Anatomy - Midgut and Hindgut Flashcards
Most of the small bowel is […]peritoneal
Intra
What is the mesentery?
The double-layer of peritoneum that keeps the loops of small bowel attached to the posterior abdominal wall and allows for them to move with digestion
The blood supply to the midgut comes from the […] which runs between […].
Superior mesenteric artery
Mysentery
To expose it, you would remove one layer of mesentery


How can you distinguish the jejunum from the ileum?

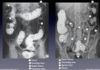
How can you distinguish between jejunum and ileum on CT?

Note that the jejunum, which is more proximal, can be identified by its more numerous plicae circulares, or transverse folds, and the ileum is comparatively smoother



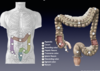
What parts of the large intestine are part of the midgut?
What parts of the large intestine are part of the hindgut?
Cecum, ascending colon, and the first 2/3 of the transverse colon
Last 1/3 of transverse colon, descending colon, sigmoid colon, rectum
The ascending colon is […]peritoneal, while the transverse colon is […]peritoneal.
Retro
Intra


The small and large intestines intersect at the […]
Ileocecal junction
The appendix is an outpouching of the […]
Cecum
Why can the appendix can be found in a number of positions relative to the ileocecal junction?

Fve examples of an ICJ + appendix located in an atypical place.
An atypical location of the cecum can occur as a result of malrotation of the GI tract during development (not enough or rotated too much)
What are the 3 GI tract constrictions in the small bowel?
What clinical significance do they have?
Pylorus and duodenum = foregut
Others = midgut

How can you ID the duodenojejunal flexure?
The duodenojejunal flexure can be identified by its attachment to the suspensory ligament of the duodenum, sometimes called the Ligament of Treitz. The suspensory ligament of the duodenum, which attaches the duodenaljejunal flexure to the esophagus, provides a landmark for surgeons demarcating what portion of the small intestine is the duodenum and which is the jejunum.


The distal duodenum, jejunum and ileum receive blood from the […].
SMA
Where does the SMA branch off the abdominal aorta?
The SMA branches off the aorta just inferior to the celiac trunk, generally just inferior to the pancreas.
What is the first branch of the SMA and what part of the midgut do they supply?
The first branch of the SMA is the inferior pancreaticoduodenal arteries, which supply the pancreas and duodenum. They anastomose with the superior pancreaticoduodenal arteries, branches of the celiac trunk.
The SMA supplies blood to what structures?
Part of duodenum, all jejunum and ileum, pancreas, ileocecal junction, appendix, ascending colon, transverse colon




Drainage of the midgut is via the […], which joins the […] to form the […]
Superior mesenteric vein
Splenic vein
Portal vein
What is the abdominal portal system? How is blood from the abdomen drained differently than blood from the body wall, pelvic organs, and lower limbs?
Portal system drains the GI tract by sending blood through the liver to be filtered. Systemic blood from the body wall, pelvic organs, and lower limbs is drained through the IVC and skips the liver.
The hindgut is drained by the […], which generally drains into the […] on the […] side of the body
Inferior mesenteric vein
Splenic vein
Left

Parasympathetic innervation to the midgut is carried in the vagus nerve. Sympathetic innervation comes from the lesser splanchnic nerves, which synapse at the superior mesenteric ganglion. The superior mesenteric plexus carries postsynaptic sympathetic and parasympathetic innervation to the midgut.








What is Volvulus?
One function of the mesentery is to keep the small intestine from tying itself into a knot by providing an attachment to the posterior body wall. However, if the mesentery doesn’t develop properly or if it is surgically altered, the small intestine can loop itself into a knot. Not only can volvulus cause an obstruction in the bowel lumen, but because the mesentery carries the blood supply to the intestine, a volvulus can cause bowel necrosis if the blood supply is affected.

What is Omphalocele?
The midgut herniates through the umbilicus during development. Sometimes it doesn’t make it all the way back in, causing an omphalocele. This is almost always caught during prenatal exams for those who have access to prenatal ultrasound. Because the abdominal cavity develops without some of the intestines inside, it’s too small to fit things in at birth, so often babies are sent home with their intestines outside their abdominal cavities to grow big enough for repair.

