Respiratory - Anatomy and Physiology Flashcards
1
Q
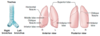
Respiratory tree:
Conducting zone
- Structures
- Functions
- Characteristics
A
- Structures
- Large airways consist of nose, pharynx, larynx, trachea, and bronchi.
- Small airways consist of bronchioles and terminal bronchioles
- Large numbers in parallel –> least airway resistance
- Functions
- Warms, humidifies, and filters air but does not participate in gas exchange –> “anatomic dead space.”
- Characteristics
- Cartilage and goblet cells extend to end of bronchi.
- Pseudostratified ciliated columnar cells (beat mucus up and out of lungs) extend to beginning of terminal bronchioles, then transition to cuboidal cells.
- Airway smooth muscles extend to end of terminal bronchioles (sparse beyond this point).

2
Q
Respiratory tree:
Respiratory zone
- Structures
- Functions
- Characteristics
A
- Structures
- Lung parenchyma
- Consists of respiratory bronchioles, alveolar ducts, and alveoli.
- Functions
- Participates in gas exchange.
- Characteristics
- Mostly cuboidal cells in respiratory bronchioles, then simple squamous cells up to alveoli.
- No cilia.
- Alveolar macrophages clear debris and participate in immune response.

3
Q
Pneumocytes
- For each
- Functions
- Characteristics
- Type I cells
- Type II cells
- Club (Clara) cells
A
- Type I cells
-
Functions:
- 97% of alveolar surfaces.
- Line the alveoli.
-
Characteristics:
- Squamous
- Thin for optimal gas diffusion.
-
Functions:
- Type II cells
-
Functions:
- Secrete pulmonary surfactant –> decreased alveolar surface tension and prevention of alveolar collapse (atelectasis).
- Also serve as precursors to type I cells and other type II cells
- Proliferate during lung damage
-
Characteristics:
- Cuboidal
- Clustered.
-
Functions:
- Club (Clara) cells
-
Functions:
- Secrete component of surfactant
- Degrade toxins
- Act as reserve cells
-
Characteristics:
- Nonciliated
- Low-columnar/cuboidal with secretory granules.
-
Functions:
4
Q
Pneumocytes
- Collapsing pressure equation
- Law of Laplace
- Pulmonary surfactant
- Surfactant synthesis
A
- Collapsing pressure
- P = [2 * (surface tension)] / radius
- Law of Laplace
- Alveoli have increased tendency to collapse on expiration as radius decreases
- Pulmonary surfactant
- A complex mix of lecithins, the most important of which is dipalmitoylphosphatidylcholine.
- Surfactant synthesis
- Begins around week 26 of gestation
- Mature levels are not achieved until around week 35.
- Lecithin-to-sphingomyelin ratio
- > 2.0 in amniotic fluid indicates fetal lung maturity.
5
Q
Lung relations
- Right lung
- Left lung
- The relation of the pulmonary artery to the bronchus at each lung hilus
- Where an aspirated peanut travels
- While upright
- While supine
A
- Right lung
- Right lung has 3 lobes
- Right lung is more common site for inhaled foreign body because the right main stem bronchus is wider and more vertical than the left
- Left lung
- Left has Less Lobes (2) and Lingula (homologue of right middle lobe).
- Instead of a middle lobe, the left lung has a space occupied by the heart.
- The relation of the pulmonary artery to the bronchus at each lung hilus
- Described by RALS—Right Anterior; Left Superior.
- Where an aspirated peanut travels
- While upright—lower portion of right inferior lobe.
- While supine—superior portion of right inferior lobe.
6
Q
Diaphragm structures
- Structures perforating diaphragm
- At T8
- At T10
- At T12
- Diaphragm
- Innervation
- Pain referral
A
- Structures perforating diaphragm
- At T8: IVC
- At T10: esophagus, vagus (CN 10; 2 trunks)
-
At T12: aorta (red), thoracic duct (white), azygos vein (blue)
- “At T-1-2 it’s the red, white, and blue”
-
Number of letters = T level:
- T8: vena cava
- T10: “oesophagus”
- T12: aortic hiatus
- I (IVC) ate (8) ten (10) eggs (esophagus) at (aorta) twelve (12).
- Diaphragm
- Innervation
- Innervated by C3, 4, and 5 (phrenic nerve).
- C3, 4, 5 keeps the diaphragm alive.
- Pain referral
- Pain from diaphragm irritation (e.g., air or blood in peritoneal cavity) can be referred to the shoulder (C5) and the trapezius ridge (C3, 4).
- Innervation

