Visual Defects Flashcards
(119 cards)
What is the ‘lens’? What structures is it suspended by? What muscles is it connected to?
- A transparent structure
- Suspended by ligaments (zonule fibres) attached to the ciliary muscles which control the shape of the lens.

What is the vitreous humour? Function?
Viscous, jelly-like substance that lies between the lens and the retina. Keeps the eye spherical.

Which part of the eye keeps it spherical?
Vitreous humour
Which part of the eye is light transformed into neural activity?
Retina
Which part of the eye is the point of highest visual acuity? Why?
Fovea - in the line of the visual axis where light can reach the photoreceptors directly
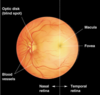
OPHTHALMOSCOPIC VIEW OF RETINA
Macula: central vision, colour vision
Fovea: central/ thinner region of retina
Optic disc: origin of blood vessels, where the optic nerve axons exit the eye (blind spot)
Which part of the eye is responsible for colour vision?
Macula
How is light focused onto the retina?
Refraction by the cornea (and lens) - then passes through the vitreous humour to the retina
What are the 2 layers of the retina?
An outer pigmented layer called the pigment epithelium, which adheres to the choroid, and an inner layer of nerve tissue called the sensory (or neural) retina.
What are the cells in the pigment epithelium of the retina filled with? Purpose of this?
Cells in the pigment epithelium are filled with melanin which absorbs light which isn’t passed on to photoreceptors (stops damage).
What composes the neural layer of the retina?
Photoreceptors, bipolar cells, ganglion cells etc
What is the other function of the pigment of the retina?
Pigment also provides nutrients which are required for photoreceptors to work properly
Light passes through all the other retinal cells to reach the photoreceptors at the back of the retina. Then describe the order which light passes between cells
- Photoreceptors: receive photons
-
Retinal biopolar cells: connect photoreceptors and ganglion cells
- Receive signals from photoreceptors and excite ganglion cells but releasing glutamate onto the dendrites of ganglion cells
- Ganglion cells: receive signal from bipolar cells, axons form the optic nerve
BUT 2 inhibitory neurons are involved:
- Horizontal cells: inhibitory neurons in the outer retina which help integrate and regulate the input from photoreceptors, also help adapt retina to different light levels
- Amacrine cells: inhibitory neurons in the inner retina which
- modulate transmission from bipolar cells to ganglion cells (form synapses onto the synaptic terminal of the bipolar cells as well as onto the dendrites of ganglion cells)

What 2 interneurons (inhibitory neurons) are found in the retina?
- Horizontal cells
- Amacrine cells
Which neurotransmitter does biopolar cells release?
Glutamate (excitatory)
What is phototransduction?
Conversion of light energy into an electrical signal (how information is moved along neurons).
Where does phototransduction occur?
Outer segments of photoreceptors are filled with lots of membranous discs – this is where phototransduction happens.

Cones vs rods;
a) sensitivity
b) light level
c) number
d) photopigment
e) acuity
f) convergence
Rods:
a) Very sensitive to light, can pick up scattered rays
b) low light, nighttime
c) 20x more common
d) High photopigment so can capture more light
e) low acuity
f) High level of convergence
Cones:
a) Not sensitive to light, must have direct ray
b) Day time, bright light
c) uncommon
d) Low photopigment so captures less light
e) high acuity
f) Lower level of convergence: one per ganglion in macula

Where are rods found? Where are cones found?
Rods: All over the retina except the fovea
Cones: Most dense at the fovea and macula
In the dark, are photoreceptors depolarised or repolarised? Describe their glutamate release
In the dark photoreceptors are depolarised (to around -30 mV) and continuously release glutamate
In the light, are photoreceptors depolarised or repolarised? Describe their glutamate release
Light causes these photorecptors to repolarise/hyperpolarise (as depolarising ion channels close) and decrease their glutamate release.
What are membranous discs of photoreceptors packed full of?
Photopigments
What are photopigments?
Each photopigments is a single transmembrane protein (G-protein coupled receptors) –> ‘opsin’ proteins
What are the photopigments called in rods?
Rhodopsin









