Cardio - Biochemistry - Hemoglobin; Sickle Cell Anemia & Thalassemia; Immunoglobulins; Erythrocytosis Flashcards
Why is hemoglobin a necessary component of efficient oxygen transport within the body?
O2 is relatively insoluble
(as are all nonpolar gases)
Which is more soluble in blood (and any aqueous solution), polar or nonpolar gases?
Polar gases
What are some examples of gases in the body that are relatively insoluble?
O2,
N2,
CO2
(all nonpolar - CO2 is slightly less so due to its dipoles)
What are some examples of gases in the body that are relatively soluble?
Ammonia,
hydrogen sulfide
(polar gases)
At what pH is O2 / hemoglobin binding increased, high or low?
High pH
At what pH is O2 / hemoglobin binding decreased, high or low?
Low pH
Which of the following affect myoglobin affinity for O2?
pH
2,3-DPG
CO2
None of them
(myoglobin not regulated by pH or modifying molecules as hemoglobin is)
Hemoglobin is made up of how many subunits?
Myoglobin is made up of how many subunits?
4;
1
What are the two contributing portions of a heme molecule?
The protoporphyrin IX ring
+
Fe2+ (ferrous iron)
How many bonds can a single ferrous iron atom make?
To what structure(s) is one ferrous iron atom bound in a single heme molecule?
6;
4 bonds to the protoporphyrin IX ring,
1 bond to a posterior histidine (from helix F),
1 potential bond to oxygen

Binding of O2 to the ferrous iron in a heme molecule leads to _______ movement of what amino acid also bound to the ferrous iron?
Lateral;
histidine

Ferrous iron is notated as ___?
Is this an oxidized or reduced form of Fe?
Fe2+;
reduced (as opposed to oxidized, ferric iron –> Fe3+)
True/False.
Ligand binding to molecules such as hemoglobin is all of the following: specific, reversible, and transient.
True.
What is the Kd in regards to ligands for a molecule like myoglobin?
The concentration [L] of the ligand (mM) at which 50% of the available binding sites are occupied (on average)

A ligand with high affinity for its substrate protein (e.g. hemoglobin) will have what type of Kd, high or low?
Low
A Kd in ligand binding is equivalent to what type of constant in Michaelis-Menten kinetics?
Km

- (low Kd = high affinity;*
- high Kd = low affinity)*
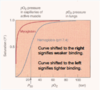
What does sigma represent in the attached graph?
(Note: the graph shows myoglobin O2 binding in relation to partial pressure of O2)

θ = binding sites filled
(in this case, by O2)
Which is indicative of high ligand affinity in a graph comparing binding sites to partial pressure of the gas in question, a right shift or a left shift?

Left shift

A right shift in a graph showing hemoglobin-O2 binding would indicate what type of affinity, high or low?
Low

The hemoglobin-O2 binding curve is ___________, indicating cooperativity.
The myoglobin-O2 binding curve is ___________, indicating no cooperativity.
Sigmoidal;
hyperbolic
The myoglobin-O2 binding curve is hyperbolic, indicating no __________.
The hemoglobin-O2 binding curve is sigmoidal, indicating __________.
Cooperativity;
cooperativity

In the T state, the Fe2+ in heme is where?
Pulled out of the plane of the protoporphyrin IX ring
(low affinity for O2)

In the R state, the Fe2+ in heme is where?
In-plane with the protoporphyrin IX ring
(high affinity for O2)

The histidine that binds the heme group Fe2+ is attached to which hemoglobin subunit, α or β?
α
(from helix F)

