7
Q
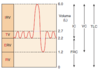
Lung volumes
- Inspiratory reserve volume (IRV)
- Tidal volume (TV)
- Expiratory reserve volume (ERV)
- Residual volume (RV)
A
- Inspiratory reserve volume (IRV)
- Air that can still be breathed in after normal inspiration
- Tidal volume (TV)
- Air that moves into lung with each quiet inspiration
- Typically 500 mL
- Expiratory reserve volume (ERV)
- Air that can still be breathed out after normal expiration
- Residual volume (RV)
- Air in lung after maximal expiration
- Cannot be measured on spirometry
-
Lung volumes (LITER):
- IRV
- TV
- ERV
- RV
8
Q
Lung capacities
- Inspiratory capacity (IC)
- Functional residual capacity (FRC)
- Vital capacity (VC)
- Total lung capacity (TLC)
- Capacity
A
- Inspiratory capacity (IC)
- IRV + TV
- Functional residual capacity (FRC)
- RV + ERV
- Volume in lungs after normal expiration
- Vital capacity (VC)
- TV + IRV + ERV
- Maximum volume of gas that can be expired after a maximal inspiration
- Total lung capacity (TLC)
- IRV + TV + ERV + RV
- Volume of gas present in lungs after a maximal inspiration
- Capacity
- A capacity is a sum of ≥ 2 volumes.
9
Q
Determination of physiologic dead space
- Definition
- Equation
A
- Definition
- Anatomic dead space of conducting airways plus functional dead space in alveoli
- Apex of healthy lung is largest contributor of functional dead space.
- Volume of inspired air that does not take part in gas exchange.
- Equation
- VD = VT × [(PaCO2 – PeCO2) / PaCO2]
- Taco, Paco, Peco, Paco (refers to order of variables in equation)
- VT = tidal volume
- PaCO2 = arterial PCO2
- PeCO2 = expired air PCO2
- VD = VT × [(PaCO2 – PeCO2) / PaCO2]
10
Q
Ventilation
- For each
- Definition
- Equation
- Minute ventilation (VE)
- Alveolar ventilation (VA)
A
- Minute ventilation (VE)
- Total volume of gas entering the lungs per minute
- VE = VT × respiratory rate (RR)
- Alveolar ventilation (VA)
- Volume of gas per unit time that reaches the alveoli
- VA = (VT - VD) × RR
11
Q
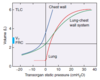
Lung and chest wall
- Tendencies
- Lungs
- Chest wall
- What determines their combined volume
- At FRC
- System pressure
- Airway and alveolar pressures
- Intrapleural pressure
- Pulmonary vascular resistance (PVR)
- Compliance
- Definition
- Decreased in…
- Increased in..
A
- Tendencies
- Lungs to collapse inward
- Chest wall to spring outward.
- Elastic properties of both chest wall and lungs determine their combined volume
- At FRC
- Inward pull of lung is balanced by outward pull of chest wall, and system pressure is atmospheric.
- Airway and alveolar pressures are 0
- Intrapleural pressure is negative (prevents pneumothorax).
- Pulmonary vascular resistance (PVR) is at minimum.
- Compliance
- Change in lung volume for a given change in pressure
- Decreased in pulmonary fibrosis, pneumonia, and pulmonary edema
- Increase in emphysema and normal aging.
12
Q
Hemoglobin (Hb)
- Hemoglobin
- Composition
- Forms
- Effect of increased Cl-, H+, CO2, 2,3-BPG, and temperature
- Fetal Hb
- Composition
- Difference
A
- Hemoglobin
- Composed of 4 polypeptide subunits (2 α and 2 β)
- Exists in 2 forms
- T (taut) form has low affinity for O2.
- Taut in Tissues.
- R (relaxed) form has high affinity for O2 (300×).
- Hb exhibits positive cooperativity and negative allostery.
- Relaxed in Respiratory tract.
- T (taut) form has low affinity for O2.
- Effect of increased Cl-, H+, CO2, 2,3-BPG, and temperature
- Increased Cl-, H+, CO2, 2,3-BPG, and temperature favor taut form over relaxed form
- Shifts dissociation curve to right, leading to O2 unloading).
- Fetal Hb
- 2 α and 2 γ subunits
- Has lower affinity for 2,3-BPG than adult Hb and thus has higher affinity for O2.

