ossificans
- Phleboliths in haemangioma
what may an x-ray of a benign tumour look like?
Inactive
- clear margins
- surrounding rim of reactive bone
- cortical expansion can occur with aggressive benign lesions
how may an x-ray of an aggressive tumour appear?
- less well defined zone of transition between lesion and normal bone (permeative growth)
- cortical destruction = malignancy
- Periosteal reactive new bone growth occurs when the lesion destroys the cortex
- Codman’s triangle, onion-skinning or sunburst pattern
what may a CT be used for?
- Assessing ossification and calcification
- integrity of cortex
- best for assessing nidus in osteoid osteoma (good for assessing these tiny tumorus for surgery and treatment)
- Staging - primarily of lungs (involved CT scanning of the lungs)
what are Isotope Bone Scans used for?
- Staging for skeletal metastasis
- Multiple lesions - osteochondroma, enchondroma, fibrous dysplasia & histiocytosis
- Frequently negative in Myeloma
- Benign also demonstrate increased uptake
Big advantage in metastatic bone disease as in secondaries you can see how far or how many metastases there are

what is the investigation of choice?
MRI
what can a MRI be used for?
- size, extent, anatomical relationships (how far it has spread, e.g. in soft tissue as x-ray doesnt show soft tissue)
- Accurate for limits of disease both within and outside bone
- Specific for Lipoma, haemangioma, haematoma or PVNS (can tell its these types)
Non-specific for benign vs. malignant (hard to tell which one it is)
what are some other investigations that my be used?
• Angiography:
superseeded by MRI
Psuedoaneurysms, A-V malformations
Embolisation of vascular tumours - Renal, ABC
•PET: may be useful for investigating response to chemo
what needs to be done before a biopsy?
- Bloods
- X-rays of affected Limb & Chest
- MRI of lesion
- Bone Scan
- CT Chest, abdo & pelvis
Benign vs. Malignant - how do you tell?
- History
- Clinical findings
- Radiological features
- Biopsy – needle core vs. Open
- Treatment
- Reconstruction
Benign picture – pain, rapid progression in size, night pain
Hard craggy masses = malignant
Malignant Primary Bone Tumours - what are the cardinal features?
- Increasing pain
- unexplained pain
- Deep-seated boring nature
- Night pain
- Difficulty weight-bearing
- Deep swelling
Case 1:
- 16 year old female episode of back pain
- Referred by GP for investigation as not resolving
- Referred by Orthopaedic surgeon for bone scan
- By time of bone scan pain pretty much resolved
- Uptake on bone scan in Left proximal humerus!
- Asymptomatic - Referred to Sarcoma MDT for opinion
Case 2:
- 32 year old male
- Closed # junction middle and distal 1/3 Left Tibia playing football
- Developed post tibial nailing anterior knee pain – incidence of which is 40-50%.
- Didn’t improve, in fact deteriorating. X-rays show # slow to heal
- Knee pain continues – arthroscopy
- Develops fixed flexion deformity of knee
- Alarm bells!
Case 3:
- 23 year old knee pain
- GP – simple remedies
- Failed to resolve
- Physio
- Pain increasing – x-ray – normal
- more physio – pain still increasing & swelling
- Alarm bells!
- X-ray - six months later!
Osteosarcoma
who and where do osteosarcomas mainly occur?
(malignant Bone-forming tumours)
Mainly male condition
Over 50% occur in the age group 10-30
Mainly in distal femur and proximal tibia

what are the Clinical features of a osteosarcoma?
- pain
- loss of function
- swelling - comes on later as the initial bone tumour wont be very large
- pathological fracture
- joint effusion
- deformity
- neurovascular effects (e.g. weight loss, loss of apetite)
- systemic effects of neoplasia
how does pain present in an osteosarcoma
cardinal feature
increasing pain - impending #fracture (esp. lower limb)
analgesics eventually ineffective
not related to exercise
DEEP BORING ACHE, WORSE AT NIGHT = !!
how does loss of function present in an osteosarcoma
limp
reduced joint movement
stiff back (esp. child)
how does swelling (“tumour”) present in a osteoscarcoma?
generally diffuse in malignancy
generally near end of long bone
once reaching noticeable size, enlargement may be rapid
warmth over swelling + venous congestion = active!
pressure effects e.g. intrapelvic (pressure on surrounding structures e.g. bowel, bladder. seen particulary in intrapelvic tumours)
how does a pathological fracture present in a osteosarcoma?
A pathologic fracture is a broken bone that’s caused by a disease, rather than an injury. Some conditions weaken your bones, which makes them more likely to break. Everyday things, such as coughing, stepping out of a car, or bending over can fracture a bone that’s been weakened by an illness
n.b. many causes, of which primary bone tumour (benign or malignant) is one of rarest, c.f. osteoporosis commonest (usually in osteoprosis bone)
minimal trauma + history of pain prior to fracture !!
MRI is the investigation of choice for (osteosarcomas)- very sensitive
what is it very good for showing?
