Sudden Death in Lambs Flashcards
what are reasons for sudden death in growing lambs
Clostridial diseases
Pasteurellosis —> septicaemia (M. hemolytica, P. Multocida), systemic (Pasteurella trehalosi)
Acidosis (grain overload) vs cerebrocortical necrosis (CCN)
Acute liver fluke
Others
what are clostridial diseases and the bacteria that cause them (7)
- lamb dysentery (clostridium perfringens type B)
- pulpy kidney (cl. perfringens type D)
- black leg (cl. chauvoei)
- tetanus (cl. tetani)
- black disease (cl. novyi type B)
- braxy (cl. septicum)
- abomasitis (cl. sordellii)
what are the clinical features of pulpy kidney
Enterotoxemia
what does pulpy kidney cause
Sudden death in non-immune lambs
what age of lamb does pulpy kidney commonly affect
4 weeks to 8 month old lambs
Often the bigger, better lambs
what could be seen in pulpy kidney if the lambs are alive
Severe depression
Abdominal pain
Grinding teeth
Neurological signs (seizures, opisthotonus)
describe the pathogenesis of pulpy kidney 12
- organism is present in gut
- reaches high # in presence of undigested CHO (high milk intake or excess food in weaned)
- in presence of trypsin and absence of antibody the protoxin is cleaved to the active ε toxin
- ε is 3rd most lethal C toxin
- ε produced and enters bood
- increased intestinal permeability
- toxin absorbed and fixes to cells in liver, kidney and brain
- in brain causes liquefactive necrosis, perivascular edema and hemorrhage (focal symmetrical encephalomalacia)
- in brain the cell tight junctions degenerate, increased permeability with fluid loss followed by elevated intracranial pressure
- mobilization of hepatic glycogen stores
- hyperglycemia, glycosuria, nervous changes
- death
how is pulpy kidney diagnosed
history of recent move to rich feeding
PM
C. perfringens type D in smears by gram stain, by culture and toxin gene PCR
toxin detectable in ELISA
what is the pathology of pulpy kidney
Good condition, some fecal staining
No gross lesions, clear fluid in body cavities
Small petechial hemorrhages on lungs and epicardium
Pulpy kidneys and glycosuria
Small intestinal contents in fluid
Focal symmetrical hemorrhages in basal ganglia of brain and later focal symmetrical encephalomalacia
C. perfringens type D and its toxin in small intestinal contents
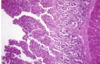
what pathology is shown here

pulpy kidney
how does clostridium chauvoei enter
via skin wounds
ex. shearing, castration
what does blackleg affect
skeletal and cardiac muscle
how do blackleg lambs present
sudden death
or
if alive
dullness
febrile (<41C)
toxic mucous membranes
severe lameness with edema and emphysema
what toxins does c chauvoei produce
α, β, γ, δ
where are C tetani spores found
ubiquitous in soil
when is c tetani commonly associated
docking
castration wounds
what is responsible for the clinical signs in C tetani
production of potent neurotoxin tetanospasmin
what are the clinical signs of C tetani
generalized stiffness
rigidity of limbs
unable to swallow or eructate
progress to convulsions
how are early cases of C tetani treated
tetanus antitoxin
penicillin
what age does black disease affect
sheep of all ages
what does black disease affect
liver
what is C novyi associated with
migration of immature liver fluke in the liver
when is C novyi commonly seen
late autumn/winter
what does C novyi cause
sudden death