Regulation of blood glucose by the endocrine system week 4 Flashcards
In the body, the availability of ATP is kept as constant as possible by regulating the concentration of ____ (the predominant source or substrate for the production of ATP) in the blood.
In the body, the availability of ATP is kept as constant as possible by regulating the concentration of glucose (the predominant source or substrate for the production of ATP) in the blood.
a. Too low a blood glucose concentration (hypoglycemia) leads to cellular dysfunction (particularly in the CNS).
b. Too high a blood glucose concentration (hyperglycemia) damages many cells and tissues throughout the body.
What are the ranges for fasting and post-prandial blood glucose levels?
Fasting: 70 – 100 mg/dl
Post-prandial: up to 140 mg/dl
What hormones are responsible for decreasing blood glucose?
What hormones are responsible for increasing blood glucose?
- Hormones that decrease the blood glucose levels –> Insulin
- Hormones that increase the blood glucose
levels –> Glucagon, Epinephrine, Cortisol,
Thyroid Hormones, Growth Hormone
What organ is exposed to the highest concentration of pancreatic hormones and extracts 50% of the insulin released by the pancreas?

What is insulin co-secreted with? What is the fxn of this substance?
Why is it more reliable to measure this substance instead of measuring insulin concentrations if you want an idea of insulin concentration?
Since insulin is quickly cleared from the bloodstream (50% after perfusion of the liver), C-peptide concentrations are used to determine levels of insulin secretion. C-peptide is not absorbed by the liver.
C peptide is now believed to be a growth hormone.

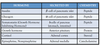
Explain what the error detector, control center, effectors, and variable is for regulation of glucose concentration.

What GLUT transporter is present in the pancreas? When does this transporter bring glucose into the cell?
In B-cells of the pancreas, glucose undergoes degradation which increases the cellular level of what 3 molecules?
• Insulin controls the rate of glucose uptake in many tissues
-• exceptions are the brain and the liver
• B- cells themselves take up glucose in an insulin independent manner (GLUT-2)
• the rate of glucose uptake depends on the plasma glucose level
• In the B-cells, glucose undergoes degradation, which increases the cellular level of:
-• ATP, nicotinamide adenine dinucleotide phosphate (NADP), and NADPH
Explain the cellular mechanism of how glucose stimulates insulin release from B-cells of the pancreas.
- glucose uptake through GLUT2
- glucokinase (Km=5mM)-at equilibrium with resting blood glucose concentration.
- glucose metabolism-glucose–>pyruvate–ACoA–>TCA cycle–>electron transport chain–>ATP
- Increase in ATP/ADP ratio
- ATP closes the ATP dependent K+ channel.
- Closing of the K+ channel causes membrane depolarization
- Depolarization opens Ca2+ channels and increases intracellular Ca2+ concentration
- Insulin granules fuse with the membrane and are released-Ca2+ dependent process

Explain the role of the ATP dependent K+ channel in DM.
How are sulfonureas used in the treatment of DM?
Sulfonylureas:
- Close K+ channel in β-cells
- cell depolarization
- triggers insulin release
Clinical use
- endogenous insulin release
- requires islet function (type 2 diabetes)
Toxicities
-hypoglycemia

What is the incretin effect?
What 2 hormones are responsible for the incretin effect?
What is repsonsible for the inactivation of these 2 hormones?

Explain the difference in the incretin effect between healthy patients and Type 2 diabetics.
What drugs may be given to normalize the incretin effect in Type 2 diabetics?
Other than stimulating insulin release

Explain the cellular mechanism behind the stimulation of insulin release by:
GLP-1
GIP
ACh

GIP, GLP-1
Gs-protein coupled receptor
• cAMP stimulation of PKA
• PKA dependent Ca channel phosphorylation
• enhanced [Ca]i
Acetylcholine (parasympathetic innervation, α-cells (paracrine)
Gs-protein coupled receptor
• DAG stimulates PKC
• PKC phosphorylates Ca-channel and K ATP channel
• Gs-protein stimulation of PLC–> IP3
• increasing [Ca]i through release from stores

What effect do amino acids have on insulin release? (explain cellular mechanism)
What effect do arginine and glycine/Na cotransport have on insulin release?
Amino Acids
-uptake into the cell
• metabolized to pyruvate
• increase of metabolic products ATP/ NADPH
• Arginine and glycine/Na co-transport leads to cell depolarization-Ca2+ flows into the cell and allows for insulin release

What effect does somatostatin have on insulin and glucagon release?
What effect do alpha-adrenergic agonists have on insulin release? Explain the cellular mechansim.

