Test 5 - pulmonary Flashcards
What are the clinical symptoms of brocnhitis? Is fever a common symptom?
productive cough
wheezing
fever is unusual
How is bronchitis diagnosed?
Clinical diagnosis - based on symptoms of cough, wheezing. CXR is only indicated if pneumonia is suspected, and if consolidation is not seen pneumonia can be ruled out.
What is pneumonia?
Infection of the lung parynchyma (respiratory airways)
Pneumonia is categorized into 4 types. Name these 4 types (one type is further divided into two categories)
Community acquired (typical and atypical)
Hospital acquired
Health-care associated
Opportunistic
What are the clinical symptoms of pneumonia?
fever
chest pain
dyspnea
productive cough
How is pneumonia diagnosed? Is culture often performed?
Diagnosis is made with clinical symptoms and a chest x-ray with focal lung opacities
Culture is not usually performed because patients cannot expectorate sputum and even if they can the culture is contaminated with oropharyngeal bacteria
How is pneumonia treated? discuss community-acquired and hospital-acquired treatments

What is Mycobacterium tuberculosis? (stain, shape, and type of microbe)
Tuberculosis is an acid fast rod bacterium
How is TB transmitted?
air droplets
Describe the potential course of TB (primary infection, etc)

What are the general clinical symptoms of TB?
productive cough
fever
malaise
weight loss
+/- hemoptysis
If TB becomes systemic, what diseases can the patient develop?
Pott’s disease (TB in the vertebrae)
Milliary disease (widespread dissemination)
How is active TB diagnosed (there are a few methods you should name)? Can IGRA or a PPD test diagnose active TB?
CXR
Sputum smear with acid fast stain (takes 4-6 weeks to culture)
nucleic acid amplification
IGRA and PPD CANNOT diagnose active TB

Is PPD specific to Mycobacterium tuberculosis?
If the patient recieved a BCG vaccination, PPD will yield a positive result
How does primary TB and secondary TB present on CXR?
Primary TB has cavitary lesions in the lower/middle lobe(s)
Secondary has cavitary lesions in the upper lobe(s)
Note: hilar LAD may be present in both

What are risk factors for developing active TB?
Malnutrition
immunocompromized patients (drugs, HIV)
Diabetes
alcoholism
children under 2 years of age
How is TB treated?

What type of infectious agent causes pneumocystis pneumonia and in what patient population is this infection seen in?
PCP is a fungal pneumonia (caused by Pneumocystis jirovecii) that is commonly seen in AIDS patients with a CD4 count below 200
What are the clinical symptoms of pneumocystis pneumonia?
fever
non-productive cough
dyspnea
How is pneumocystis diagnosed?
Chest imaging (ground glass opacities) +/- “crushed ping-pong balls” opacities
Bronchoalveolar lavage crushed ping-pong balls morphology
What is the treatment for pneumocystis pneumonia?
Bactrim (sulfamethoxazole and trimethoprim)
What is bronchiolitis?
Inflammation of the bronchioles
What age is bronchiolitis typically seen in? What are the clinical symptoms of bronchiolitis?
Seen in children under 6 months
coryza (stuffy nose)
Rhinorrhea (runny nose)
cough
wheezing
chest wall retractions
respiratory distress
difficulty feeding due to increased work of breathing
How is bronchiolitis diagnosed?
CXR:
air trapping
peribronchial thickening
subsegmental opacities
How is bronchiolitis treated?
Supportive therapy only:
fluids, O2, bronchodilators
What is laryngeotracheobronchitis?
Croup
upper airway obstruction
What causes croup?
RSV and parainfluenza
What are the clinical symptoms of croup? Is fever common?
Seal bark cough
Stridor (inspiratory wheeze)
hoarsness
fever is not common
How do you diagnose croup? Do you use a tongue depressor to examine the pharynx?
Steeple sign on XR
DO NOT stick anything in through as the airway could collapse!!