13
Q
Hemoglobin modifications
- Lead to…
- Methemoglobin
- Definition
- Methemoglobinemia
- To treat cyanide poisoning
- Carboxyhemoglobin
- Definition
- Causes…
A
- Lead to tissue hypoxia from decreased O2 saturation and decreased O2 content.
- Methemoglobin
- Definition
- Oxidized form of Hb (ferric, Fe3+) that does not bind O2 as readily, but has increased affinity for cyanide.
- Iron in Hb is normally in a reduced state (ferrous, Fe2+).
- Just the 2 of us: ferrous** is Fe_2+_.**
- Methemoglobinemia
- May present with cyanosis and chocolate-colored blood.
- To treat cyanide poisoning
- Use nitrites to oxidize Hb to methemoglobin, which binds cyanide.
- Nitrites cause poisoning by oxidizing Fe2+ to Fe3+.
- Use thiosulfate to bind this cyanide, forming thiocyanate, which is renally excreted.
- Methemoglobinemia can be treated with methylene blue.
- Use nitrites to oxidize Hb to methemoglobin, which binds cyanide.
- Definition
- Carboxyhemoglobin
- Definition
- Form of Hb bound to CO in place of O2.
- CO has 200× greater affinity than O2 for Hb
- Causes…
- Decreased oxygen-binding capacity with a left shift in the oxygen-hemoglobin dissociation curve.
- Decreased O2 unloading in tissues.
- Definition
14
Q
Oxygen-hemoglobin dissociation curve
- Shape
- Hemoglobin
- Myoglobin
- Curve shifts
- Right
- Left
- Fetal Hb
A
- Shape
- Hemoglobin
- Sigmoidal shape due to positive cooperativity
- i.e., tetrameric Hb molecule can bind 4 O2 molecules and has higher affinity for each subsequent O2 molecule bound.
- Myoglobin
- Monomeric and thus does not show positive cooperativity
- Curve lacks sigmoidal appearance.
- Hemoglobin
- Curve shifts
- An increase in all factors (including H+) causes a shift of the curve to the right.
- When curve shifts to the right, decrease affinity of Hb for O2 (facilitates unloading of O2 to tissue)
-
Right shift—BAT ACE:
- BPG (2,3-BPG)
- Altitude
- Temperature
- Acid
- CO2
- Exercise
- A decrease in all factors (including H+) causes a shift of the curve to the left
- Fetal Hb has a higher affinity for O2 than adult Hb, so its dissociation curve is shifted left
- An increase in all factors (including H+) causes a shift of the curve to the right.