Explain the autocrine fxn of insulin.

Explain the phasic release of insulin.

The loss of which phase of insulin release is an early predictor of DM/glucose intolerance?

Insulin is a(n):
a. anabolic hormone
b. catabolic hormone
What organs are effected by insulin stimulation?
Insulin Action on Liver and Muscle:
Insulin:
• stimulates membrane insertion of glucose transporter
• transport of Glucose is passive down the Glucose gradient
• stimulates synthesis of glycogen (maintenance of glucose gradient)
• facilitates conversion of glucose to glycogen for storage (glycogen synthase)
• decreases breakdown of glycogen and release of glucose (glycogen phosphorylase)
• decreases gluconeogenesis by – pyruvate carboxylases – PEP carboxykinases – Fructose 1,6 bisphosphatases – glucose6-phosphatase inhibition.
Insulin Action on Adipose Tissue
STIMULATION
- of lipoprotein lipase that liberates free fatty acids (FFA) from tri-glycerides
- of FFA uptake into adipose cells
- of lipogenesis (acetyl-CoA carboxylase)
- of hepatic VLDL synthesis resulting in decreased ketone bodies in the bloodstream
INHIBITION
- of lipolysis (Hormone-sensitive adipose tissue lipase)
Other effects
– increases cellular uptake of K+
– increases Na+-retention in the kidney

What are the effects of insulin deficiency?

summary of insulin’s effects on metabolism

What stimulates glucagon release? What inhibits glucagon release?
Suppressed:
- by hyperglycemia
- by insulin
- free fatty acids & ketoacids
Stimulated:
- low blood glucose (hypoglycemia)
- high level amino acids (arginine, alanine)
- sympathetic stimulation, catecholamines
- GIP, Gastrin
- Glucocorticoids

How is glucagon released when blood glucose levels are low? (cellular mechansim)?
How is glucagon release inhibited when glucose levels are high?
• KATP channel
– α-cells have increased basal ATP levels
– K ATP dependent channel is closed in absence of glucose-membrane depol-glucagon release
• Insulin (Zn2+) and Somatostatin
– release stimulated by high glucose
– override depolarizing effects of the closed K ATP channel
– inhibits AMP-activated protein kinase (AMPK)
see figure on slide 39 of notes
Glucagon in response to a meal: How is glucagon release inhibited after a high carb meal?

Explain the changes in blood glucose levels after a high protein meal.

What effect do free FA have on glucagon release?

summary of glucagon effects
see reverse


Describe glucagon levels in individuals with type 2 diabetes.

see reverse


What organ is amylin secreted from? What hormone is it co-secreted with?
What are the effects of amylin?
• Amylin or Islet Amyloid Polypeptide (IAPP)
– co-secreted with Insulin (100:1)
– synergistic action to Insulin by inhibiting glucagon release
– promotes satiety
– decreases food intake
– slows down gastric emptying
– inhibits secretion of digestive fluids

How can amylin be used clinically? (what disease)

Where in the body is leptin produced?
What is the target organ of leptin?
What are the fxns of leptin?
What hormone opposes leptin? What organ is it released from?
• Leptin
– produced primarily in adipose tissue
– its secretion is proportional to the BMI
– it permeates the blood brain barrier
– at high levels it inhibits food intake and stimulates energy expenditure
– at low levels it stimulates food intake and decreases energy expenditure
– crosses blood brain barrier
– stimulates neurons in Arcuate Nucleus (ARC)
– ARC neurons project to the hypothalamus
– inhibits Agouti-related protein and Neuropeptide Y neurons, that stimulate food intake
– stimulates pro-opio-melanocortin, amphetamine related transcript neurons that inhibit food intake
-Ghrelin acts opposite to leptin and insulin (released from the stomach)

Explain the levels and effects of leptin in obesity.
• Obesity
– high blood levels of leptin
– decreased permeability of the blood brain barrier for Leptin
– Leptin permeability decreased with high fat diet

Explain the involvement of leptin in Prader-Willi syndrome.



