Urogen HARC Lectures Flashcards
(83 cards)
1
Q

A

2
Q

A

3
Q

A

4
Q

A

5
Q

A

6
Q

A

7
Q

A

8
Q

A

9
Q

A

10
Q
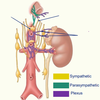
- Kidneys
- Renal Plexus Autonomic
- Sympathetic (T10-T11)
A
- Coeliac ganglion & plexus
- Aorticorenal ganglion
- Least splanchnic nerve
- First lumbar splanchnic nerve
11
Q
- Kidneys
- Renal Plexus Autonomic
- Parasympathetic
A
• Posterior Vagal Trunk (Vagus Nerve)
12
Q
- Kidneys
- Renal Plexus Autonomic
- Sensory (Visceral Afferents)
A
- Conveyed to CNS via sympathetic fibres
- Referred pain at T10-T11
13
Q
A

14
Q
Innervation
- Adrenal Glands
- Renal Plexus
- Sympathetic (T10-L1)
A
- Coeliac plexus and greater splanchnic nerves.
- Coeliac ganglion
- Unusually, synapse occurs in medulla
- Promotes secretion of adrenaline and noradrenaline from the medulla into the bloodstream
15
Q
What are the ureter lined with?
A
Urothelium
16
Q
What is the action called when the ureters passes urine from kidneys to bladder?
A
Peristaltic action
17
Q

A

18
Q
• Ureteric plexus

A
- Branches from three plexuses
- Renal & aortic (Upper)
- Superior hypogastric (Intermediate)
- Inferior hypogastric (Lower)
19
Q
What are the three points of ureteric constriction?
A
- Ureteropelvic junction
- Pelvic brim - As it crosses the common iliac a.
- Vesicoureteral junction
20
Q
What is the common site of lodged kidney stones?
A
Ureter
21
Q
What are the causes of Urinary Tract Stones?
A
- Dehydration, diet and disease
- Urine saturation with salts and varied pH
- Constriction sites

22
Q
What are the symptoms of Urinary Tract Stones?
A
Renal Colic
- Haematuria
- Urinary urgency
23
Q
Urinary Tract Stones (Calculi) are classified based on position. What are these positions?
A
- Nephrolithiasis (Kidney)
- Uretrolithiass (Ureter)
- Cystolithiasis (Bladder)
24
Q
What are the complications of urinary tract stones?
A
- Urinary obstruction
- Infection
- Renal failure
25
•Staghorn Calculus
Staghorn calculi refer to branched stones that fill all or part of the renal pelvis and branch into several or all of the calyces. They are most often composed of struvite (magnesium ammonium phosphate) and/or calcium carbonate apatite.
26


27
In the male urethra there a four parts what are they?
* Pre-prostatic 1 → Bladder to prostate
* Prostatic 2 → Length of the prostate
* Membranous (Muscular) 3 → Deep perineal pouch
* Penile/Spongy 4 → Deep perineal pouch to external urethral orifice
28

* Pre-prostatic 1
* Prostatic 2
* Membranous (Muscular) 3
* Penile/Spongy 4
29
Urethra Catheterisation
* Allows bladder drainage if patient cannot urinate.
* Biological sex of the patient must be considered - Differences in urethral length and course
* If urethra cannot be catheterised, bladder can be drained via suprapubic catheter
30
What forms the pelvic floor?
• Levator ani and coccygeus m
31
Pelvic floor separates the ____ \_\_\_\_\_ from \_\_\_\_\_\_
Pelvic floor separates the **pelvic cavity** from **perineum**
32
The pelvic FLoor
* Provides supports and prevents prolapsing of pelvic viscera - Bladder, uterus and rectum
* Separately identifying parts of levator ani is difficult due to fibres blending together.
33


34
What can cause dysfunction to the pelvic floor?
• Trauma, age, pregnancy and hormonal status
35
What can the dysfunction of pelvic floor lead to?
rectal/urinary incontinence or organ prolapse i.e bladder/uterus
36
What is Ischioanal fossa
* Wedge shaped, fat filled space
* Either side of anal canal and external anal sphincter
* Expansion of anal canal and accommodation during childbirth

37
Ischioanal abcesses
* Ischioanal fossa can become infected
* Lateral spread from anal canal
* Poor blood supply causes predisposition
* Infection can spread between different regions
* Named based on position
38


39
Where is the vesicouterine pouch?
between the bladder and uterus
40
Where is the Rectouterine pouch?
Between rectum and uterus
Most inferior aspect
Point of fluid accumulation
41


42
What does the supenspory ligament of the ovary contain?
* Ovarian vessels & nerves
* Lymphatics
43
What is the ovum pathway?

