Infections - Soft Tissue - Hand Flashcards
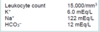
An otherwise healthy 10-year-old girl is brought for evaluation because of a chronic ulcer of the right leg. The ulcer first appeared 6 months ago when she scraped her leg on a boat dock at her family’s lake house. The wound has increased in size despite treatment with a course of oral antibiotic therapy prescribed by her primary care physician. A photograph is shown. On evaluation today, the patient is afebrile and has no systemic signs of infection. Which of the following organisms is the most likely cause of these findings?
A) Candida tropicalis
B) Group A beta-hemolytic Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Mycobacterium marinum
E) Vibrio vulnificus
The correct response is Option D.
The history and presentation are classic for an atypical mycobacterial infection. Unlike bacterial infections, atypical mycobacteria rarely produce systemic signs of infection and often manifest as a nonhealing (sometimes progressive) wound. Given the history of injury on a boat dock, the most likely causative organism is Mycobacterium marinum, an acid-fast bacillus that lives in water environments. This pathogen results in localized granulomas such as the one seen in this patient. Staphylococcus aureus is the most common source of skin infections but typically results in a more pronounced and acute immune reaction with localized redness and purulence. These findings are not present in this patient. Cutaneous infections with Group A beta-hemolytic Streptococcus and Vibrio vulnificus tend to increase rapidly and are often accompanied by severe systemic response (i.e., necrotizing fasciitis). Candida tropicalis is a fungus that is often part of normal skin flora. It is related to Candida albicans and can produce opportunistic internal infections in susceptible individuals.
A 59-year-old man with type 2 diabetes mellitus comes to the office because he has had swelling, pain, and decreased function of the right small finger after he injured it slightly 2 weeks ago. The patient reports similar symptoms of the right thumb, although it sustained no inciting injury. Examination of both digits shows signs and symptoms of pyogenic flexor tenosynovitis. In addition to washing out the respective tendon sheaths, exploration of which of the following additional sites is necessary?
A) First web space
B) Flexor carpi radialis tendon sheath
C) Hypothenar compartment
D) Ring finger flexor tendon sheath
E) Space of Parona
The correct response is Option E.
Infectious flexor tenosynovitis can spread from the tendon sheath of the fifth digit to the flexor tendon sheath of the thumb by way of the space of Parona: the potential space in the volar wrist, deep to the flexor tendons but superficial to the pronator quadratus muscle. In this area, the proximal extent of the tendon sheaths of both the small finger and the thumb are in close proximity. This has been termed the “horseshoe abscess” of the upper extremity.

A 48-year-old right-hand–dominant man with a history of cadaveric renal transplantation comes to the emergency department because of a swollen, painful left hand. A photograph is shown. He works as a crab fisherman and reports that he was bitten in the first web space by a crab 18 hours ago. He is taken to the operating room for emergent debridement. Intraoperative Gram stain shows a gram-negative, curve-shaped rod. In addition to aggressive surgical treatment, administration of which of the following antibiotics is most appropriate to treat this patient?
A) Cephalexin
B) Levofloxacin
C) Linezolid
D) Nafcillin
E) Vancomycin

The correct response is Option B.
Vibrio vulnificus is a common Vibrio species causing soft-tissue infections of the hand. Vibrio species are ubiquitous in aquatic environments including saltwater bodies. Immunocompromised hosts are at greater risk for amputation and death. The best chance for patient survival includes early diagnosis and initiation of appropriate antibiotics, as well as urgent surgical debridement for any evidence of necrotizing infection.
A broad range of antibiotics are effective against Vibrio species, including V. vulnificus. Agents effective against gram-negative rods, including quinolones, aminoglycosides, and aminopenicillins, are all effective against V. vulnificus. While all cephalosporins are effective against Vibrio species, third-generation cephalosporins are up to 130 times more potent than first- or second-generation cephalosporins. Vancomycin, nafcillin, and linezolid are all narrow-spectrum antibiotics, primarily effective against gram-positive cocci, and are not effective against Vibrio species.
A 24-year-old man comes to the emergency department 6 hours after sustaining an open distal radius fracture and loss of soft tissue while he was working on a farm. History includes diabetes mellitus. On physical examination, distal pulses and sensation are intact. Debridement and repair with open reduction and internal fixation are planned. Which of the following factors places this patient at greatest risk for infection postoperatively?
