Syke's infectious diseases - bacterial Flashcards
What specie(s) of tick(s) transmit Ehrlichia canis?
Rhipicephalus sanguineus (primary); Ixodes ricinus, Haemaphysalis spp. ticks, and Dermacentor spp. ticks; experimental transmission has been accom- plished with Dermacentor variabilis ticks
What specie(s) of tick(s) transmit Ehrlichia ewingii?
Amblyomma americanum
What infectious organism(s) does Rhipicephalus sanguineus transmit?
Ehrlichia canis, Babesia canis, Rickettsia ricketsii
What infectious organism(s) does Amblyomma americanum transmit?
Ehrlichia ewingii, Ehrlichia chafeensis, Francisella tularensis, Rickettsia ricketsii
What cells does Ehrlichia infect?
leukocytes – Ehrlichia canis (monocytes), Ehrlichia ewingii (granulocytes), Ehrlichia chafeensis (monocytes)
What are the phases of canine monocytic ehrlichiosis (CME)?
acute (8-20 days after infection); subclinical (months to years); chronic
Where does Ehrlichia canis multiply/replicate?
multiplies by binary fission within vacuoles of mononucear phagocytes –> rupture of infected host cells leads to infection of new cells
Why might a dog infected with Ehrlichia have a negative immunofluorescent antibody (IFA) test?
antibodies can only be detected 7-28 days after initial infection – false-negative may occur if tested too soon
T/F: A positive serum antibody titer for Ehrlichia indicates infection.
False - may reflect previous exposure and not necessarily disease
What test is more sensitive than immunofluorescent antibody or ELISA testing for acute canine monocytic ehrlichiosis?
whole-blood PCR assys for E. canis DNA
Why are fluoroquinolones not recommended for treatment of canine monocytic ehrlichiosis?
Ehrlichia canis appears to have intrinsic gyrase-mediated resistance to fluoroquinolones
What cutaneous signs have been associated with canine monocytic ehrlichiosis?
petechial and ecchymotic hemorrhages (occur d/t thrombocytopenia and platelet dysfunction)
What ticks are known to transmit Rickettsia ricketsii?
Dermacentor variabilis (american dog tick), Dermacentor andersoni (Rocky mountain wood tick), Rhipicephalus sanguineus, Amblyomma americanum, Amblyomma cajennense, Amblyomma aureolatum
What organism causes Rocky Mountain spotted fever? Characteristics of the organism?
Rickettsia rickettsii, an obligately intracellular bacteria
What is the characteristic clinical sign of Rocky Mountain spotted fever?
disseminated vasculitis –> cutaneous macules, papules, petecchia
What cells does Rickettsia ricketsii infect?
primarily infects endothelial cells (smooth muscles and monocytes may also be infected)
T/F: Rocky Mountain spotted fever has three phases: acute, subclinical, and chronic.
False - Ehrlichia has three phases, RMSF causes an ACUTE disease
What tests are used to aid in diagnosis of Rocky Mountain spotted fever?
convalescent antibody titers (2-3 weeks apart), PCR testing (during acute phase), biopsy – shows vasculitis and organisms around vessels – with direct IFA or Gimenez stain
What antibiotics can worsen the course of Rocky Mountain spotted fever?
trimethoprim sulfonamides
T/F: Staphylococcus spp. are strictly aerobic bacteria.
False - facultative anaerobes
What is coagulase?
enzyme that cleaves fibrinogen into fibrin –> results in coagulation of plasma
What is the mecA gene?
located on a large genetic element (staphylococcal casette chromosome) –> encodes an altered penicillin binding protein (PBP2a)
what are the members of the S. intermedius group?
Staph. Intermedius, Staph. Pseudintermedius, Staph. Delphini
Scalded skin syndrome has been reported in people with what organism? Pathogenesis?
Staph. Aureus –> strains that produce an exfoliative toxin, which hydrolyzes the intercellular glycoprotein desmoglein-1
How does inducible clindamycin resistance occur?
bacterial methylation of the ribosomal binding site for clindamycin
How can you test for inducible clindamycin resistance?
D-zone test – culture organism in the presence of erythromycin and clindamycin disks; organisms near the erythromycin disk express enhanced resistance to clindamycin –> results in a D shape to the zone of inhibition around the clindamycin disk
Staph strains that possess the tetracycline efflux protein tetK may still be susceptible to what tetracycline antibiotic?
minocycyline
Staph strains that posses tetM are resistant to which tetracyclines?