1. Fimbriae
2. Infundibulum
3. Ampulla
4. Isthmus
5. Intramural
44
Uterine Tubes
* 8-10cm long
* Suspended in upper part of the broad ligament (mesosalpinx)
45
What does salpinx mean?
tube
46
Properties of Uterus

* Pear shaped
* 7/8cm long
* Cervical canal (Cervix)
- Internal os: Communicates with uterine cavity
- External os: Communicates with vaginal canal, Changes shape postpartum, Circular to ‘slit-like
47
Properties of Vagina
* 8-9cm long
* Surrounds the cervix
* Extends between the vulva (external genitalia) and uterus
* Passes through the pelvic floor - Opens into vestibular area
* Upper half of vagina lies above pelvic floor, lower half below it.

48
What is this a picture of?

Internal view of vaginal canal around cervix using speculum
49
What is Culdocentesis?
Culdocentesis is a procedure in which peritoneal fluid is obtained from the cul de sac of a female patient. It involves the introduction of a spinal needle through the vaginal wall into the peritoneal space of the pouch of Douglas
Draining rectouterine pouch using the posterior fornix for access
50


51
Parietal periotneum=
Lining the walls of the abdominopelvic cavity
52
Visceral Peritoneum=
Covering the organs The bladder (labelled) is hidden by peritoneal covering
53
Broad Ligament =
Due to the shape of the female reproductive tract, the peritoneum drapes over it forming a double layer of peritoneum. Encas
54


55
What are the three parts to the braod ligament ?
* Mesosalpinx
* Mesovarium
* Mesometrium
56


57


58


59
What is the major artery supplying the female reproductive system?
Internal iliac a.
60
Innervation


61
Testes and scrotum
* Testes suspended in scrotum by spermatic cord (External) - Keeps testes 3 degrees lower than body temperature for spermatogenesis
* Left usually lower → Descend first
* Firm and mobile – limited rotation → Testicular torsion
* Septum divides scrotum into left and right
62


63
Testes and Scrotum
Layers:

* Skin
* Dartos fascia
* External spermatic fascia
* Cremasteric fascia (Muscle)
* Internal spermatic fascia
* Tunica Vaginalis (Two layer
64
What is the function of accessory glands? and what are the accessory glands?
* Produce seminal fluid to carry sperm - Nutritive and protective
* Prostate (Singular) - Inferior to the bladder
* Seminal Vesicles (Paired) - Posterior surface of the bladder
* Bulbourethral Glands (Paired) - Deep perineal pouch
65


66


67
Seminal Vesicle
* Seminal Vesicle (Paired)
* Posterior to the bladder
* Produces ~70% seminal fluid
* Nourishment
* Alkaline – protects against low pH in vagina
68
•Bulbourethral gland (Paired)
* Deep perineal pouch
* Produces pre-ejaculatory fluid
* Mucus rich – lubrication and protection
* Empties into spongy urethra
69


70
Ductus deferens
* Muscular tube carrying spermatozoa from the testis - Continuation from epididymal tail
* Primary component of spermatic cord passing in inguinal canal
* Terminates by joining with the seminal vesicle duct to form the ejaculatory duct
71
Vasculature of the male reproductive system


72
Innervation of male reproductive


73
What is the inguinal Canal
* Oblique passage through the layers of the abdominal wall in both males and females
* Created by the dragging of structures through the incomplete abdominal wall
74


75
Formation of Inguinal canal (step 1)
* Abdominal wall same structure in foetus & adult
* Testes need to be external
* Gonad anchored to the skin (labioscrotal swelling) by gubernaculum
* Inguinal canal created first, gonad follows
76
Formation of Inguinal canal (step 2)
* Processus vaginalis forms outpouching of peritoneum
* Takes all the layers of the wall with it as it pushes through
* Gonad pulled along after
* Pathway through the wall is inguinal canal
77
Formation of Inguinal canal (step 3)
* Labioscrotal swelling becomes scrotal sac (scrotum)
* Upon gonadal descent, “layers” of the wall become “coverings” of spermatic cord and testes
* Gubernaculum becomes scrotal ligament\*
78
Gonadal descent
* Similar process in male and female
* Male gonad descends into the scrotum by 9 months development
- Creates a larger inguinal canal
- Cryptorchidism – Incomplete descent
• Female gonad only descends as far as pelvic cavity
- Gubernaculum attached to labioscrotal swelling becomes ovarian ligament and round ligament of the uterus -
Smaller inguinal canal
79


80


81


82


83