A) Gustilo fracture classification
B) History of diabetes mellitus
C) Method of fracture fixation
D) Period of time from injury to initial debridement
E) Type of contamination
The correct response is Option E.
Of the listed factors relating to risk of postoperative infection in this scenario, the strongest correlation is with contamination type. The Gustilo–Anderson fracture classification has been found to have some correlation with open fracture infection rates, but this relationship is not as strong in the distal radius as it is in long bones of the lower extremity. Recent studies by Glueck, et al, and Swanson, et al, have shown that contamination is a much stronger correlate.
A history of systemic illness, such as diabetes mellitus, and the type of fracture fixation seem to have a modest correlation to postoperative infections in distal radius fractures, but the findings are generally not statistically significant.
The timing of the initial debridement, as long as it occurs within the first 24 hours of injury, does not significantly affect infection rate. In contrast, there is evidence to suggest that performing multiple serial debridements in significantly contaminated wounds is of benefit in preventing postoperative infection.
A 34-year-old woman undergoes laser-assisted liposuction of the abdomen, hips, and inner and outer thighs using a tumescent technique. A total of 2500 mL of aspirate is removed. Postoperative recovery is uneventful, and the patient is discharged home the same day. She comes to the emergency department 4 days later with intense pain over the lower abdomen and flanks. Temperature is 101°F (38.3°C). Physical examination shows the skin has well-demarcated erythema, induration, and bullae forming at multiple sites. Her incisions are seeping clear, grey fluid. Which of the following is the most appropriate management?
A) Exploratory laparotomy for presumed bowel perforation
B) Intravenous administration of antibiotics and local burn care
C) Intravenous administration of antibiotics only
D) Oral administration of antibiotics
E) Surgical debridement of the involved tissue
The correct response is Option E.
Necrotizing fasciitis is a rapidly progressive soft-tissue infection characterized by necrosis of the fascia and subcutaneous fat with subsequent necrosis of the overlying skin. Although complication rates associated with liposuction are not unduly increased, infection is a major concern, and cases of prolonged inflammation, septic shock, and infections have been documented. Likewise, cases of necrotizing fasciitis following liposuction have been reported on several occasions and, according to data reported in the literature, the overall incidence of necrotizing fasciitis is equal to 0.4 per 100,000 patients.
There are two common forms that are reported: infections caused by Streptococcus pyogenes and mixed infections caused by a variety of microbes, including Escherichia coli, Proteus, Serratia, and Staphylococcus aureus. A detailed case of necrotizing fasciitis sustained by Mycobacterium chelonae after a combined procedure of liposuction and lipofilling has also been described. The progressive necrosis of the tissues typically involves the superficial fascia and the subcutaneous layer, but is limited in extension to the skin; the extent of the gangrene at the fascial layer is usually more severe and greater than at the skin level.
Necrotizing fasciitis is virtually unnoticeable in the first 48 hours with nonspecific symptoms. In the days that follow, an extensive, hardened region forms, which is often dark in the center. Severe pain and necrosis follow at the level of the infection.
Drainage of “dishwater fluid” is often pathognomonic. Metabolic changes occur, ending with respiratory distress, oliguria, acidosis, increased troponin concentrations, and sepsis. Diagnosis and treatment consist of surgical exploration and debridement that reveal necrotic, edematous, subcutaneous fat. Bacteriologic analysis of exudate, cultures, and histologic evaluation complete the diagnosis.
Early diagnosis is imperative to avoid a fatal outcome. Treatment is based on immediate and aggressive surgical debridement with combined antibiotic therapy. Because necrotizing fasciitis is a progressive, rapid infection, the wound typically is left open for a planned “second-look” operation and additional debridement if necessary. The mortality rates are increased and range up to 70% but decrease to 4.2% after immediate surgical intervention. Delay in debridement increases mortality.
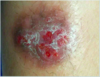
A 40-year-old man presents to the emergency department because of the infection shown. Medical history includes type 2 diabetes mellitus, hypertension, kidney transplantation 5 years ago, and a 10 pack-year history of smoking (former smoker). Temperature is 39.7°C (103.5°F) and blood pressure is 80/45 mmHg, white blood cell count is 25,000/μL. He is transferred to the surgical intensive care unit for fluid resuscitation and intravenous antibiotics prior to operative debridement in six hours. Which of the following is the strongest risk factor for mortality in this patient?
