Hematology Oncology II Flashcards
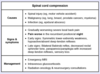
What is the initial step in management for a patient with suspected epidural spinal cord compression?
IV glucocorticoids
glucocorticoids should be administered before MRI

What is the likely diagnosis in a chronic smoker that presents with dyspnea, weight loss, and face/arm swelling that is worst in the morning?
SVC syndrome
malignancy is the most common cause (often lung cancer and non-Hodgkin lymphoma); may also occur due to fibrosing mediastinitis or thrombosis from indwelling central venous catheters

What is the likely diagnosis in a middle-aged patient with pancytopenia and splenomegaly without lymphadenopathy and the peripheral smear below?

Hairy cell leukemia

What is the likely diagnosis in a patient that develops a fever, chills, and malaise two hours after starting RBC tranfusion? Coombs test is negative.
Febrile non-hemolytic transfusion reaction
due to cytokines released by residual leukocytes; the direct antiglobulin test is positive and plasma free hemoglobin is > 25 mg/dL in acute hemolytic reactions

What is the likely diagnosis in a patient that develops fever/chills, flank pain, hemoglobinuria, and DIC 30 minutes after starting RBC tranfusion?
Acute hemolytic transfusion reaction
hemoglobinuria is a helpful clue that you’re dealing with an acute hemolytic transfusion rather than an allergic reaction

What is the likely diagnosis in a patient that develops wheezing, respiratory distress, and hypotension minutes after reciving a pRBC transfusion?
Anaphylactic reaction
more common in individuals with IgA deficiency

What is the likely diagnosis in a patient that presents 5 days post-CABG with large purple-black patches surrounded by erythema in the periumbilical area by sites of heparin injection?
Type 2 heparin-induced thrombocytopenia (HIT)
HIT should be suspected if there is a drop in platelets by > 50% or a new thrombus within 5-10 days of heparin initiation (may occur earlier in patients previously exposed to heparin)

What is the likely diagnosis in a patient that received a bone marrow transplantation from a sibling that develops a maculopapular rash, bloody diarrhea, and elevated LFTs after two weeks?
Graft-versus-host disease (GVHD)
due to recognition of host HLA-antigens by donor T-cells; typically affects the skin, intestine, and liver
What is the likely diagnosis in a patient with a facial rash that worsens with sun exposure and a history of DVT and 2 miscarriages?
Anti-phospholipid syndrome
more common in patients with SLE but can occur on its own; diagnosis requires clinical symptoms and presence of an antibody (e.g. antiphospholipid, anticardiolipin, or beta-2 glycoprotein-1 antibody)

What is the likely diagnosis in a patient with a history of prostate cancer that presents with severe back pain, decreased lower extremity DTRs, and urinary retention?
Epidural spinal cord compression
What is the likely diagnosis in a patient with a signficant smoking history that presents with daytime headaches, dizziness, and nausea? CBC reveals elevated hemoglobin levels. The patient works in a parking garage.
Carbon monoxide poisoning
chronic tissue hypoxia stimulates the kidney to produce more EPO, resulting in secondary polycythemia

What is the likely diagnosis in a patient with abdominal pain, dark urine, and hepatic vein thrombosis with evidence of hemolytic anemia on laboratory exam?
Paroxysmal nocturnal hemoglobinuria
the combination of hemolytic anemia, cytopenias, and hypercoaguable state is suspicious for PNH

What is the likely diagnosis in a patient with acute lymphoblastic leukemia that develops premature ventricular beats and acute kidney injury after initiating chemotherapy?
Tumor lysis syndrome

What is the likely diagnosis in a patient with anemia, painful osteolytic lesions, hypercalcemia, and recurrent infections?
Multiple myeloma
manifestations of MM may be remembered with the mnemonic CRAB: hyperCalcemia, Renal complications, Anemia, Bone lytic lesions

What is the likely diagnosis in a patient with brownish skin pigmentation, elevated fasting glucose, and elevated LFTs?
Hereditary hemochromatosis
other common manifestations include hypogonadism, arthralgias, and hepatomegaly

What is the likely diagnosis in a patient with epistaxis, red blanchable papules on the lips, digital clubbing and isolated polycythemia on laboratory exam?
Hereditary telangiectasia (Osler-Weber-Rendu syndrome)
associated with widespread AV malformations; AVMs in the lung can result in right-to-left shunting with chronic hypoxemia (clubbing), reactive polycythemia, and hemoptysis
What is the likely diagnosis in a patient with hemolytic anemia with an increased MCHC and negative Coombs test?
Hereditary spherocytosis
increased MCHC is classic for hereditary spherocytosis

What is the likely diagnosis in a patient with night sweats, weight loss, and splenomegaly? Laboratory exam reveals leukocytosis with increased levels of basophils and myelocytes.
Chronic myeloid leukemia
high myelocyte count and basophilia favors diagnosis of CML > leukemoid reaction (normal basophil levels and higher metamyelocyte count)

What is the likely diagnosis in a patient with pruritus, especially after bathing, splenomegaly, headaches, and pancytosis on laboratory exam?
Polycythemia vera
almost always caused by a JAK2 mutation

What is the likely diagnosis in a patient with recurrent hemarthrosis after mild trauma and a family history significant for a maternal uncle with a similar issue?
Hemophilia A or B
i.e. factor VIII or IX deficiency, respectively

What is the likely diagnosis in a young adult female with prolonged bleeding and ecchymoses and isolated thrombocytopenia on laboratory exam?
Idiopathic thrombocytopenic purpura (ITP)
diagnosis of exclusion; due to production of IgG autoantibodies against platelet membrane glycoproteins

What is the likely diagnosis in a young adult with worsening knee pain refractory to NSAID therapy and an expansile lytic area in the epiphysis of the distal femur identified on X-ray?
Giant cell tumor of bone (osteoclastoma)
X-ray demonstrates classic “soap-bubble” appearance

What is the likely diagnosis in a young male that presents with irritability, aggressive behavior, and gynecomastia with isolated polycythemia on laboratory exam?
Androgen abuse
mechanism underlying polycythemia is not well understood

What is the likely diagnosis in an adult African-American patient that presents with splenomegaly and scleral icterus two weeks after having a URI treated with amoxicillin? Peripheral blood smear reveals spherocytosis.
Autoimmune hemolytic anemia
sickle cell disease is less likely given the splenomegaly and spherocytes; AIHA may be precipitated by viral infections and penicillins









