Week 3 - D - Physiology of pregnancy and lactation (placenta,hormones, matneral, nutrition, lactation) Flashcards
Where does the egg meet the sperm? What is this known as?
Fertilization occurs in the ampulla of the Fallopian Tube. This is known as fertilisation
What does the zygote formed from fertilisation of the egg divide into to become the blastocyst? How many cells is this structure? What day is this structure formed by?
The zygote divides to become the morula - this is a 8-16 cell stage at around day 3/4 after ovulation

What are the five major stages of embryonic development?
Gametogenesis Fertilisation Cleavage Gastrulation - formation of the germ layers Organogenesis
What day is the blastocyst formed by? When is the earlies possible day of implantation? What is normally the day of implantation of the fertilised egg?
The blastocyst should be formed by day 5/6 after ovulation Earliest possible day of implantation is day 6 (hence why copper coil can be used for up to 5 days after the earliest expected date of ovulation - unethical to kill the implanted foetus)
After implantation, if you look into the uterine cavity, can you see the blastocyst ? Once the egg is ovulated, what sweep it into the oviduct?
The egg is swept into the oviduct by the fimbriae - the fimbraie surround the ostium of the fallopian tube
The blasocyst has an outer cell structure known as the trophoblast and an inner cell mass What is the inner cell mas known as and what does it go on to develop? What does the outer cell mass go on to develop?
The inner cell mass known as the embryoblast goes on to develop the embryo
The outer cell mass known as the trophoblast burrows into the endometrium and becomes the placenta

The trophoblast has two layers - the cytotrophoblast and the syncytiotrophoblast
- Which is the inner layer?
- Which is the outer layer which actively invades the endometrium?
Which layer produces b-HCG and progesterone?
The inner layer of the trophoblast is the cytotrophoblast
The outer layer that invades the endometrium and produces b-HCG and prgesterone (which maintains the endometrium lining) is known as the syncytiotrophoblast

* When the free-floating blastocyst adheres to the endometrial lining, cords of trophoblastic cells begin to penetrate the endometrium. * Advancing cords of trophoblastic cells tunnel deeper into endometrium, carving out a hole for the blastocyst. The boundaries between cells in the advancing trophoblastic tissue disintegrate.
What is the sac which covers the baby known as?
The amnion - covers the embryo The chorion covers the embryo+placenta (foetal portion of placenta is known as the chorion sometimes)
When implantation is finished the blastocyst is completely buried in the endometrium By what day will the blastocyst be fully embedded in the endometrial wall? What are the structures that sprout from the chorion to provide maximum contact area with maternal blood known as?
The blastocyst will be fully embedded in the endometrial wall by day 12 after ovulation Chorionic villi sprout from the chorion to provide maximum contact area with maternal blood
* Placenta is formed from embryo – True or false? * Placenta helps in nutrition of the growing embryo from fertilisation - True or false? * Placenta is fetal heart - True or false?
* Placenta is formed from the embryo - false as it is formed from both the embryo and the mother * Placenta helps in nutrition of the growing embryo from fertilisation - false as it is the yolk sac that in the early weeks of pregnancy, the embryo is attached to a tiny yolk sac that provides nourishment. A few weeks later, the placenta will be fully formed and will take over the transfer of nutrients to the embryo. * Placental is foetal heart - false it is foetal lung
Placenta is formed from both trophoblast cells and decidual cells What are decidual cells? What are the trophoblastic cells that differentiate into multinucleate cells and invade the the decidua to break down cavites and form capillaries that fill with maternal blood?
The decidual cells are the uterine cells of the endometrium which form the maternal part of the placenta The syncytiotrophoblasts invade the decidua and form the foetal part of the placenta
Developing embryo sends capillaries into the syncytiotrophoblast projections to form “placental villi” Each villus contains foetal capillaries separated from maternal blood by a thin layer of tissue – no direct contact between foetal & maternal blood What is the foetal part of the placenta known as? What is the placental part of the placenta known as?
Foetal part of the placenta is known as the chorion Placental part is known as the decidua basalis
What is the structure that separates the foetal blood and maternal blood known as?
Placental membrane or barrier
2 way exchange of respiratory gases, nutrients, metabolites etc between mother and foetus, largely down diffusion gradient By what week of pregnancy are the placenta (and foetal heart) functional? (not complete but functional)
They are functional by the 5th week of pregnancy
- * Early nutrition of the embryo is due to - invasion of trophoblastic cells into the decidua
- * Human chorionic gonadotropin (HCG) signals the corpus luteum to continue secreting progesterone stimulates decidual cells to concentrate glycogen, proteins and lipids
- * Blood vessels from embryo develop in the villi. A thin membrane separates the embryo’s blood in villi from mother’s blood in the intervillous space
How is the circulation in the intervillous space described?
It is described as an arteriovenous shunt - takes the deoxygenated blood from the foetus and provides the foetus with oxygenated blood from the placenta
The placenta plays the role of the “Fetal Lungs” The respiratory function of the placenta makes supply of oxygen and removal of carbon dioxide possible. The exchange takes place between maternal (oxygen-rich) blood and the umbilical blood (mixing of arterial and venous blood, oxygen-poor).
What carries the oxygenated blood from placenta to growing foetus?
The umbilical vein carries the oxygen rich blood of the mother from placenta to foetus