A) Age
B) Delay in operative debridement
C) History of kidney transplantation
D) History of smoking
E) Type 2 diabetes mellitus

The correct response is Option B.
Necrotizing fasciitis is a rapidly progressive soft-tissue infection. Patients usually present with systemic sepsis, fever, high leukocytosis (higher than 25,000), skin findings of edema with blue discoloration, weeping blisters and cellulitis. The more severe cases can present with multisystem organ failure and altered mental status. Polymicrobial infections are most common. Streptococcal species are isolated in more than 60% of polymicrobial infections. Other organisms identified include Staphylococcus aureus, Escherichia coli, Pseudomonas, Enterobacter, Klebsiella, Proteus, Bacteroides, Clostridium, and Peptostreptococcus.
Multiple studies have reported a mortality rate of approximately 20% from necrotizing fasciitis. Mortality is directly proportional to time of intervention. Delayed surgical debridement has been shown to significantly increase the mortality risk. After diagnostic delay, the most common pitfall in treatment is inadequacy and delay in surgical debridement.
Type 2 diabetes mellitus is incorrect. Comorbid conditions such as diabetes, vascular disease and venous insufficiency are very common in these patients. Diabetes specifically is associated with higher morbidity and mortality. Studies have shown that patients with diabetes have a higher chance of a negative outcome compared to patients without diabetes. However, it has not been shown to be the most severe risk factor associated with mortality.
Smoking is incorrect. Smoking is a risk factor for delayed healing, but there are no studies that show smoking alone to be a risk factor in the progression of necrotizing fasciitis.
After delay of operative debridement, immunosuppression is the second most significant risk factor for mortality. Patients with solid organ transplantation or undergoing treatment for hematologic malignancies are most at risk. Age has been reported as another risk factor of mortality in patients with necrotizing fasciitis. Studies have shown that extremes of age, younger than 1 year or older than 60 years, were associated with mortality, but age is not the strongest risk factor among the others reported.
A construction worker has an abscess of the palm of the nondominant hand after sustaining a puncture wound to the palm. In this patient, the midpalmar space is defined by which of the following boundaries?
(A) Flexor tendons, abductor pollicis muscle, superficial aponeurosis, and septum from the second metacarpal bone to the flexor digitorum profundus sheath
(B) Flexor tendons, metacarpal bone and interosseous fascia, septum from the third metacarpal to the flexor digitorum profundus sheath, and hypothenar eminence
(C) Flexor tendons, superficial palmar aponeurosis, and thenar and hypothenar eminences
(D) Flexor tendons, thenar eminence, septum from the second metacarpal bone to the flexor digitorum profundus tendon, and superficial aponeurosis
(E) Septum from the first metacarpal bone to the superficial aponeurosis, septum from the third metacarpal to the flexor tendon sheath, and lateral and medial edges of the abductor pollicis muscle
The correct response is Option B.
The midpalmar space is one potential site of infection of the palm; others include the subcutaneous tissue, tendon sheaths, and thenar and hypothenar eminences. The midpalmar space is located deep to the flexor tendon. It extends dorsally to the fascia over the second and third volar interossei and the third and fourth metacarpals.
The midpalmar space is bordered radially by a fascial septum extending from the third metacarpal to the flexor sheath of the flexor digitorum profundus tendon of the long finger, and ulnarly by the fascia of the hypothenar musculature. The proximal margin of the midpalmar space is a thin layer of fascia that lies just distal to the carpal canal. The distal margin of the midpalmar space is bordered by vertical septa of the palmar fascia, which extend almost to the web spaces.
In patients with infection of the midpalmar space, diagnosis is often delayed. Affected patients typically exhibit swelling of the dorsal aspect of the hand, loss of palmar concavity, and difficulty extending and flexing the fingers. Marked tenderness in the midpalmar area is characteristic, and cellulitis is often associated.
The thenar space is located radial to the vertical septum between the third metacarpal and the flexor digitorum profundus tendon of the long finger; it extends to the radial edge of the abductor pollicis brevis tendon. The hypothenar space contains the hypothenar muscles and is enveloped within the fascia of these muscles. It is bordered radially by a fascial septum extending from the fifth metacarpal bone to the palmar fascia.
