Gi and Nutrition II Flashcards
The symptoms of pellagra can be remembered as the “3 D’s”:
D: Dermatitis (hyperpigmented, scaly skin in sun-exposed areas)
D: […]
D: Dementia
The symptoms of pellagra can be remembered as the “3 D’s”:
D: Dermatitis (hyperpigmented, scaly skin in sun-exposed areas)
D: Diarrhea
D: Dementia
causes include malnutrition, isoniazid use, carcinoid syndrome (due to deficiency of tryptophan), and Hartnup disease (impaired absorption of tryptophan)

The symptoms of pellagra can be remembered as the “3 D’s”:
D: Dermatitis (hyperpigmented, scaly skin in sun-exposed areas)
D: Diarrhea
D: […]
The symptoms of pellagra can be remembered as the “3 D’s”:

D: Dermatitis (hyperpigmented, scaly skin in sun-exposed areas)
D: Diarrhea
D: Dementia
causes include malnutrition, isoniazid use, carcinoid syndrome (due to deficiency of tryptophan), and Hartnup disease (impaired absorption of tryptophan)
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: […]
A: arthralgias
N: neurologic symptoms
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: cardiac symptoms
A: arthralgias
N: neurologic symptoms
other common symptoms are lymphadenopathy, chronic cough, and GI symptoms
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: cardiac symptoms
A: […]
N: neurologic symptoms
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: cardiac symptoms
A: arthralgias
N: neurologic symptoms
other common symptoms are lymphadenopathy, chronic cough, and GI symptoms
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: cardiac symptoms
A: arthralgias
N: […]
The symptoms of Whipple’s disease may be remembered with the mnemonic “Whipped cream in a CAN”:
C: cardiac symptoms
A: arthralgias
N: neurologic symptoms
other common symptoms are lymphadenopathy, chronic cough, and GI symptoms
Toxic megacolon is a medical emergency that requires nasogastric decompression, antibiotics, IV fluids +/- […] (if IBD associated).
Toxic megacolon is a medical emergency that requires nasogastric decompression, antibiotics, IV fluids +/- steroids (if IBD associated).
if the colitis does not resolve, emergency surgery may be required

Weight loss, jaundice, and a non-tender, distended gallbladder are consistent with tumors in the […] of the pancreas.
Weight loss, jaundice, and a non-tender, distended gallbladder are consistent with tumors in the head of the pancreas.
other symptoms include pruritus, pale stools, and dark urine (obstructive jaundice)
What acid-base disturbance is classically found in patients with laxative abuse?
Metabolic alkalosis
versus the metabolic acidosis typically found with diarrhea
What age should patients with average risk of colon cancer begin screening?
50 years
either with fecal occult blood testing, flexible sigmoidoscopy, or colonoscopy
What anti-seizure medication is a common cause of drug-induced pancreatitis?
Valproic acid
other common drug classes include diuretics and antibiotics (e.g. metronidazole)

What antibiotic regimen is used to treat fulminant C. difficile colitis?
IV metronidazole + oral vancomycin
fulminant disease includes patients with shock, hypotnesion, ileus, or megacolon; rectal vancomycin may be used in patients with ileus

What antibiotic should be started for patients with a first episode of non-fulminant C. difficile colitis?
Oral vancomycin or fidaxomicin
oral metronidazole may be used if the above agents are unavailable
note: these are NEW guidelines (2018), older guidelines may list metronidazole as the first-line treatment

What antibiotic should be started for patients with a first recurrence of C. difficile colitis?
Oral vancomycin or fidaxomicin
use whichever antibiotic was not used for the initial infection (e.g. if initial infection treated with vancomycin, treat with fidaxomicin)

What antibody is associated with primary sclerosing cholangitis?
p-ANCA

What antibody is characteristically elevated in primary biliary cholangitis?
Anti-mitochondrial antibody

What are first-line agents (2) used to lower NH3 levels in hepatic encephalopathy?
lactulose and rifaximin
neomycin may be used to treat HE in patients unresponsive to lactulose and unable to tolerate rifaximin

What AST:ALT ratio is indicative of heavy alcohol use?
>2:1 AST:ALT
What AST:ALT ratio is typically seen in non-alcoholic fatty liver disease (NAFLD)?
< 1 AST:ALT
useful distinguishing feature from alcoholic hepatitis, which is characterized by >2:1 AST:ALT ratio

What biliary disease is characterized by a “beads-on-a-string” appearance on imaging?
Primary sclerosing cholangitis

What characteristics (growth pattern, histology) of colonic adenomatous polyps suggest greater malignant potential?
sessile growth and villous histology
other signs of malignant potential include large size (> 1 cm) and high number (> 3 concurrent adenomas)

What class of analgesics are associated with pill esophagitis?
NSAIDs
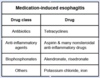
What class of antibiotics is associated with pill esophagitis?
Tetracyclines
What class of osteoporosis drugs are associated with pill esophagitis?
Bisphosphonates

What combined antibiotic regimen can be used for C. difficile colitis in patients with multiple recurrences?
Vancomycin followed by rifaximin
alternatives to this treatment option include oral vancomycin (prolonged course), oral fidaxomicin, or fecal microbiota transplant





















































