Commonly encountered rheumatic diseases: crystal arthropathies & polymyalgia rheumatica Flashcards
what are common crystal deposition diseases?
•Characterised by deposition of mineralised material within joints and peri-articular tissue
COMMON
- Monosodium urate deposition - responsible for gout
- Calcium pyrophosphate dihydrate (CPPD) - Pseudogout
- Basic calcium phosphate hydroxy-apatite (BCP) deposition – causes calcific periarthritis/tendonitis
how does Purine metabolism occur?
Endogenous production of uric acid from degradation of purines usually contributes about two-thirds of the body urate pool, the remainder being dietary in origin
Of the uric acid produced daily, the majority (∼ 70%) is excreted via the kidney and the remainder is eliminated into the biliary tract and subsequently converted by colonic bacterial uricase to allantoin
In the vast majority of people with gout, hyperuricaemia results from reduced efficiency of renal urate clearance

what 2 ways if Hyperuricaemia caused?
(Hyperuricemia is an excess of uric acid in the blood. Uric acid passes through the liver, and enters your bloodstream. Most of it is excreted (removed from your body) in your urine, or passes through your intestines to regulate “normal” levels)
overproduction
under excretion
what ways may hyperuricaemia be caused by overproduction?
- Malignancy e.g lymphoproliferative, tumour lysis syndrome (high cell turnover and breakdown - Uric acid comes form purine break dow)
- Severe exfoliative psoriasis
- Drugs e.g. ethanol, cytotoxic drugs
- Inborn errors of metabolism
- HGPRT deficiency
what ways may hyperuricaemia be caused by under excretion? (most common)
- Renal impairment
- Hypertension
- Hypothyroidism
- Drugs e.g. alcohol, low dose aspirin, diuretics, cyclosporin
- Exercise, starvation, dehydration
- Lead poisoning
how does alcohol cause hyperuricaemia?
Some alcoholic drinks are rich in purines, notably beer which contains guanosine. Alcohol is thought to increase the risk of gout because the metabolism of ethanol to acetyl CoA leads to adenine nucleotide degradation, resulting in increased formation of adenosine monophosphate, a precursor of uric acid. Alcohol also raises the lactic acid level in blood, which inhibits uric acid excretion
Alcohol can cause it and goes with overproduction and under excretion
what is Lesch Nyan Syndrome?
deficiency of the enzyme hypoxanthine-guanine phosphoribosyl transferase (HPRT). Hypoxanthine-guanine phosphoribosyl transferase (HPRT) normally plays a key role in the recycling of the purine bases, hypoxanthine and guanine, into the purine nucleotide pools
In the absence of HPRT, these purine bases cannot be salvaged; instead, they are degraded and excreted as uric acid. In addition to the failure of purine recycling, the synthetic rate for purines is accelerated, presumably to compensate for purines lost by the failure of the salvage process. The failure of recycling together with the increased synthesis of purines is the basis for the overproduction of uric acid
• X-linked recessive

what are the effects of Lesch Nyan Syndrome?
- intellectual disability
- aggressive and impulsive behaviour
- self mutilation
- gout
- renal disease
what is the prevalence of gout like in the UK?
Prevalence of gout in the UK, showing that it is predominantly a disease of older men
Men have higher urate levels than women and an increased prevalence of gout at all ages, though less pronounced in older age
Oestrogen has a uricosuric effect, making gout very rare in younger women. However, after the menopause, urate levels rise and gout becomes increasingly prevalent
Ageing is an important risk factor in both men and women, possibly due to multiple factors including:
an increase in sUA levels (mainly due to reduced renal function);
increased use of diuretics and other drugs that raise sUA;
age-related changes in connective tissues, which may encourage crystal formation;
and an increased prevalence of OA

how is a Diagnosis of Gout made?
- History
- Examination
- Differential Diagnosis
- Investigations
what are some risk factors of gout?
Over weight
Rich in meat and seafood diet
Alcohol excess
people on diuretics
Dehydration
how does gout present?
Classically occur in the first MTP joint
Usually start over night
Short history
Very painful
5-7 days before settles down
Red hot, shiny skin

what is hsown here in this perosn with gout?