For each clinical scenario, select the most appropriate pharmacologic agent (A–E): A 45-year-old man has a two-day history of pain and swelling of the proximal interphalangeal joint of the right index finger. Physical examination shows pain on passive motion of the affected joint and erythema and tenderness extending into the right hand. Gram’s stain of fluid aspirated from the joint shows gram-positive cocci.
A) Acyclovir
B) First-generation cephalosporin
C) Prednisone
D) Rifampin isoniazid
E) Third-generation cephalosporin
The correct answer is option B.
Septic arthritis may result from extension of an adjacent subcutaneous abscess or by intra-articular contamination caused by a laceration or puncture wound. The joint is a poorly vascularized potential space, favoring colonization. Early diagnosis and drainage are crucial to treatment, as a joint infection can progress rapidly to destruction of articular cartilage.
The two most common organisms that cause hand infections are Staphylococcus aureus and B-hemolytic streptococci. Minor staphylococcal and streptococcal infections are treated with first-generation cephalosporins. More significant infections of the interphalangeal joint should be performed through a midaxial incision. Neisseria gonorrhoeae usually manifests as a primary venereal infection. However, it can disseminate and sometimes present as a secondary hand infection, which is often confused with a purulent tenosynovitis or arthritis. It is important to distinguish gonococcal from pyogenic infection because, unlike a pyogenic infection, a gonococcal infection does not usually destroy tendon or articular cartilage. Therefore, incision, drainage, and debridement are unnecessary and should be avoided. Disseminated gonococcal infection is the most common cause of acute infectious arthritis in sexually active adults. A history or evidence of trauma are lacking. Fluid aspiration with Gram staining for gram-negative diplococci allows definitive diagnosis. Hospitalization and intravenous administration of a third-generation cephalosporin is recommended. Manifestations of Sweet syndrome can masquerade as acute hand infections. Sweet syndrome, originally described as an acute febrile neutrophilic dermatosis, belongs to a class of skin lesions that histologically have intense epidermal and/or dermal inflammatory infiltrate of neutrophils without evidence of infection or vasculitis. The lesions can erupt at sites of minor trauma. The clinical picture is consistent with infection initially. The unresponsiveness of these lesions to antimicrobial therapy and the lack of associated cellulitis is a clue to the diagnosis. The treatment of choice involves a tapering dose of corticosteroids. Herpetic whitlows are often confused with paronychia or felon and are treated mistakenly as such. Initial signs include intense pain and erythema of the fingertip, followed by edema and tenderness. A Tzanck smear of vesicular fluid may show multinucleated giant cells. Primary herpes simplex infections typically resolve without treatment within three weeks. Incision and drainage of herpetic whitlow is contraindicated because surgical treatment converts a closed wound to open and may result in a secondary bacterial infection or viral superinfection. To date, there have been no controlled studies that assess the efficacy of acyclovir for the treatment of herpetic whitlow, but case reports suggest that it both suppresses and decreases the length and severity of recurrent infections when taken orally.
A 45-year old male employed as a dishwasher presents with an 8 month history of redness and tenderness along his paronychial fold. He was treated on five different occasions with a 7 day course of oral antibiotics and antifungal agents without any improvement. The next step should be to:
A) Check his blood sugars
B) An eight week course of a broad spectrum intravenous antibiotic
C) Marsupialization
D) Removal of the nail plate and daily application of Betadine to the matrix
E) Recommend a change of jobs
The correct answer is option C.
This is an example of a chronic paronychial infection. There is usually no single causative organism hence long term antibiotics may not be successful. Although diabetes may be implicated, control of the blood sugars by itself will not be curative. Similarly, avoidance of maceration is important but not enough by itself. In this case Zook recommends a marsupialization of the nail fold ,which consists of excision an ellipse of skin proximal to the nail bed with secondary healing. Avoiding chronic water immersion and controlling abnormal blood glucose levels are appropriate measures but they will not by themselves result in a resolution of this chronic condition.
A 40-year-old woman is undergoing chemotherapy for metastatic lung cancer. During administration of her first dose of doxorubicin, she reports pain at the site of injection. The following day, physical examination shows the hand to be swollen and an ulcer measuring 2 × 3 cm is seen over the dorsum surrounded by an area of ischemia. Which of the following is the most appropriate immediate treatment?