How is croup treated?
For kids in respiratory distress - aerosolized racemic epinephrine reduced subglottic edema
Systemic steroids
What is epiglottitis? What is the most common cause?
inflammation of the epiglottis
H. influenzae
What are the clinical symptoms of epiglottitis?
fever
drooling
dysphagia
refusal to eat/drink
sudden onset of stridor
How is epiglottitis diagnosed?
Thumb sign on XR

How is epiglottitis treated?
intubation
antibiotics
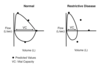
Draw the restricive pattern dendritic
Notice that hypersensitivity pneumonitis is under granulomatous diseases and inhaled. Inhalation of particles results in non-caseating granulomas

What are the finding in a restricitve pattern? (PFT results)

What changes can be seen on a spirogram in restrictive diseases? Are RV and FRC reduced in neuromuscular diseases?
RV is normal/high in neruromuscular disease
FRC is normal in neuromuscular disease

What changes can be seen on a flow-volume loop in restrictive diseases?
What are the 3 categories (heavily focused on in sullabus) of diffuse parenchymal lung disease?
Idiopathic pulmonary fibrosis
granulomatous disease
inhaled disease
What is Idiopathic pulmonary fibrosis?
increased flibroblast growth and collagen synthesis in the alveolar interstitium
What are the clinical symptoms of idiopathic pulmonary fibrosis? Is it an acute process? is the prognosis good or bad?
exertional dyspnea (decreaed RBC transit time)
dry cough
inspiratory crackles at lung bases (velco sounding)
digital clubbing
It is a slow, insideous process that shows up late in life (poor prognosis)
How does IPF change FEV1, FVC, FEV1/FVC, DLCO, A-a O2 difference
reduced FEV1, FVC, DLCO
normal FEV1/FVC
increased A-a O2 difference
How does IPF present on CXR? CT?
CXR
low lung volumes, reticulonodular opacities
CT
honeycombing at lung bases

How is IPF diagnosed?
history, PFTs, and imaging
biopsy is not always required
How is IPF treated?
There are no real treatments for IPF
anti-fibrotic agent prifenidone may help to slow down progression
What diseases are classified under granulomatous restrictive lung diseases?
Sarcoidosis
Hypersensitivity pneumonitis
What is sarcoidosis?
inflammation process that results in the formation of non-caseating granulomas in the lungs
In severe cases, the disease is systemic
Who is at high risk for sarcoidosis? What organ systems are involved in systemic disease?
black women
heart, CNS, liver, spleen, skin, eyes
What are the clinical symptoms of intrapulmonary sarcoidosis? extrapulmonary?
Intrapulmonary:
typically asymptomatic
dyspnea
nonproductive cough
Extrapulmonary:
arrhythmias (heart block)
uveitis
hepatomegaly
Lofgren’s syndrome (erythemia nodosum, fever, hilar LAD)
How is sarcoidosis diagnosed?
symptoms, CXR, and biopsy of non-caseating granulomas
How is sarcoidosis treated?
Disease spontaneously resolves in most patients
For those with severe pulmonary symptoms, corticosteroids are used
What disease closely resembles sarcoidosis?
Berylliosis
What is hypersensitivity pneumonitis
parenchymal lung disease characterized by non-caseating granulomas brought on by the inhalation of particles (specific particles)
Is HSP reversible?
In most cases, yes
What are the clinical symptoms of hypersensitivity pneumonitis?
Presents like pneumonia
fever
dyspnea
cough
When do hypersensitivity pneumonitis symptoms present?
4-8 hours after exposure
How does HSP present on radiograph? Acute vs Chronic
Acute:
ground glass opacities (similar to PCP) with upper lobe predominance
Chronic:
volume loss
reticular opacities
honeycombing

How is hypersensitivity pneumonitis diagnosed?
re-expose patient to particle and see if symptoms recur
How is HSP treated?
Avoid the antigen
steroids in acute, severe situations
What diseases are classified under inhaled?
Hypersensitivity pneumonitis
Asbestosis
Silicosis
Coal Worker’s pneumoconiosis (black lung)
Berylliosis
What is asbestosis?
A fibrotic lung disease brought on by the inhalation of asbestos
Who is at risk for asbestosis?
occupational hazard:
shipyard/shipbuilding
brak lining work
insulation and textiles
stone polishing and cutting
What is the pathophysiology of asbestos?
Fibers are inhaled —> lower resp. tract —> pneumocytes and alveolar macrophages release inflammatory mediators, ROS, free radicals —> progressive fibrosis