All tetracyclines (including minocycline) – tetM protects the ribosome from tetracycline binding
What layer of the cell membrane is much thicker in gram-positive bacteria than gram-negative bacteria?
peptidoglycan layer
What additional cell membrane structures are present in gram-negative bacteria?
complex outer membrane that contains lipopolysaccharide as well as porins (regulate transport of molecules in and out of the cell)
What are the components of lipopolysaccharide?
lipid A backbone, core oligosaccharide, O antigen side chain
What component of the cell membrane of gram negative bacteria is called endotoxin?
lipid A component - phosphorylated disaccharide to which long, hydrophobic fatty acid chains are attached (anchors LPS into the outer membrane); Is the biologically active portion of the molecule –> stimulates a potent host inflammatory response
Examples of gram-negative cocci? Where are they found on the body?
Moraxella, Neisseria – commensals of the oral cavity of dogs and cats
Two categories of gram-negative rods?
Enterobacteriaceae (E. coli, Proteus, Salmonella, Enterobacter, Citrobacter, Serratia, Klebsiella) and non-Enterobacteriaceae (Pasteurellaceae, Pseudomonas aeruginosa, Acinetobacter)
Virulence factors of Enterobacteriaceae?
capsule (K antigen), flagella (H antigen)
Virulence factors of Pseudomonas aeruginosa?
exotoxins, type III secretion system, LPS, pili, flagella, proteases, phospholipases, iron-scavenging mechanisms such as pyoverdin production, biofilms (almost every type of virulence factor!!!)
Mechanisms of resistance of Pseudomonas aeruginosa?
production of beta-lactamase enzymes (can include ESBLs), antibiotic efflux pumps, enzymes that modify aminoglycosides or later antibiotic binding sites (such as DNA gyrase for fluoroquinolones), and decreased bacterial permeability
Characteristics of actinomyces? Normal site of inhabitance?
anaerobic or microaerophilic, filamentous, gram-positive bacteria; tan to yellow colonies; normal inhabitants of mucous membranes
Typical route of infection with actinomyces?
inoculation into tissues with other bacteria, often as a result of deeply penetrating wound or foreign body migration
Differential diagnoses for actinomycosis?
mycobacterial infections, streptomycosis, nocardiosis, bartonellosis, fungal infections, neoplasia
Clinical signs associated with actinomycosis?
subcutaneous masses and draining skin lesions (cervicofacial and cutaneous-subcutaneous disease); pulmonary nodules/masses/effusion; abdominal effusion/masses
Appearance of Actinomyces on cytology?
filamentous rods; gram-postive, non-acid fast filamentous organisms that are occasionally branched – filaments are less than 1 um wide, vary in legnth, and can stain irregularly –> produces a “beaded” appearance
Gross characteristics of Actinomycosis
sulfur granules may be visible – white to tan gray granules
T/F: Actinomyces spp. are difficult to grow on routine aerobic cultures.
False - most that cause disease are facultative anaerobes that will grow under aerobic conditions BUT a few are obligate anaerobes (A. bovis, A. israelii, A. meyeri); visible growth can occur within 48 hours but usually requires 5-7 days
T/F: It is common to isolate up to five other associated bacteria along with Actinomyces spp.
True - most are also resident flora of the oral cavity or intestinal tract
Histopathologic findings with Actinomycosis?
abscesses with a core of neutrophils encapsulated by granulation tissue; sulfur granules are generally in the center of microabscesses – granules are round, oval or scalloped amphophilic solid masses; often rimmed by partially confluent radiating eosinophilic club-shaped structures (Splendore-Hoeppli phenomenon)
The Splendore-Hoeppli phenomenon has been reported with what infections?
Actinomycosis, Zygomycosis, sporotrichosis, parasitic infections, foreign body reactions, hypereosinophilic syndrome
T/F: Acintomyces stain positive with acid fast.
False - they are NOT acid fast; will stain with Gram stain (gram positive), Giemsa, and silver stains
What is the drug of choice for actinomycosis?
penicillins
Characteristics of nocardia (gram +/-? Rods/cocci?)? Normal sites of inhabitance?
filamentous, branching (branch at right angles), gram positive bacteria; ubiquitous soil saprophytes, found in water, dust, and on decaying plants and fecal matter
What is the most common form of nocardiosis in cats?
cutaneous-subcutaneous nocardiosis - slow and progressive circumferential spread of a nonhealing, draining wound
What is the most common form of nocardiosis in people?
pulmonary nocardiosis (does occur in dogs and less commonly in cats) - resembles deep mycoses
T/F: Nocardia stain positive with acid-fast stain.