15
Q
Oxygen content of blood
- Hb
- Normal
- Cyanosis
- O2 content vs. saturation
- Equations
- O2 content
- O2 delivery to tissues
A
- Hb
- Normal
- Normally 1 g Hb can bind 1.34 mL O2
- Normal Hb amount in blood is 15 g/dL.
- O2 binding capacity ≈ 20.1 mL O2/dL
- Cyanosis
- Results when deoxygenated Hb > 5 g/dL.
- Normal
- O2 content vs. saturation
- O2 content of arterial blood decreases as Hb falls
- O2 saturation and arterial Po2 do not
- Equations
- O2 content = (O2 binding capacity × % saturation) + dissolved O2
- O2 delivery to tissues = cardiac output × O2 content of blood
16
Q
Oxygen content of blood
- For each (increased/decreased)
- Hb level
- % O2 sat of Hb
- Dissolved O2 (PaO2)
- Total O2 content
- CO poisoning
- Anemia
- Polycythemia
A
- CO poisoning
- Hb level: Normal
- % O2 sat of Hb: Decreased (CO competes with O2)
- Dissolved O2 (PaO2): Normal
- Total O2 content: Decreased
- Anemia
- Hb level: Decreased
- % O2 sat of Hb: Normal
- Dissolved O2 (PaO2): Normal
- Total O2 content: Decreased
- Polycythemia
- Hb level: Increased
- % O2 sat of Hb: Normal
- Dissolved O2 (PaO2): Normal
- Total O2 content: Increased
17
Q
Pulmonary circulation (599)
- System
- Normally…
- Po2 and Pco2
- A decrease in PAo2 causes…
- Limitations
- Perfusion limited
- Diffusion limited
A
- System
- Normally a low-resistance, high-compliance system.
- Po2 and Pco2 exert opposite effects on pulmonary and systemic circulation.
- A decrease in PAo2 causes a hypoxic vasoconstriction that shifts blood away from poorly ventilated regions of lung to well-ventilated regions of lung.
- Limitations
- Perfusion limited
- O2 (normal health), CO2, N2O.
- Gas equilibrates early along the length of the capillary.
- Diffusion can be increased only if blood flow increases.
- Diffusion limited
- O2 (emphysema, fibrosis), CO.
- Gas does not equilibrate by the time blood reaches the end of the capillary.
- Perfusion limited

18
Q
Pulmonary circulation (599)
- A consequence of pulmonary hypertension
- Diffusion equation
- Diffusion pathologies
- Area
- Thickness
A
- A consequence of pulmonary hypertension
- Cor pulmonale
- Subsequent right ventricular failure (jugular venous distention, edema, hepatomegaly).
- Diffusion equation
- Vgas = (A / T) × Dk (P1 – P2)
- A = area
- T = thickness
- Dk (P1 – P2) ≈ difference in partial pressures
- Diffusion pathologies
- Area decreased in emphysema.
- Thickness increased in pulmonary fibrosis.