A ) Administration of hyperbaric oxygen
B ) Application of cold packs
C ) Application of hot packs
D ) Application of topical dimethyl sulfoxide
E ) Immediate surgical excision and autografting
The correct response is Option D.
The specific treatment of an extravasation injury is dependent on the drug infused. Application of topical dimethyl sulfoxide has been advocated for the treatment of extravasation of anthracyclines and is supported by several studies.
The value of hyperbaric oxygen therapy has not been proven. In the case of doxorubicin extravasation injury, cold compresses may exacerbate the complication by venous constriction, which localizes the drug, whereas hot packs may cause vasodilatation with further extravasation. Inflammation and pain can be managed with anti-inflammatory analgesics.
Early excision is rarely performed without evidence of at least ulceration, and the main indication would then be for pain control. In the scenario described, an option would be early surgical debridement and delayed closure of the wound; however, some of the surrounding skin may heal. Thus, a conservative initial approach with later excision after 2 to 3 weeks is recommended since this will give a better cosmetic result.
All of the following factors are associated with an increased rate of amputation in the surgical treatment of diabetic patients with a hand infection except:
A) Renal failure
B) Deep infection
C) Insulin dependence
D) Gram-negative infection
E) Polymicrobial infection
The correct answer is option C.
A recent retrospective review of 45 patients with diabetes and surgically treated hand infections noted that insulin dependence, present in 31 patients, was not statistically related to a higher likelihood of amputation. Forty-six percent of the cultures were polymicrobial, which was associated with higher amputation rate. Other factors associated with a higher amputation rate were renal failure, deep infection, and gram-negative infection.
A 28-year-old, right-hand–dominant woman is brought to the emergency department 18 hours after sustaining a cat bite to the dorsum of the hand proximal to the fifth metacarpophalangeal (MCP) joint. Which of the following organisms is most likely to be cultured from this abscess?
A) Eikenella corrodens
B) Group A Streptococcus
C) Methicillin-resistant Staphylococcus aureus
D) Pasteurella multocida
E) Pseudomonas aeruginosa
The correct response is Option D.
Pasteurella multocida is a small, gram-negative coccobacillus that is frequently associated with infections caused by dog and/or cat bites. Local findings are consistent with infection including erythema, warmth, pain and tenderness, and fluctuance or purulent discharge. Delayed treatment may result in chronic deep-space infection and/or osteomyelitis. Treatment involves starting penicillin combined with local wound care as well as surgical incision and debridement if needed.
Methicillin-resistant Staphylococcus aureus (MRSA) is becoming more common in community-acquired hand infections, but is not typically associated with dog or cat bites. Eikenella corrodens is more commonly associated with infections occurring after human bites. Pseudomonas infection is often seen as a nosocomial infection that is very resistant to antibiotics. Group A Streptococcus is a common bacterial infection associated with strep throat.
A 45-year-old man is brought to the emergency department with a Gustilo IIIB tibial fracture that he sustained falling off a tractor in a pasture. Medical history shows no drug allergies. Administration of which of the following antibiotics is most appropriate in this patient?
A) Amoxicillin
B) Ceftriaxone
C) Ciprofloxacin
D) Clindamycin
E) Vancomycin
The correct response is Option B.
The most appropriate antibiotic prophylaxis for this patient with a Gustilo grade III fracture is a third generation cephalosporin. Although much debate exists regarding antibiotic prophylaxis in open tibial fractures, it is generally accepted that antibiotic prophylaxis reduces the rate of infection. When antibiotic prophylaxis is not used, infection occurs in approximately 24% of open fractures. Thus, selecting the appropriate antibiotic, as well as duration, is of utmost importance. Antibiotic prophylaxis should be administered as soon as possible after injury and should be limited to a 72-hour course. In general, broad-spectrum antibiotics and multiple antibiotics should be avoided because they have been shown to increase the risk of nosocomial infections, including pneumonia. Of the antibiotics listed, the most appropriate choice for a patient with no drug allergies is ceftriaxone. Clindamycin and vancomycin should be reserved for cases of true penicillin allergy. Ciprofloxacin alone has been shown to be inferior to prevent infection after open tibial fractures.

A 37-year-old man comes to the emergency department 4 hours after he sustained a human bite wound to the nondominant hand. Examination shows no erythema, swelling, purulent drainage, lymphangitis, or fever. Exploration of the wound shows no joint or tendon involvement. Debridement and irrigation of the wound is performed. Which of the following is the most appropriate next step in management?