True - often partially or weakly acid-fast
T/F: Mycobacterium spp., like Nocardia, will often branch.
False - only Nocardia branches
T/F: Nocardiosis is often associated with mixed infections.
False - Actinomycosis is associated with mixed infections, Nocardiosis is usually the only pathogen
T/F: Nocardia grow aerobically under normal conditions.
True - colonies are usually visible within 2 days but sometimes can take 2-4 weeks of incubation
Histopathologic findings with Nocardiosis?
central region of necrosis and suppuration, surrounded by macrophages, lymphocytes, and plasma cells; Nocardia filaments are usually present in abundance within regions of necrosis and suppuration
T/F: Nocardia spp. are readily identified on biopsy specimens with H&E.
False - need Gram stain or methenamine silver, partially acid fast
What are the first line antimicrobials for treatment of Nocardiosis?
sulfonamides, including trimethoprim-sulfonamides
T/F: Wide surgical exicision is necessary for cure of both Actinomycosis and Nocardiosis.
False - not usually needed for Actinomycosis unless present for long periods of time with granulation tissue/fibrosis; usually needed for Nocardiosis
Characteristics of mycobacterium spp. (gram +/-? Rods/cocci?)?
aerobic, nonmotile, non-spore-forming, GRAM POSITIVE, ACID-FAST pleomorphic bacilli
What stains are useful to find Mycobacterium?
Ziehl-Neelson or Kinyoun stains (acid-fast stains)
What species is the reservoir host for Mycobacterium tuberculosis?
humans, cats are RESISTANT to infection with M. tuberculosis
What species is the reservoir host for Mycobacterium microti?
rodents (especially voles & shrews)
What species is the reservoir host for Mycobacterium bovis?
cattle and other wildlife species
What bacteria from the Mycobacterium tubeculosis complex infect dogs and cats?
Mycobacteria tuberculosis - dogs ONLY; Mycobacteria bovis & Mycobacteria microti - cats & rarely dogs
What species of Mycobacterium are SLOWLY growing?
Mycobacterium tuberculosis complex (M. tuberculosis, M. bovis, M. microti); M. avium-intracellulare complex (M. avium subsp. Avium, M. avium subsp hominissuis); Slowly growing nontuberculosis mycobacteria (M. kansaii, M. ulcerans, M. genavense, M. malmoense, M. celatum, M. terrae, M. simiae, M. visibile)
What species of Mycobacterium are RAPIDLY growing?
M. fortuitum, M. smegmatis, M. abscessus, M. chelonae, M. thermoresistibile, M. goodii, M. flavescens, M. alvei
What species of Mycobacterium are unable to be cultured?
Mycobacterium lepraemurium, the Canine Leproid Granuloma organism
Mycobacterium tuberculosis complex organisms can replicate inside of what cells inside of the host?
can replicate locally at site of inoculation (lungs, skin, GI tract) but are then ingested by macrophages and replicate within the cells –> macrophage destruction leads to recruitment of lymphocytes and additional monocytes –> tubercle formation
Cats infected with M. bovis or M. microti have what clinical signs?
cutaneous nodular lesions +/- mandibular lymphadenopathy
What findings on cytology are suggstive of mycobacterial tuberculosis complex infection?
mixed population of heavily vacuolated histiocytes, smaller numbers of neutrophils and small lymphocytes; intracytoplasmic, nonstaining bacilli inside of macrophages***; cholesterol crystals, caseous debris, concentrically laminated crystalline structures (calcospherite bodies)
T/F: Routine aerobic, anaerobic, fungal, and mycoplasma cultures are negative from animals with mycobacterium tuberculosis complex infections.
True - require special medium to grow (7H11 agar or Lowenstein-Jensen media)
Histopathologic findings with mycobacterium tuberculosis complex infections?
tubercles/granulomas composed of abundant epithelioid macrophages and lesser number of neutrophils; acid-fast stains reveal low numbers of acid-fast bacteria in the tubercle centers
T/F: Both mycobacterium tuberculosis complex and mycobacterium avium complex bacteria have reservoir hosts.
False - only mycobacterium tuberculosis complex organisms have reservoir hosts – MAC bacteria are environmental saprophytes
T/F: Pulmonary lesions are not common with Mycobacterium avium complex infections in dogs.
