CR Revision 7 Flashcards
(44 cards)
what are the nasopharynx, oropharynx and laryngopharynx innervated by?
nasopharynx: CN V2
oropharynx: CN IX
laryngopharynx: CN X
what happens to the epiglottis when you swallow?
larynx moves up, towards base of tongue and hyoid bone: makes the epiglottis close over the laryngeal inlet to prevent aspiration into trachea

which ligament connect the hyoid bone and thyroid? - what is this covered by?
which ligament connects the cricoid and thyroid cartilage?
where does ithe internal laryngeal nerve and superior laryngeal artery enter larnyx?
Hyoid bone and thyroid are joined by thyrohyoid ligament, covered by a thyrohyoid membrane.
Internal laryngeal nerve and superior laryngeal artery come through this ligament/membrane
Between the cricoid and thyroid cartilages: Crico-thyroid ligament



which nerve controls most of the muscles of larynx? - which muscle does it not innervate?

most motor to muscles controlled by the recurrent laryngeal nerve - PHONATION
sensory innervation to area below vocal cords
doesnt innervate motor control for cricothyroid (comes from superior laryngeal nerve)

Which nerves can be damaged during laryngeal surgery? [2]
Explain the effect of each nerve damage [2]
Could be caused by surgery to the neck (particularly thyroid), Tumours (often thyroid) leading to compressing nerve, trauma or viral infection, thyroidectomy due to tumour/hyperthyroidism.
Recurrent laryngeal injury will result in paralysis of all intrinsic muscles except cricothyroid which will cause problems with phonation. Vocal cord paralysis means you will be unable to abduct laterally, leading to hoarseness (if this damage only occurs on one side) or aphonia (if the damage is bilateral).
Stridor or respiratory distress can happen if acute due to blockage of the airflow which your body is not able to adapt to. This is due to paralysis of intrinsic muscles.
External laryngeal will lead to paralysis of cricothyroid preventing higher pitched phonation. This leads to Weak voice with low pitch, reduced range so your voice easily tires
The larynx lies in which vertebral layers? [1]
C3-C6
The vocal cords attach anteriorly to which cartilage?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilage
Thyroid cartilage
The vocal cords attach anteriorly to which cartilage?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilage
Thyroid cartilage

During swallowing, epiglottis [] and moves [] to close off the larynx
During swallowing, epiglottis flattens and moves posteriorly to close off the larynx to prevent aspiration of food
Which of the following is the only complete cartilaginous ring within the upper airway?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilage
Thyroid cartilage
Which of the following is the only complete cartilaginous ring within the upper airway?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilage
Thyroid cartilage
What does the cricoid cartilage attach to:
Anteriorly?
Posteriorly?
Anteriorly: Cricothyroid membrane
Posteriorly: Inferior horns of thyroid cartilage + paired arytenoid cartilages
The vocal cords attach posteriorly to which of the following?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilage
Thyroid cartilage
The vocal cords attach posteriorly to which of the following?
Cricoid cartilage
Cuneiform cartilage
Epiglottis
Arytenoid cartilages
Thyroid cartilage

What is the sensory innervation to all muscles below the vocal cords? [1]
What is the sensory innervation to all muscles above the vocal cords? [1]
What is the motor innervation to all muscles of the larynx except for the cricothryroid? [1]
What is the motor innervation for the cricothryroid? [1]
What is the sensory innervation to all muscles below the vocal cords? [1]
Recurrent laryngeal nerve
What is the sensory innervation to all muscles above the vocal cords? [1]
Internal laryngeal nerve
What is the motor innervation to all muscles of the larynx except for the cricothryroid? [1]
Recurrent laryngeal nerve
What is the motor innervation for the cricothryroid? [1]
External laryngeal nerve
Which nerve is responsible for the opening the rima glottidis to refine sounds during phonation? [1]
Recurrent laryngeal nerve
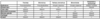
What are the effects of superior, internal and external branch palsies? [A&B]

A: reduced gag reflex
B: reduced range of pitch
Palsy to which nerve causes reduced gag reflex?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes reduced gag reflex?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve
Palsy to which nerve causes reduced range of pitch?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes reduced range of pitch?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes horseness of voice?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes horseness of voice?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes loss of phonation?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
Palsy to which nerve causes loss of phonation?
Superior laryngeal nerve, external branch
Superior laryngeal nerve, internal branch
Recurrent layngeal nerve, bilateral damage
Recurrent layngeal nerve, unilateral damage
How do you calculate forced vital capacity? [1]
Forced vital capacity (maximum volume of air air forcibly exhaled out of your lungs after a deep full breath) = Inspiratory reserve volime + tidal volume + expiratory reserve volume

DCLO technique
Rapid inhalation of CO/Helium to TLC → Breath hold (10 sec) → unforced exhalation (< 4 sec)
Sample: exhaled breath
Explain what DCLO measures [1]
How do you calculate DCLO? [1]
What is a normal DLCO value? [1]
DCLO: a measurement to assess the ability of the lungs to transfer gas from inspired air to the bloodstream. Carbon monoxide has a high affinity for hemoglobin, and it follows the same pathway as that of oxygen to finally bind with hemoglobin. Inhaled carbon monoxide is used for this test due to its high affinity for hemoglobin (200-250 times that of oxygen).
above 75 % of predicted value

Why is DCLO raised in asthma Ptx?
Expiration is decreased, so air is trapped in the lungs.
Have a lot of blood vessel recruitment
Name 3 & explain 3 excercise tests
Assess pre-operative fitness/fitness state/extent of breathlessness/benefit of oxygen therapy