Hip Fracture Flashcards
(43 cards)
Why is hip fracture such a significant injury?
it is the most common injury in elderly people and the commonest reason they will need to undergo emergency surgery
What are the mortality risks associated with hip fracture?
10% within 1 month
30% within 1 year
most deaths are not due to the fracture itself, but due to underlying comorbidities
What is the definition of a hip fracture?
fracture of the femur distal to the femoral head and proximal to a level 5cm below the lesser trochanter
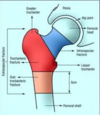
Label the components of the pelvis and femur


What is the definition of the hip joint?
a multi-axial ball and socket joint between the femoral head and the acetabulum
What helps to stabilise the hip joint?
muscles and ligaments
Label the muscles and the ligaments around the hip joint


What is the role of the femoral neck?
it connects the femoral head to the proximal femoral shaft and attaches to the intertrochanteric region
What is the main function of the greater and lesser trochanters?
they are sites for muscle attachment
what is the blood supply to the hip joint?
What can happen if it is disrupted?
medial and lateral circumflex femoral arteries
disruption of the blood supply to the head and neck of the femur can impair fracture healing
this can lead to avascular necrosis
What nerves are present in the hip region?
- femoral nerve
- obturator nerve
- superior gluteal nerve
- nerve to quadratus femoris
How can hip fractures be classified?
Intracapsular:
this is within the joint at the level of the neck of the femur
Extracapsular:
this is below the neck of the femur (outside the hip capsule)
this can be intertrochanteric or subtrochanteric

In which 4 situations is a hip fracture suspected?
- in the elderly
- falls
- high mechanism trauma - tends to be in younger patients
- osteoporosis
What is the mechanism of injury of hip fracture during a fall?
- falling directly onto the lateral hip
- a twisting action when falling
- a sudden spontaneous fracture which causes a fall (insufficiency fracture)
What is an insufficiency fracture?
severe osteoporosis causes the bone to spontaneously break
this then causes a fall
underlying bone metastases in bone cancer can also cause spontaenous fractures
Why is it important to determine the cause of why someone might have fell?
the occurrence of falls and fractures often signal underlying ill health
the underlying cause needs to be identified and treated
What are the 5 areas that must be covered when taking a history of a fall/hip fracture?
- mechanism of injury - before, during and after the fall
- collateral history - this is a history from another person if the elderly person cannot recount it themselves
- past medical and surgical history
- medication history
- social history
Why is a medication history important in elderly patients who have fallen?
polypharmacy (being on more than 4 tablets) increases risk of falls
if patients are on anticoagulants, the effect needs to be reversed before the patient has surgery
What are the 6 risk factors when diagnosing hip fractures?
- reduced bone density in osteopenia or osteoporosis
- age over 65 years
- falls
- low BMI
- female gender
- high energy trauma in patients 40 years or younger
What are the 4 diagnostic factors in hip fracture?
- inability to weight bear due to pain
- pain in affected leg/hip
- pain with hip movement
- shortened and externally rotated leg
Where is pain generally felt in a hip fracture?
around the region of the greater trochanter
it can radiate distally into the knee
What are the 3 stages in examination of the hip?
- look
- feel
- move
Before examining a patient, what 6 stages should be carried out?
- introduce yourself
- confirm patients details
- explain examination
- check understanding and gain consent
- hand gel/wash hands
- expose patient appropriately