19
Q
Pulmonary vascular resistance
- PVR equation
- Resistance equations
A
- PVR = ( Ppulm artery – PL atrium ) / cardiac output
- Ppulm artery = pressure in pulmonary artery
- PL atrium = pulmonary wedge pressure
- Resistance equations
- ΔP = Q × R
- R = ΔP / Q
- R = 8ηl / πr4
- η = viscosity of blood
- l = vessel length;
- r = vessel radius
20
Q
Alveolar gas equation
- PAo2 equation
- A-a gradient
- Equation
- Definition
A
- PAo2 = PIo2 – (Paco2 / R) ≈ 150 – (Paco2 / 0.8)
- PAo2 = alveolar Po2 (mmHg).
- PIo2 = Po2 in inspired air (mmHg).
- Paco2 = arterial Pco2 (mmHg).
- R = respiratory quotient = CO2 produced / O2 consumed.
- A-a gradient
- A-a gradient = PAo2 – Pao2 = 10–15 mmHg.
- Definition
- Increased A-a gradient may occur in hypoxemia
- Causes include shunting, V/Q mismatch, fibrosis (impairs diffusion).
21
Q
Oxygen deprivation
- For each
- Definition
- Due to…
- Hypoxemia
- Normal A-a gradient
- Increased A-a gradient
- Hypoxia
- Ischemia
A
- Hypoxemia
- Definition
- Decreased Pao2
- Due to…
- Normal A-a gradient
- High altitude
- Hypoventilation
- Increased A-a gradient
- V/Q mismatch
- Diffusion limitation
- Right-to-left shunt
- Normal A-a gradient
- Definition
- Hypoxia
- Definition
- Decreased O2 delivery to tissue
- Due to…
- Decreased cardiac output
- Hypoxemia
- Anemia
- CO poisoning
- Definition
- Ischemia
- Definition
- Loss of blood flow
- Due to…
- Impeded arterial flow
- Decreased venous drainage
- Definition
22
Q
V/Q mismatch
- Ideal V/Q
- V/Q in lung zones
- Apex
- Base
- Comparison
- V/Q with exercise
- Limits
- V/Q –> 0
- V/Q –> ∞
A
- Ideal V/Q
- Ideally, ventilation is matched to perfusion (i.e., V/Q = 1) in order for adequate gas exchange.
- V/Q in lung zones
- Apex
- V/Q = 3 (wasted ventilation)
- Base
- V/Q = 0.6 (wasted perfusion)
- Comparison
- Both ventilation and perfusion are greater at the base of the lung than at the apex of the lung.
- Certain organisms that thrive in high O2 (e.g., TB) flourish in the apex
- Apex
- V/Q with exercise
- With exercise (increased cardiac output), there is vasodilation of apical capillaries, resulting in a V/Q ratio that approaches 1.
- Limits
- V/Q –> 0 = airway obstruction (shunt).
- In shunt, 100% O2 does not improve Po2.
- V/Q –> ∞ = blood flow obstruction (physiologic dead space).
- Assuming < 100% dead space, 100% O2 improves Po2.
- V/Q –> 0 = airway obstruction (shunt).

23
Q
CO2 transport
- CO2 is transported from tissues to the lungs in 3 forms:
- In lungs
- In peripheral tissue
A
- CO2 is transported from tissues to the lungs in 3 forms:
- HCO3- (90%).
- Majority of blood CO2 is carried as HCO3- in the plasma
- Carbaminohemoglobin or HbCO2 (5%).
- CO2 bound to Hb at N-terminus of globin (not heme).
- CO2 binding favors taut form (O2 unloaded).
- Dissolved CO2 (5%).
- HCO3- (90%).
- In lungs
- Oxygenation of Hb promotes dissociation of H+ from Hb.
- This shifts equilibrium toward CO2 formation
- Therefore, CO2 is released from RBCs (Haldane effect).
- In peripheral tissue
- Increased H+ from tissue metabolism shifts curve to right, unloading O2 (Bohr effect).

24
Q
Response to high altitude
- Atmospheric oxygen
- Ventilation
- Erythropoietin
- 2,3-BPG
- Mitochondria
- Renal excretion of HCO3-
- Pulmonary
A
- Decreased atmospheric oxygen –> decreased Pao2 –> increased ventilation –> decreased Paco2.
- Chronic increase in ventilation.
- Increased erythropoietin –> increased hematocrit and Hb (chronic hypoxia).
- Increased 2,3-BPG (binds to Hb so that Hb releases more O2).
- Cellular changes (increased mitochondria).
- Increased renal excretion of HCO3- (e.g., can augment by use of acetazolamide) to compensate for the respiratory alkalosis.
- Chronic hypoxic pulmonary vasoconstriction results in RVH.
25
Q
Response to exercise
- CO2 production
- O2 consumption
- Ventilation rate
- V/Q ratio
- Pulmonary blood flow
- pH
- Pao2
- Paco2
- Venous CO2 content
- Venous O2 content
A
- Increased CO2 production.
- Increased O2 consumption.
- Increased ventilation rate to meet O2 demand.
- V/Q ratio from apex to base becomes more uniform.
- Increased pulmonary blood flow due to increased cardiac output.
- Decreased pH during strenuous exercise (2° to lactic acidosis).
- No change in Pao2
- No change in Paco2
- Increase in venous CO2 content
- Decrease in venous O2 content.