A) Administration of amoxicillin-clavulanate 875/125 mg twice daily
B) Administration of clindamycin 450 mg three times daily
C) Administration of doxycycline 100 mg twice daily
D) Administration of trimethoprim-sulfamethoxazole 1 double-strength tablet twice daily
E) Observation
The correct response is Option A.
A prospective, randomized study has shown that antibiotic prophylaxis is superior to placebo in decreasing infections after human bites that are less than 24 hours old. The most common pathogens in human bite wounds are S aureus, E corrodens, H influenzae, and beta lactamase-producing anaerobic bacteria. Eikenella species are resistant to clindamycin. Meanwhile, doxycycline and trimethoprim-sulfamethoxazole are not effective against anaerobes. Of the options mentioned, only amoxicillin-clavulanate has good activity against all common oral pathogens.
A 25-year-old man is brought to the emergency department four hours after being bitten by a raccoon. He has not been previously vaccinated for rabies. In addition to irrigation of the wound, which of the following is the most appropriate management?
The correct response is Option D.
In a patient who has been bitten by a potentially rabid animal and who has not been previously vaccinated, management should include wound care and administration of both rabies immune globulin (RIG) and rabies vaccine. Because rabies incubation periods of more than one year have been reported in humans, the prophylactic regimen should be initiated immediately in any person who has been bitten by an animal with suspected or proven rabies regardless of the length of the delay, as long as clinical signs of rabies are not present. Studies have shown that a regimen of one dose of RIG and five doses of human diploid cell vaccine (HDCV) over a 28-day period is a safe treatment protocol that induces an excellent antibody response.
Immediate, thorough washing of all bite wounds and scratches with soap and water and irrigation with a virucidal agent (such as a povidone-iodine solution) are also important for preventing rabies. Experimental animal studies have shown that thorough wound cleansing alone without other postexposure prophylaxis markedly decreased the likelihood of rabies. In addition, tetanus prophylaxis and measures to control bacterial infection should be administered as indicated. Suturing of large wounds should be based on cosmetic factors and the potential for bacterial infection.
Prophylactic administration of both passive antibody and vaccine is indicated in all exposed patients except for those who have previously received complete vaccination regimens (preexposure or postexposure) with a cell culture vaccine or those persons who have been vaccinated with other types of vaccines and have had documented rabies antibody titers. Instead, these persons should receive the vaccine only. This combination of RIG and vaccine is also recommended for patients who have been exposed to rabies without specifically being bitten.

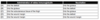
A 55-year-old woman has had pain, swelling, and erythema of the left arm for the past 24 hours. She underwent mastectomy and axillary lymph node dissection on the left four years ago. On examination, she is afebrile. Laboratory studies show a leukocyte count that is within normal limits.
Which of the following is the most appropriate management?
(A) Lymphatic massage
(B) Application of a compression bandage and elevation of the extremity
(C) Topical application of an antibiotic
(D) Intravenous administration of an antibiotic
(E) Incision and drainage
The correct response is Option D.
In this patient who has had the spontaneous onset of cellulitis of the arm after undergoing axillary lymph node dissection, the most appropriate management is intravenous administration of an antistreptococcal antibiotic. Fever and leukocytosis are typically associated with cellulitis but are not required to make the diagnosis, as many of these patients will be afebrile and will not have an increased leukocyte count or absolute neutrophil count on serologic testing. Anti-streptolysin O titer may be positive.
Although lymphatic massage and compression and elevation of the extremity are useful in controlling the lymphedema associated with lymph node dissection, these measures will not treat cellulitis. Antibiotic therapy should not be based on the results of blood or tissue aspirate cultures because these often do not yield any growth. Topical application of an antibiotic will not effectively treat cellulitis. Incision and drainage of the affected site is not indicated.
A 9-year-old boy is brought to the emergency department because he has nausea and vomiting as well as pain in the left hand one hour after he sustained a snakebite during a camping trip. Physical examination shows fang marks on the left thumb and swelling of the distal aspect of the forearm. Sensation is intact and no ecchymosis is noted. Which of the following is the most appropriate management?