What are the veins that carry the deoxygenated blood back from foetus to mother?
These are the uterine veins
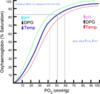
The supply of the fetus with oxygen is facilitated by three factors:
- Foetal Hb
- Higher Hb
- Bohr effect
Describe all three?
At normal partial pressures of oxygen - higher % of oxyhaemoglobin in foetus than in adult

- Foetal Hb has a higher affinity for oxygen than adult haemoglobin
- There is an increased haemoglobin concentration in the foetus (50%more than in adults)
- Bohr effect - foetal haemoglobin can carry more oxygen in low CO2 levels than in high CO2 levels (shifts oxygen dissociation curve to the left) (for some reason lecturer put this in - this is legit the haldane effect)
Why is it that foetal haemoglobin has a higher affinity for oxygen than adult haemglobin?
- Foetal haemoglobin - 2alpha subunits, 2 beta subunits
- Adult haemglogbin - 2alpha subunits, 2 beta subunits
The γ subunit has fewer positive charges than the (adult) β subunit, 2,3-BPG is less electrostatically bound to fetal hemoglobin compared to adult hemoglobin.- this shifts oxygen disocciate curve to the left as foetal haemoglobin therefore has a higher affintiy (2,3-BPG basically non-competitively inhibits oxygen on beta subunits)
The placental exchange processes occur via classic membranous transport mechanisms: Passive transport (without energy consumption) Simple diffusion Osmosis Simplified transport (facilitated transport) Active transport Electrolytes follow water via osmotic gradient Which two electrolytes can only go from mother to child?
Iron and Ca2+ can only go from mother to child irrespective of the osmotic gradient
How does glucose cross the placenta? It is the foetus’ main source of energy
Glucose crosses the placenta via facilitated transport - ie it is freely diffusible

drugs can also cross the placental barrier - teratogens: They account for 3% of all congenital malformations not including alcohol Name 4 drugs which can cross?
Heroine, nicotine, caffeine, carbamezapine, sodium valproate, ACEandARBs
A pregnant women is in the following state – T/F? Diabetic? Coagulopathic? Hyperparathyroid? Hyperthyroid? Hyper motility in gut Hyper oestrogenic? Hyper progestrogenic?
Diabetic - True Coagulopathic - True Hyperparathyroid - True Hyperthyroid - True Hyper motility in the gut - True Hyper oestrogenic - True Hyper progestogenic - True
What does the corpus luteum become if fertilisation doesnt occur? What hormone produced by the placenta prevents this? What does the corpus luteum prodcue?
If fertilisation doesnt occur the coprus luteum (yellow) will become the corpus albicans beta-human chorionic gonadotrophin prevents the involution of the coprus luteum and therefore the corpus luteum continues to produce progesterone (and oestrogen) which maintains the endometrium