True - different from mycobacterium tuberculosis complex infections
Infection with mycobacterium avium complex bacteria usually occurs under what conditions?
immunosuppression/immunocompromised animals
Feline leprosy is caused by what organism?
Mycobacterium lepraemurium
T/F: The causative organism of canine leproid granuloma syndrome has never been isolated in culture.
True - has only be partially characterized by PCR sequencing
T/F: Cats with feline leprosy are usually systemically ill.
False - usually only have cutaneous/subcutaneous nodules
What is the environmental reservoir of non-tuberculosis bacteria other than mycobacterium-avium
soil and water sources
What type of mycobacterial infection has a predilection for infecting adipose tissue
rapidly growing mycobacteria - M. fortuitum and M. smegmatis –> develop mycobacterial panniculitis
T/F: Infection with rapidly growing mycobacteria such as Mycobacterium fortuitum or Mycobacterium smegmatis is usually secondary to immunosuppression.
False - usually are inoculated by means of cat fight injuries (bites/scratches) or other penetrating wounds
T/F: Disseminated infections with rapidly growing mycobacteria such as M. fortuitum or M. smegmatis are rare.
TRUE
T/F: Disease caused by the non-tuberculoid slowly growing mycobacteria resemble disease caused by mycobacterium avium complex.
True - can cause ulcerative skin lesions or disseminated disease
In cats, mycobacterial panniculitis is most likely to occur where on the body?
inguinal fat pad – subcutis becomes thickened and adheres to the dermis —> nodular and draining skin lesions develop
T/F: Cats with mycobacterial panniculitis are usually systemically ill.
False - usually are otherwise well
Histopathologic findings with mycobacterial panniculitis?
pyogranulomatous inflammation without tubercle formation or necrosis; large lipid vacuoles that contain acid-fast bacilli may be present
T/F: Rapidly growing mycobacteria (M. fortuitum and M. smegmatis) grow readily on routine culture media.
TRUE
What treatment options are recommended for mycobacterium avium complex or slowly growing mycobacterial infections?
combinations of clarithromycin, rifamycin, and a fluoroquinolone
What are treatment options for rapidly growing mycobacterial infections?
doxycycline, fluoroquinolones, clarithromycin, aminoglycosides, sulfonamides, carbapenems
Differential diagnoses for mycobacterial infection in the cat?
neoplasia (lymphoma), feline infectious peritonitis, tularemia, nocardiosis, actinomycosis, rhodococcosis, bartonellosis, leishmaniasis, fungal infections (crypto, blasto, etc.)
Most common species of Bartonella in cats?
Bartonella henselae, Bartonella clarridgeiae
Most common species of Bartonella in dogs?
Bartonella vinsonii subsp berkhoffii, Bartonella henselae
Mode of transmission of Bartonella?
fleas (Ctenocephalides felis), other species of fleas (Pulex spp.) and vectors such as ticks, lice, biting flies
Most frequent manifestation of bartonellosis in dogs
endocarditis – clinical signs include lethargy, fever, cardiac murmur, cough, tachypnea, lameness, neurologic signs
Characteristics of bartonella spp?
Fastidious, intraerythrocytic GRAM-NEGATIVE bacteria
What species is the reservoir host for Bartonella henselae?
cats
What species is the reservoir host for Bartonella vinsonii subsp berkhoffi?
domestic and wild dogs
After infection, where does Bartonella replicate?
in erythrocytes; can also infect endothelial cells and bone marrow progenitor cells
T/F: Most dogs and cats infected with Bartonella show no clinical signs of illness when bacteremic.
TRUE- cats infected with B. henselae develop a small papule at the site of inoculation, transient fever and lymphadenopathy (may show no clinical signs)
Histopathologic findings with Bartonella infections? In what tissue?
Chronic inflammation with fibrous tissue and extensive mineral deposits in the HEART; small bacilli may be seen within lesions with silver stains or IHC for B. henselae)
Why might a blood culture be negative in an animal infected with Bartonella?
due to relapsing bacteremia (and may have a low level of bacteremia)
Antibiotics recommended for treatment of Bartonellosis?
doxycycline; amoxicillin-clavulanic acid
DDX?

Actinomyces, Nocardia spp., Corynebacterium spp., Mycobacterium spp.
Describe changes present and give top ddx
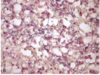
Severe, necrotizing pyogranulomatous inflammation with intralesional, filamentous, branching, gram-positive bacteria;
Top DDX is Nocardiosis (less likely Actinomycosis)


