Uro - Renal Regulation Flashcards
What force drives osmosis in the kidneys?
osmotic pressure

What is osmotic pressure proportional to?
Osmotic pressure ∝ No. of solute particles
What is osmalarity?
Osmolarity = Concentration x No. of dissociated particles
(Osm/L OR mOsm/L)
Calculate the osmolarity for 100 mmol/L glucose
Osmolarity for glucose = 100 x 1 = 100 mOsm/L
Calculate the osmolarity for 100mmol/L NaCl.
Osmolarity for NaCl = 100 x 2 = 200 mOsm/L
What percentage of our body weight is made up of fluid volume?
60%
What is distribution of fluid in the body?

What is water loss is unregulated?
- Sweat
- Feces
- Vomit
- Water evaporation from respiratory lining and skin
What water loss is regulated?
• Renal regulation – urine production
What is the general process of positive water balance in renal regulation?
high water intake → increased ECF volume, decreased sodium ions, decreased osmolarity → hypo-osmotic urine production → osmolarity normlises
What is the process of negative water balance in renal regulation?
low water intake → decreased ECF volume, increased sodium ions, increased osmolarity → hyper-osmotic urine production → osmolarity normlises
What compartment does water enter first when entering the body?
ECF, then moves into intracellular fluid space
How much water is reabsorped in PCT?
67%
What is reabsorped in the thin descending loop, and how?
water (passively) but NO NaCl
What is reabsorped in the thin ascending loop of Henle, and how?
NaCl (passively), but no water
What is reabsorped in the thick ascending loop of Henle, and how?
NaCl (actively)
What is reabsorped in the collecting duct? Why?
- variable amounts of water
- modulates aquaporin channels, responds to hormones depending on body’s needs, etc.
Why does the thin descending loop not reabsorp NaCl?
- Since water is reabsorbed through the passive process of osmosis, it requires a gradient.
- The medullary interstitium needs to be hyperosmotic for water reabsorption to occur from the Loop of Henle and Collecting duct.
- done so that body doesn’t waste energy actively transporting water, etc.
What is the process of concurrent multiplication?
- when filtrate passes through the thin descending limb round to the thick ascending limb, active salt reabsorption occurs in the thick ascending limb.
- this decreases osmolality in the thick ascending limb and increases osmolality in the medullary interstitium.
- when the medullary interstitium’s osmolality increases, passive water reabsorption from the thin descending limb occurs in order to reach equilibrium.
- this process occurs multiple times, and forms a gradient through the loop of henle

How does urea leave the medullary interstitium?
2 ways:
- enters the vasa recta (series of blood capillaries that surrounds the nephron)
- enters the loop of Henle via the thin descending limb
What transporter does urea use to enter the vasa recta?
UT-B1
What transporter does urea use to enter the thin descending limb?
UT-A2
How is urea recycled?
- enters the loop of henle and collecting duct
- comes back to the medullary interstitium using UT-A1 and UT-A3
Why is urea recycled?
to increase the medullary interstitium’s osmolarity
What is the purpose of increasing the interstitium’s osmolarity?
- urine becomes more concentrated + urea excretion requires less water
- this is due to the interstitium’s high urea concentration, causing the ure conc. in the collecting duct to increase to reach an equilibrium.
- this high urea con. requires less water to be excreted
- allows body to conserve this water
What effects does vasopressin have on urea recycling?
vasopressin boosts UT-A1 and UT-A3 numbers in the colletcing duct, help sincrease collecting duct’s permeability for urea
What is vasopressin / ADH?
protein (length of 9 AAs)
What produces vasopressin?
hypothalamus (neurones in the supraoptic + paraventricular nuclei)
Where is vasopressin + ADH stored?
posterior pituitary
What is the main function of vasopressin?
- promote water reabsorption from the collecting duct
- plays a role in urea excretion + sodium excretion
What factors stimulate ADH production?
- increase in plasma osmolarity
- hypovolemia (state of abnormally low extracellular fluid in the body)
- decrease in blood pressure
- nausea
- angiotensin II
- nicotine
What factors inhibit ADH production + release?
- decrease in plasma osmolarity
- hypervolemia
- increase in blood pressure
- ethanol
- atrial natriuretic peptide
What detects fluctuation in plasma osmolarity?
osmoreceptors in hypothalamus
What detects change in blood pressure + volume? What percentage of change is required for it to be detected?
baroreceptors, 5-10%, info transmitted to hypothalamus
How does ADH allow water to be reabsorped? What transporters + proteins are involved?
- ADH comes and binds to the V2 receptors
- this activates the G-protein mediated signalling cascade
- this activates protein kinase A
- this increases the secretion of aquaporin 2 channels
- this channels are transported to the apical membrane + inserted
- allows water to be reabsorped from the lumen of the collecting duct
- aquaporin 3 and 4 transport this reabsorped water back into blood capillaries