(A) Elevation of the extremity and application of a tourniquet
(B) Fluid resuscitation with normal saline
(C) Administration of antivenin after skin testing with dilute horse serum
(D) Immediate cryotherapy to the affected area of the hand
(E) Measurement of compartment pressures and subsequent fasciotomy
The correct response is Option C.
In this clinical scenario of a snakebite to the upper extremity, the patient meets criteria for moderate envenomation, which can also yield orthostatic changes and mild coagulation parameter changes. Guidelines for management include the administration of 10 to 20 vials of antivenin after skin testing with horse serum for possible hypersensitivity reaction. Criteria for minimal envenomation include fang marks, local swelling or pain, and no systemic reaction; therapy includes delivery of up to five vials of antivenin. Severe envenomation can produce subcutaneous ecchymosis, marked swelling of the extremity, coagulopathy, shock, and compartment syndrome; therapy includes delivery of 20 or more vials of antivenin (without delaying for skin testing), resuscitation with correction of acidosis and coagulopathy, and fasciotomy for compartment pressures greater than 30 mmHg or worsening findings on neurologic examination.
Tourniquets and cryotherapy, although used in the past, are controversial and may be associated with increased tissue damage.
Resuscitation should be performed with lactated Ringer’s solution. Normal saline is contraindicated because this solution will exacerbate metabolic acidosis due to its high chloride load (154 mEq/l).
In a series of 107 patients with pit viper snakebites managed at a university teaching hospital in the southeastern U.S., 27% of patients underwent surgical debridement and 4% of patients required fasciotomies. Antivenin was administered to 34 patients, and serum sickness developed in nine patients. Coagulopathy was present in 4% of patients, and no deaths were reported. Copperhead bites accounted for 68% of all envenomations.
A commercial fisherman has restarted his business on the Mississippi Gulf Coast. He was too busy to come to clinic last month when he was attacked by a crab caught in his net. On exam, a puncture wound is present in his left palm with surrounding erythema. No drainage is present. There are absent Kanavel’s signs. Cultures and I & D of the mid palmar space are done. The organism most likely:
A) is mycobacterium tuberculi
B) is negative on Ziehl-Neelsen staining
C) histologically has noncaseating granulomas
D) must be cultured in Löwenstein-Jensen medium at 20°
E) takes several days to treat with systemic agents
The correct answer is option C.
The organism most likely involved is atypical mycobacteria, mycobacterium marinum. It histologically has noncaseating granulomas and stains positive on Ziehl-Neelsen staining. It is grown for four to six weeks on Löwenstein-Jensen medium at 30°C. Several months of treatments are required.
A 55-year-old man undergoes microsurgical replantation of an amputated ear. There is venous congestion, and leeches are applied. This patient is at risk for infection by which of the following organisms?
A) Actinobacillus lignieresii
B) Aeromonas hydrophila
C) Eikenella corrodens
D) Pasteurella canis
The correct response is Option B.
Aeromonas hydrophila is an organism present in the leech species Hirudo medicinalis gastrointestinal tract that can lead to an infection if used medicinally. In this patient with venous congestion and application of leeches, antibiotic prophylaxis is recommended with fluoroquinolones, tetracycline, or trimethoprim-sulfamethoxazole.
Actinobacillus lignieresii is seen in horse bites, Pasteurella canis in dog bites, and Eikenella corrodens in human bites.
In a recent review of ear reattachment methods, a variety of approaches have been used including microsurgical reattachment, burying of the part in a subcutaneous pocket, periauricular tissue flaps for coverage of the part, and direct reattachment as a composite graft. Microsurgical replantation is associated with the best aesthetic outcome even if venous anastomosis is not possible and leeching is necessary.
A 15-year-old girl comes to the office because of a 1-day history of infection of the right index finger. Physical examination shows the tip of the finger is tender and swollen over the pulp. There is no history of trauma. Which of the following organisms is the most likely cause of this patient’s condition?
A) Candida albicans
B) Eikenella corrodens
C) Listeria monocytogenes
D) Pasteurella multocida
E) Staphyloccus aureus
The correct response is Option E.
Staphylococcus is still the most common organism in hand infections. The most common in felons is Staphylococcus aureus. Methicillin-resistant Staphylococcus aureus community-acquired (MRSA-CA) infections are now the most predominant strain in hand infections, comprising 60% of Staphylococcus aureus infections.
