CVS Diseases 2 Flashcards
(169 cards)
What is Anemia?
Anemia is a simply a reduction in haem and/ or globin
Properties to Hb
- Consists of haem and globin
- 4 polypeptide globin chains
- Each chain is complexed to a haem molecule
- Haem is an iron containing compound
2 beta chains and 2 alpha chains
Classification of Anemia
- Anaemia is classified as:
- Men: Hb <130/L
- Women: Hb <120/L
- Further classification based on mean corpuscular volume (MCV) – what is this?
- In simple terms, the average size of the total red blood cells.
Examples of Microcytic anaemia?
Iron Deficiency
Thalassaemia
Anemia of Chronic disease
Sideroblastic anemia
Lead poisoning
Examples of Normocytic anaemia?
Acute blood loss
Haemolytic anaemia
Anaemia of Chronic disease
Chronic Kidney Disease
Aplastic anaemia
Examples of Macrocytic anaemia?
B12 deficiency
Folate deficiency
alcohol
Liver dosease
Hypothyroidism
Signs and symptoms of anaemia?
Fatigue
Tachycardia
SOB on exertion
Tachypnoea
Chest pain
Hypotension
Palpitations
Pallor
Red flags for Anaemia?
•Weight loss, anorexia, night sweats, lymphadenopathy
What is iron deficiency Anaemia?
Reduced intake, increased requirement or increased loss of iron
Features of iron deficiency?
Glossitis
Angular stomatisits/chelitis
Koilonychia
Pica
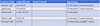
Ix for Iron deficiency Anaemia

What is Thalassemia?
Prevalent in what areas?
Definition: Autosomal recessive haemoglobinopathy. Inherited blood disorder causing the body to make fewer healthy red blood cells with les hb
•Haemoglobinopathy: Impaired globin chain synthesis
Prevalent in areas of malaria
- Alpha: Asia and Africa
- Beta: Asia, Mediterranean and Middle East
Patho of thalassemia
Alpha: 4 alleles on chromosome 16 that code for alpha globin – the more deletions, the worse the anaemia.
•4 deletions = hydrops fetalis- not compatible with life
Beta: 2 alleles on chromosome 11 that code for beta globin. Mutated alleles can either produce less beat globin or no beta globin. The worse the mutations, the worse the anaemia.
Clinical features of thalassaemia?

What is anaemia of chronic disease?
What is the causes?
Anaemia due to an inflammatory mediated reduction in RBC production
Can be microcytic or normocytic
Causes:
- Autoimmune disorders: e.g. RA
- Chronic infection
- Chronic disease: e.g. CKD, HF
- Malignancy
- Major trauma
What is the difference between iron deficiency anemia and anemia of chronic disease?
In iron-deficiency anemia, the TIBC is higher than 400–450 mcg/dL because stores are low. In anemia of chronic disease, the TIBC is usually below normal because the iron stores are elevated
A total iron-binding capacity (TIBC) test measures the blood’s ability to attach itself to iron and transport it around the body. A transferrin test is similar. If you have iron deficiency (a lack of iron in your blood), your iron level will be low but your TIBC will be high.
What is sideroblastic anaemia?
Causes?
•Rare
Definition: Anaemia due to defective heam synthesis within the mitochondria.
Causes:
- Lead poisoning
- Vitamin B6 deficiency
- Congenital: X-linked recessive enzyme deficiency
- Chronic Alcoholism
Signs in normocytic anaemia
think of 3As and 2Hs
- A – Acute blood loss
- A – Anaemia of Chronic Disease
- A – Aplastic Anaemia
- H – Haemolytic Anaemia
- H – Hypothyroidism (can also be macrocytic)
What happens in normocytic anaemia?
- Normocytic anaemias: Either increased destruction of RBCs or reduced production of RBCs.
- Reticular count is used to distinguish the two
- Reduced production – reticular count is low (failure of bone marrow )
- Increased destruction – Bone marrow is working fine – compensation from haemolysis so increased reticulocytes
What is hereditary spherocytosis?
- Inherited defect in the RBC membrane proteins leading to a haemolytic anaemia
- Usually autosomal dominant
- Extra features:
- Neonatal jaundice, splenomegaly, gallstones
- Ix: Increased reticulocytes
What is sickle cell disease?
- Autosomal recessive mutation in the Hb beta chain at position 6 (glutamic acid to valine)
- 2 alleles code for the beta chain
- Sickle cell disease: 2 abnormal alleles
- Sickle cell trait: 1 abnormal allels
- Sickle cell crisis: Acute manifestation of sickle cell disease

Patho of sickle cell?
- HBS: Crystallises and is insoluble at low PaO2
- This causes sickling of the RBC
- Extra features: jaundice, failure to thrive, frontal bossing
What is G6PD deficiency?
- Inherited X-linked deficiency resulting in a haemolytic anaemia.
- Results in a reduced half-life of RBCs (<120days)
- G6PD is required by cells to prevent them from damage by oxidation.
- Red cells are under constant stress by oxidants as oxyhaemoglobin is converted to deoxyhaemoglobin
G6PD deficiency is an inherited condition. It is when the body doesn’t have enough of an enzyme called G6PD (glucose-6-phosphate dehydrogenase). This enzyme helps red blood cells work correctly. A lack of this enzyme can cause hemolytic anemia. This is when the red blood cells break down faster than they are made.
What is autoimmune haemolytic anaemia?
- Antibody mediated destruction of RBCs
- Divided into cold or warm depending on what temperature the antibodies bind to RBCs the best.
- Warm: IgG binds to RBCs; Cold: IgM binds to RBCs.
- Associated with Autoimmune conditions, infections and drugs
- Causes extravascular haemolysis (warm) and extra/intravascular haemolysis (cold)
- Warm: SLE, CLL, Drugs e.g. penicillin
- Cold: M.pneumonia, EBV
- Warm vs cold? Coombs test (normally direct)