2.1.3 Immune-mediated Tissue Injury Flashcards
What are the important cytokines in type I hypersensitivity?
IL-1, 3, 4, 5, and 6
What are the important arachidonic acid metabolites produced in type I hypersensitivity?
Prostaglandins and leukotrienes B4, C4, and D4
What type of hypersensitivity are these images related to?

Type I hypersensitivity
What is this an image of?

Type I hypersensitivity - asthma
Small bronchiole with mucus plugging (goblet cell hyperplasia), smooth muscle hypertrophy, and a surrounding chronic inflammatory cell infiltrate. These are suggestive, but not diagnostic, of asthma, a diagnosis usually made by pulmonary function testing.
What is this an image of?
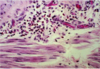
Asthma - High power of previous. Eosinophils and mononuclear cells. The chronic inflammatory cells are now known to cause irreversible, although mild, lung injury (interstitial fibrosis and remodeling) in asthma, so it is imperative that asthma be well-controlled to avoid chronic lung problems later in life.
What is the cause of autoimmune hemolytic anemia?
Antibodies against red blood cell membrane proteins leads to opsonization and phagocytosis or red cells
What is the cause of Goodpasture syndrome?
Noncollagenous protein in basement membranes of kidney glomeruli and lung alveoli leading to complement and Fc receptor mediated inflammation
What is this?

Linear basement membrane fluorescence in Goodpasture syndrome, caused by an IgG antibody against collagen type IV, which, you will recall, occurs only in basement membranes.
What is the cause of polyarteritis nodosa?
Hep B virus antigens resulting in systemic vasculitis - Type 3 hypersensitivity
Explain this image

Type III hypersensitivity - Antibodies form complexes on the endothelium of vessels. Activation of complement attracting neutrophils to release lysosomal enzymes.
What is this an image of?

Post-streptococcal glomerulonephritis. Note hypercellular glomerulus. Many of the extra nuclei are PMNs, attracted by chemokines, and attached to the membrane via C3b and Fc receptors.
Type 3 hypersensitivity
What is this an image of?

This is granulomatous inflammation at type IV reaction
What is this?

Non-caseating granuloma characteristic of a type IV
What is this an image of?

Caseating granuloma in pulmonary tuberculosis, widely considered to be a Type IV hypersensitivity disease, as the pathogen (Mycobacterium tuberculosis hominis) has no toxins, and usually very few organisms can be found, often located within epithelioid histiocytes or Langhans giant cells.
What is this?

A. Perivascular accumulation (“cuffing”) of mononuclear inflammatory cells (lymphocytes and macrophages), with associated dermal edema and fibrin deposition. B, Immunoperoxidase staining reveals a predominantly perivascular cellular infiltrate that marks positively with anti-CD4 antibodies.
Type IV hypersensitivity
What is this and what causes it?

This is another example of Type IV hypersensitivity. Macrophages in the skin (a.k.a. Langerhans cells or dendritic cells) present plant antigen to T cells, which do the damage to the basilar epithelium several hours or days after the initial encounter with the plant (That’s why they call it delayed-type hypersensitivity!).