Pasteurella multocida should be considered with most animal bites, although it is most common with cat bites. Eikenella corrodensis associated with human bites. There is no history of bites in this case.
Listeria monocytogenes has been reported in flexor tenosynovitis in immunocompromised patients.
Candida albicans is usually associated with chronic paronychia.
Which of the following is the most common causative organism of infectious folliculitis?
(A) Peptostreptococcus anaerobius
(B) Staphylococcus aureus
(C) Staphylococcus epidermidis
(D) Streptococcus milleri
(E) Streptococcus pyogenes
The correct response in Option B.
Staphylococcal folliculitis is the most common form of infectious folliculitis. One or more pustules may appear, usually without fever or other systemic symptoms, on any body surface. Staphylococcal folliculitis may occur because of injury, abrasion, or nearby surgical wounds or draining abscesses. The two gram-positive cocci, Staphylococcus aureus and Streptococcus pyogenes (group A), account for the majority of skin and soft tissue infections. The streptococci are secondary invaders of traumatic skin lesions and cause impetigo, erysipelas, cellulitis, and lymphangitis. S. aureus invades skin and causes impetigo, folliculitis, cellulitis, and furuncles. Elaboration of toxins by S. aureus causes the lesions of bullous impetigo and staphylococcal scalded skin syndrome.
A 25-year-old man who is a soldier from Afghanistan is evaluated because of deep frostbite of the right hand after being in the field for 36 hours. Rewarming is performed in the field. He is transferred to a hospital for further evaluation. Physical examination shows hemorrhagic blisters and eschar formation on the hand, erythema of the surrounding area, and streaking up the forearm. Which of the following is the most appropriate next step in management?
A ) Administration of dextran
B ) Administration of penicillin
C ) Hyperbaric oxygen therapy
D ) Intra-arterial injection of reserpine
E ) Observation
The correct response is Option B.
Field management for frostbite includes rapid rewarming of the affected area with circulating water at 104 to 107.6 °F (40 to 42 °C) for a period of 15 to 30 minutes, protection from mechanical trauma, and appropriate analgesia.
Next steps in management include elevation, antitetanus prophylaxis, debridement of clear blisters, leaving hemorrhagic blisters intact, and application of aloe vera. Penicillin should be administered for cellulitis.
Adjuvant therapies can include anticoagulation, thrombolytics, hyperbaric oxygen, and sympathetic blockade; however, data to support these therapies are scant and equivocal at best. Definitive surgical amputation should be delayed for at least 3 weeks to allow for tissues to demarcate, in terms of viability.
To drain a thenar space infection, the dissection is carried out:
A) volar to the abductor pollicis brevis muscle
B) ulnar to the vertical septum between the third metacarpal and long finger profundus tendon
C) volar to the opponens pollicis muscle
D) volar to the adductor pollicis muscle
E) volar to the flexor pollicis longus tendon
The correct answer is option D.
The dorsal border of the thenar space is the adductor fascia, hence drainage of the thenar space entails dissection volar to that muscle. The thenar space is located radial to the vertical septum between the third metacarpal and the long finger profundus and extends to the lateral edge of the adductor pollicis. The space is bounded anteriorly by the thumb and index flexor tendons, posteriorly by the fascia over the adductor pollicis, radially by the thenar intermuscular septum and ulnarly by the midpalmar oblique septum. The abductor and opponens pollicis muscles are superficial (volar) to the thenar space.

Verruca vulgaris (common wart) and verruca plana (flat wart) are similar in which way?
A) Rate of occurrence
B) Likelihood of spontaneous resolution
C) Pathologic appearance
D) Risk of transforming to carcinoma
E) Human papilloma virus etiology
The correct answer is option E.
Warts are more common in childhood. The rate of occurrence of common to plane warts is 20 to 1. Both can spontaneously resolve but the plana type is more likely to do so. The pathologic findings are different. Both have koilocytes, large keratinocytes with eccentric nuclei and perinuclear halo. The verruca plana lack parakeratosis and papillomatosis which are present in the vulgaris. Transformation to carcinoma has been reported with verruca vulgaris.
Persons with immunosuppression are at increased risk for this change. Both forms are caused by epidermal infection with the HPV virus, the common wart from HPV types 1, 2, 4, and 7, and the plane wart from HPV types 3, 10, 27, and 41.