What is Meckel’s diverticulum?
The most common congenital gastrointestinal anomaly is Meckel’s diverticulum. It looks a lot like an appendix, but is located in the ileum, usually within 2 feet of the ileocecal junction. The diverticulum is a result of a normal structure (a connection between the yolk sac and midgut) that doesn’t disappear as it should. It can contain gastric and pancreatic epithelial cells, which, due to their presence in an organ without any protection, can cause the walls of the pouch to bleed.
The yolk sac is initially in wide communication with the midgut. It becomes compressed into the umbilical cord when the gastrula folds into the cylindrical embryo. The stalk of the yolk sac may persist as a diverticulum off the ileum (midgut) or a cord from ileum to umbilicus with varying degrees of the persistence of the yolk sac lumen. The cord may be fibrous all the way (no lumen), or it may contain a sinus, cyst, or fistula.

What is the main presenting symptom for meckel’s diverticulum?
What is the rule of 2’s for this condition?
Bleeding
See slide

What is appendicitis?
The appendix itself is covered with visceral peritoneum, but it generally doesn’t touch the parietal peritoneum. Thus, when the appendix first becomes inflamed, only visceral sensory signals are sent to the brain. Visceral sensory signals are vague and difficult for the brain to localize, so patients generally report a general pain that moves around the lower right quadrant, often near the umbilicus. However, as the appendix increases in size, it can tough and irritate the parietal peritoneum, at which point, somatic nerves take over and send much sharper and more distinct signals to the brain. It’s at this point that a patient can point to a specific point on their abdomen and say, “it hurts right here.”




The […] supplies blood to the hindgut.
Inferior mesenteric artery, or IMA
Where can you find the IMA in the abdomen?
Can usually find it between the transverse and sigmoid colons in the midline.
What are the branches of the IMA and what do they supply?
Left colic –> distal transverse and descending colons and splenic flexure
Sigmoid arteries –> sigmoid colon
Superior rectal artery –> rectum
True/false: the superior, middle and inferior rectal arteries all come off the IMA
False *Middle and inferior rectal arteries come from the common iliac artery, which is a different branch of the aorta*




The marginal artery connects the […] and […] arteries
Left and middle colic
What 3 anastamoses in the abdomen must we know?
1) The celiac trunk and SMA are connected via the superior and inferior pancreaticoduodenal arteries
2) The SMA and IMA are connected via the marginal artery and sometimes the Arc of Riolan. This anastomosis is so large that a person can live with an entirely obstructed IMA and survive because of increased blood flow through the SMA. A common site of abdominal aortic aneurysm is right where the IMA comes off the aorta, and in repairing it, surgeons won’t replace the IMA, but depend on increased flow through the SMA via the marginal artery to keep the hindgut structures alive.
3) Increased blood flow through the internal iliac artery can also compensate for a lost IMA, because the middle and inferior rectal arteries (branches of the internal iliac) anastomose with the superior rectal artery (branch of the IMA) and therefore can assist in supplying the foregut when necessary.
How is the hindgut innervated?

Parasympathetic innervation to the hindgut is carried in the pelvic splanchnic nerves, which come from branches of S2 through S4. Sympathetic innervation comes from the lumbar splanchnic nerves, which synapse at the inferior mesenteric ganglion. The inferior mesenteric plexus carries postsynaptic sympathetic and parasympathetic innervation to the hindgut







- Colonoscopies are recommended as a preventative screening every […] years after the age of […] (for people of average risk)
- What does a colonoscopy visualize?
10
50
The screening visualizes the colon and terminal ileum and allows for the removal of small polyps

- What is diverticulosis?
- Where is it most common?
- What is thought to be a possible causative factor?
- When does it become diverticulitis?
- Outpouchings of colon
- Descending and sigmoid colons
- Low-fiber diet
- If the pouches get infected causing inflammation and pain

What is Hirschprung’s Disease?
During development, the enteric nerves may not develop in some of the distal colon, causing it to collapse and block stool from passing through. Proximal to the area without nerves, stool builds up and causes a megacolon