How does ADH affect aquaporin trasporters?
upregulates + downregulates aquaporin transporters as needed?
What is diuresis?
increased dilute urine excretion
How much ADH is involved in diuresis?
usually little to none
How does diuresis occur?
fluid flowing from the PCT to the loop of Henle is isomotic fluid
when travelling through the loop of henle, due to greater net reabsorption of NaCl, fluid becomes hypo-osmotic
due to lack of ADH, there are no aquaporin channels in the DCT, so water is not reabsorped
some water is reabsorped through some pre-existing aquaporin channels + paracellular pathways in the collecting duct
end result = lots of urine with osmolarity of (50 mOsm/L)

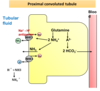
How does NaCl reabsorption occur in the thick ascending limb?
- sodium potassium ATPase pump pumps sodium ions out of the cell and potassium ions into the cell through the basolateral mebrane
- creates a low sodium concentration inside the cell
- causes sodium ions to enter cell through apical membrane passively through sodium potassium chloride symporter
- this releases energy, which is used by chloride + potassium ions to enter the cell via the same transporter
- potassium and chloride ions exit the cell via the potassium + chloride symporter via the basolateral membrane
- potassium ions are also recycled and reabsorped from the cells through the apical membrane
- chloride ions also exit the cell via the basolateral membrane

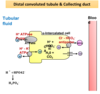
How is NaCl reabsorped from the DCT?
- sodium potassium ATPase pump pumps sodium ions out of the cell and potassium ions into the cell through the basolateral mebrane
- creates a low sodium concentration inside the cell
- causes sodium ions to enter cell through apical membrane passively through sodium potassium chloride symporter
- this releases energy, which is used by chloride + potassium ions to enter the cell via the same transporter
- potassium and chloride ions exit the cell via the potassium + chloride symporter via the basolateral membrane
- chloride ions also exit the cell via the basolateral membrane passively
How are sodium ions reabsorped in the collecting duct?
- via the principal cells, which have a sodium potassium ATPase pump
- creates a low conc of sodium ions inside cell
- creates a concentration gradient
- allows sodium to passively enter cell through apical side

What is antidiuresis?
concentrated urine in low volume excretion
What is the ADH amount like in antidiuresis?
high
How does ADH support Na+ reabsorption?
- Thick ascending limb: upregulates Na+ - K+ - 2Cl- symporter
- Distal convoluted tubule: upregulates Na+ - Cl- symporter
- Collecting duct: upregulates Na+ channel
How does antidiuresis occur?
- when hyposomotic fluid reached the DCT, due to ADH there is a huge upregulation of aquaporin channels, allowing water to be reabsorped
- as it passes through the colletcing ducts, countercurrent multiplication continues to occur, so by the time fluid leaves the kidneys, it has an osmolarity close to 1200 mOsm/L