Can lose overlying skin
Chalky white material – may get discharge of it
what is shown here?
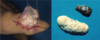
TOPHUS - TOPHI
Massive accumulations of uric acid
Seen over bony surfaces

what is the gold standard way to investigate gout?
Investigate – gold stand is to Aspirate joint and look for crystals
Also aspirate for differential diagnosis of sepsis as hard to tell clinically
Often seen in MTP so if its there don’t often aspirate to confirm diagnosis of gout if it is there

what is shown here?

gout crystals
Send away form microscopy and culture to make sure not missing infection
what is the 2 different stages involved in the management of gout?
acute flare
hyperuricaemia
how do you manage the acute flare in gout?
- NSAIDs (first line)
- Colchicine
- Steroids - I/A, I/M, oral
how do you manage hyperuricaemia in gout? (longer term)
- Does it need to be treated ?
- 1st attack not treated unless; Single attack of polyarticular gout, Tophaceous gout, Urate calculi, Renal insufficiency
- Treat if 2nd attack within 1 yr
- Prophylactically prior to treating certain malignancies
- DO NOT treat asymptomatic hyperuricaemia
what is used in the Lowering of uric acid?
- Xanthine oxidase inhibitor e.g. Allopurinol (most commonly used)
- Febuxostat
- Uricosuric agents e.g. sulphinpyrazone, probenecid, benzbromarone (enhance urinary excretion of urinary acid)
- Canakinumab
(Allopurinol and Febuxostat act at blue arrows)

What are the rules for lowering uric acid levels?
- Wait until the acute attack has settled before attempting to reduce the urate level
- Use prophylactic NSAIDs or low dose colchicine/steroids until urate level normal
- Adjust allopurinol dose according to renal function
what other factors do you need to assess?
Address cardiovascular and lifestyle factors
Assess weight, BP, alcohol, smoking and diet
How is pseudogout like gout?
•The knee is to pseudogout as the toe is to gout
First MTP is commonly affected in gout
Knee is most common joint effected in pseudogout
what is pseudo gout?
Pseudogout (or “false gout”) is a form of arthritis that results from deposits of calcium pyrophosphate crystals, hence its new name of calcium Calcium pyrophosphate dihydrate crystal deposition disease or CPPD. It commonly affects the knees and wrists.
who and how does pseudogout normally effect?
- Elderly females
- Erratic flares
what is the aetiology of pseudogout?
Idiopathic, familial, metabolic
what are the triggers of pseudogout?
Trauma, Intercurrent illness
what cn be seen on xray of someone with pseudogout?
Chondrocalcinosis
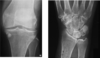
if you were to aspirate a joint is pseudo gout and look at it under a microscope what would you see?
Pyrophosphate crystals

what is the management of pseudogout?
- NSAIDs
- I/A steroids
- There are no prophylactic therapies (as there are for gout)
Often following infection so important to exclude septic joint so important to aspirate
Treating trigger and symptomatically
what is Polymyalgia Rheumatica?
Inflammatory condition of the elderly. There is a close relationship wth GCA (most common of the systemic vasculitides characterised by involvement of the large vessels). Not going to discuss GCA – covered in later lecture
Polymyalgia rheumatica (PMR) is a condition that causes pain, stiffness and inflammation in the muscles around the shoulders, neck and hips
who does polymyalgia rheumatic occur in?
Very common in community
Close relationship with giant cell arteritis
elderly
how is polymyalgia rheumatica rleated to giant cell arteritis?
20% of patients with PMR may have evidence of GCA
50% of patients with GCA may have PMR

how does Polymyalgia Rheumatica present?
- SUDDEN onset of shoulder +/- pelvic girdle STIFFNESS
- ESR usually > 45 often 100
- Anaemia
- Malaise ; Weight loss ; fever; depression
- Arthralgia / synovitis occasionally
who does Polymyalgia Rheumatica occur in?
- Rare < 50y usually > 70y
- F:M 2:1
how is the diagnosis of polymyalgia rheumatica made?
- Compatible history
- Age > 50
- ESR > 50
- Dramatic steroid response
- No specific diagnostic test
what are some Differential diagnosis of polymyalgia rheumatica?
- Myalgic onset Inflammatory joint disease
- Underlying malignancy - e.g Multiple myeloma, lung cancer
- Inflammatory muscle disease
- Hypo/hyperthyroidism
- Bilateral shoulder capsulitis
- Fibromyalgia (wouldn’t expect an inflammatory response, so not a raised ESR, CRP or anemia)
Really important you ask about temporal artery
what is the treatment of polymyalgia rheumatica?
- Prednisolone 15mg per day initially
- 18-24 mth course
- Bone prophylaxis
Summary:
- Aware of the different crystal deposition diseases and their presentation
- Basic understanding of why hyperuricaemia may occur
- Know how to manage an acute attack of gout
- Know how to manage hyperuricaemia
- Recognise the signs and symptoms of Polymyalgia Rheumatica