- intraosseous (intramedullary) extent of tumour
- extraosseous soft tissue extent of tumour
- joint involvement
- skip metastases
- epiphyseal extension
- determines resection margins - surgeons what to take the tumour out along side a piece of bone and leave a functioning limb so this tells them if it is possible or not
what is the treatment of an osteosarcoma
- Goal is to make free of disease
- Chemotherapy - shrink the tumour
- Surgery
- Radiotherapy
- TEAM !!
What surgery is performed?
- Limb salvage possible for most cases
- Consider involvement of neurovascular structures
- pathological #fractures
- poorly performed biopsy - If make biopsy on wrong place then it can spread along that biopsy line and may make it imposible for limb salavge surgery
how common is metastatic bone disease?
- 2° bone tumour 25 x commoner than 1°
- bone most common site for 2° after lung and liver
- great differences between tumours and sites of metastases - e.g. breast commonly goes to bone (50 breast : 9 melanoma), melanoma commonly goes to lung (40 melanoma : 12 breast)
how many people get Metastatic Bone Disease?
- incidence of skeletal 2°’s usually underestimated +++
- Approx 9000 women with Breast Ca develop 2°’s each year
- All cancers - 20 000 new cases 2°’s each year
name the sites in order of frequency (for all 2°’s)
vertebrae > proximal femur > pelvis > ribs > sternum > skull
what is the 7 commonest primary cancers which metastasise to bone?
- LUNG - smoker; CXR, sputum cytology
- BREAST - commonest; examine!
- PROSTATE - osteosclerotic 2°; PR, PSA
- KIDNEY - solitary, vascular; IVP + US, angiography & embolise
- THYROID - esp. follicular Ca; examine
- GI TRACT - FOB, endoscopy, Ba studies, markers
- MELANOMA - examine!
[neuroblastoma (of adrenal medulla) - aet. <4 y]
what is survival like after a pathological fracture?
- survival after pathological fracture depends on type of tumour -e.g. bronchial Ca. <= 1 y
- in breast - median survival with bone metastases hugely increased; with soft tissue metastases is 12-24 months
- in general, approx. 50% of patients with pathological fractures will survive >6 m, & 30% >=1 y
how is prevention of a pathological fracture done?
- early chemotherapy / DXT
- prophylactic internal fixation - lytic lesion + increasing pain &/or ³ 2.5 cm diam &/or ³ 50% cortical destruction (Fidler M 1973 Br Med J 1: 341-3); better with Mirel’s Scoring System
- ± use of bone cement (not signif. affected by DXT)
- embolisation esp. renal, thyroid - wait 48h before surgery
- only one long bone at a time
- aim for early painless weight-bearing + mobilisation
- fracture of non-WB skeleton (e.g. humerus) can be treated conservatively, but re-fracture freq.
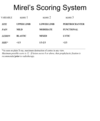
Fracture Risk Assessment - what is Mirel’s Scoring System?
This is how we decide how to fix one
If 8 or above then prophylactic fixation and then radiotherapy
Radiotherapy will kill off tumour at site but if no prophylaxis then the radiotherapy will fracture before you fix them
Metastatic Bone Disease: Key Points
(BOA Working Party)
- The prognosis for Patients with Metastatic Bone Disease (MBD) is steadily improving. Many patients will survive three or more years.
- Never assume that a lytic lesion, particularly if solitary, is a metastasis.
- Metastatic pathological fractures rarely unite, even if stabilized.
- Prophylactic fixation of long bone mets is generally easier for the surgeon and less traumatic for the patient.
- Use the Mirels scoring system.
- Fixation of pathological fractures or lytic lesions, especially around the hip/proximal femur have a high failure rate. Cemented hip prostheses (either standard or tumour prostheses) have a low failure rate.
- Never rush to fix a pathological fracture. Traction or splintage will suffice while investigations are performed and surgical intervention discussed with the lead clinician for MBD and other appropriate colleagues.
- When surgery is indicated for spinal metastases, both decompression and stabilisation are generally required.
- Constructs, whether spinal or appendicular, should allow immediate weightbearing and aim to last the lifetime of the patient.
- Solitary renal metastases should, where possible, be radically excised.
- Each trauma group requires a lead clinician for MBD.
- Treatment should be within the context of a multi-disciplinary team.
Summary - Bone:
what kind of pain is it?
where is a mass?
what investigation?
- Pain - persistent, increasing, non-mechanical/rest, nocturnal
- Deep seated mass (vague)
- X-rays
what is the commonest soft tissue tumour?
lipoma
what is the solitary Lipoma : sarcoma ratio?
<5cm 150:1 for sarcoma
>5cm 20:1
>10cm 6:1
Deep seated tumours 4:1
(80% of deep sarcomas are > 5 cm)
Bigger it is more chance it is sarcoma (malignant)
If swelling is large and deep sated then think sarcoma
what are the features of Soft-tissue tumours?
- painless
- mass deep to deep fascia
- any mass >5cm
- any fixed, hard or indurated mass
- any recurrent mass
what imaging study is done for soft tissue tumours?
MRI
Soft tissue tumours:
- all patients with a soft tissue tumour suspected of being _______ should be referred to a specialist Tumour Centre
- suspicious signs are:
- ____ (i.e. deep to deep fascia) tumours of any size
- subcutaneous tumours > _ cm
- rapid growth, ____, ______, non-tender
malignant
deep
5
hard
craggy