Name 3 ADH related clinical disorders.
- central diabetes insipidus
- syndrome of inappropriate ADH secretion (SIADH)
- nephrogenic diabetes insipidus
What is the cause of central diabetes insipidus?
decreased / negligent production + release of ADH
What are the clinical features of central diabetes insipidus?
- polyuria
- polydipsia
How is central diabetes insipidus treated?
external ADH
What is the cause of SIADH?
increased poduction + release of ADH
What are the clinical features of SIADH?
- hyperosmolar urine
- hypervolemia
- hypoatremia
What is the treatment for SIADH?
non-peptide inhibitor of ADH receptor
e.g. conivaptan or tolvaptan
What is the cause of nephrogenic diabetes insipidus?
less/mutant AQP2 or mutant V2 receptor
What are the clinical features of nephrogenic DI?
- polyuria
- polydipsia
What is the treatment for nephrogenic DI?
thiazide diuretics, NSAIDs
What causes an increase in our acid + base conc. in our blood?
diet + metabolism
What is our net gain of acid or base? Why?
Why does the net addition of metabolic acid need to be neutralised?
to prevent blood pH from chnaging and preventing the body from going into acidosis
How is metabolic acid neutralised?
neutralised through bicarbonate buffers:
- H2SO4 + 2NaHCO3 ↔ Na2SO4 + 2CO2 + 2H2O
- HCl+NaHCO3↔NaCl+CO2+H2O
What is our average store of bicarbonate? Why does it need to be replenished?
ECF [HCO3-] = approx. 350 mEq
needs to be replenished or regenerated as stores will run out after 4-7 days
What role do the kideys play in replenishing our bicarbonate stores?
- secretion + excretion of H+ ions (prevents body form goign inot acidosis)
- reabsorption of HCO3- ions
- production of new HCO3- ions (allows for replenishing + regenration of bicarbonate stores)
How does CO2 contribute to both H+ and HCO3-?
CO2+H2O is turned into H2CO3 using enzyme CARBONIC ANYHYDRASE
H2CO3 diassociates into H+ and HCO3- ions
What is the Henderson-Hasselbalch equation?
- pH=pK′+ log (HCO3-)/αPCO2
- [H+]= (24 x PCO2)/([HCO3-])
What is the classification of an acid-base disorder if the cause is CO2 pressure?
respiratory
What is the classification of an acid-base disorder if the cause is [HC03] ions?
metabolic
What is the distribution of bicarbonate ions reabsorption?

How are bicarbonate ions reabsorped in the PCT?
- CO2 + H2O from the tubular fluid is converted into H+ ions and HCO3- ions by CA in the PCT
- H+ ions exit the PCT via 2 ways:
- sodium and hydrogen ion antiporter, pulls sodium ions into cell and pushes hydrogen ions into tubular fluid
- H+ ATPase pump, pumps H+ ions into tubular fluid
- HCO3- ions are transported into the blood via soidum + bicarbonate ion symporter

How does bicarboante ion reabsorption work in the DCT and colletcing duct?
- uses alpha-intercalated cells
- H+ ions are excreted in 2 ways:
- H+ ATPase pump
- H+ K+ ATPase pump
- HCO3- ions are reabsorped using Cl- HCO3- antiporter

What is the purpose of beta-intercalated cells in the DCT + collecting duct?
- used when body is in alkalosis
- responsible for HCO3- secretion + H+ reabsorption

How are new bicarbonate ions produced in the PCT?
- glutamine becomes ammonia ions and A2- ion
- A2- ions further separates to become 2 bicarbonate ions, which are reabsorped into blood

Why does ammonia produced from glutamate breakdown when forming HCO3- need to be excreted? How is it excreted?
- ammonia ions entering the blood ciruclation would need to be metabolised in liver, which requires bicarbonate ions
- this would negate any bicarbonate ion production in this process
- therefore ammonia is excreted in 2 ways:
- sodium hydrogen antiporter that excretes ammonia instead of hyrdogen ions
- excreted as ammonia gas, combing with hydrogen ions in the tubular fluid to be excreted as ammonia ions
How are new bicarbonate ions formed in the DCT + collecting tube?
bicarbonate buffers in the tubular fluid e.g. HPO4- neautralise the hydroegn ions released from the breakdown of CO2, resulting in a net gain of bicarbonate ions
What are the characteristics of metabolic acidosis?
low bicarbonate ion conc, low pH
What is the compensatory repsonse for metabolic acidosis?
increased ventilation, increased bicarbonate ion reabsorption + production
What are the characteristics of respiratory acidosis?
increased CO2 pressure, decreased pH
What is the compensatory response for respiratory acidosis, acute + chronic?
- acute = intracellular buffering
- chronic = increased bicarbonate ions reabsorption + production
What are the characteristics of resp alkalosis?
decreased CO2 pressure, increased pH
What is the compensatory repsonse for resp alkalosis?
acute = intracellular buffering
chronic = decreased bicarbonate ions reabsorption + production


