Mesenteric arteries, portal system, and biliary tree week 3 Flashcards
(18 cards)
What is the jejunoileum suspended from the posterior body wall by?
mesentery proper
How can the jejunum and ileum be distinguished by arterial anatomy?
Jejunum: short arterial arcades and long vasa recta (can remember as VV: jejunum has long villi and long vasa recta)
Ileum: long arterial arcades and short vasa recta

What is the mesentery of the appendix called?
mesoappendix
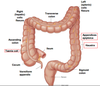
What are the 3 unique features of the colon?
- Haustra (sacculation)
- Taenia coli (longitudinal bands of smooth muscle; analogous to outer longitudinal smooth muscle of the small intestine)
- Appendices epiploica (fatty appendages.)
At what spinal level is the celiac trunk, SMA, and IMA?

What structures do the celiac trunk, superior mesenteric aa, and inferior mesenteric aa supply?
_____ of these arteries play a major role in keeping the blood flowing to all abdominal viscera.
Celiac trunk: foregut
SMA: midgut
IMA: hindgut
Anastomoses play a major role in keeping the blood flowing to all abdominal viscera.

Where does the SMA lie in relationship to the celiac trunk?
Where does the SMA lie in relationship to parts of the pancreas and duodenum?
What structure does the SMA enter?
Where does the SMV lie in relationship to the SMA?

- The SMA arises from the aorta deep to the neck of the pancreas and below the origin of the celiac artery at the L1 vertebral level.
- The SMA descends anterior to the uncinate process of the pancreas and the 3rd part of the duodenum to enter the mesentery of the small intestine.
- The superior mesenteric vein lies to the right of the artery.

What are the branches of the SMA? What do they supply?
What is special about the arterial supply to the pancreas?
Branches of the SMA include:
- Inferior pancreaticoduodenal arteries which anastomose with the superior pancreaticoduodenal branches of the gastroduodenal artery in the head of the pancreas. Note that the pancreas is an endocrine organ so it receives a lot of blood supply through the anastamosis of these arteries.
- Intestinal branches (12–15) from the left side of the SMA to supply the jejunum and ileum.
- Ileocolic artery is the most inferior branch which descends to the lower right quadrant to supply the distal ileum and cecum.
- Right colic artery passes to the right to supply the ascending colon.
- Middle colic artery ascends and enters the transverse mesocolon to supply the proximal two-thirds of the transverse colon.

What are the branches of the IMA? What do they supply?

Inferior Mesenteric Artery (IMA) supplies the distal 3rd of the transverse colon to the pectinate line).
Branches of the IMA include:
• Left colic artery - supplies the distal third of the transverse colon and the descending colon
• Sigmoid arteries - to the sigmoid colon
• Superior rectal artery - supplies the superior aspect of the rectum and anal canal.

Collateral circulation btwn the SMA an d IMA is critical to the flow to the small and large intestines. What artery is this collateral circulation due to?
Collateral Circulation between the SMA and IMA is critical to normal blood flow to the small and large intestines. The collateral circulation is due to the Marginal artery of Drummond, a continual arterial arch.
Dissector: the right and middle colic arteris form the marginal aa close to the wall of the ascending and transverse colon.

What is the most common site of bowel ischemia?
What vein may be compressed due to an aneurysm of the SMA? What sx may pts with this have? Specifically, what may males develop?
- The splenic flexure is the most common site of bowel ischemia. This is the most vulnerable spot of the marginal aa-connection btwn midgut and hindgut structures. As bowel develops, there can be weakness and incongruencies in this area. Medscape and UpToDate: The watershed areas of the colon (the splenic flexure and rectosigmoid junction) have more limited collateral networks and are also vulnerable to low flow states.
on STEP 1
- The left renal vein may be compressed by an aneurysm of the SMA as the vein crosses anterior to the aorta. Patients with compression of the left renal vein may have renal and adrenal hypertension on the left, and, in males, a varicocele on the left.

What duct does bile enter and leave from the gallbladder? What duct (from the liver) does this duct join?
Together, what do these ducts form?
The gallbladder lies in a fossa on the visceral surface of the liver to the right of the quadrate lobe. It stores and concentrates bile, which enters and leaves through the cystic duct. The cystic duct joins the common hepatic duct to form the (common) bile duct .
What is the pathway of the common bile duct? (what structures does it come into contact with, what is the rship of it with other structures)
The common bile duct penetrates the head of the pancreas where it joins the main pancreatic duct and forms the hepatopancreatic ampulla, which drains into the second part of the duodenum at the major duodenal papilla (sphincter of Oddi).

Where does the accessory pancreatic duct enter the duodenum?
What is in the porta hepatis/portal triad?
- Into the second part of the duodenum at the minor duodenal papilla (Superior to the major duodenal papilla)
- common bile duct, proper hepatic artery, portal vein

Where does the hepatic portal vein receive blood from?
Once blood enters the hepatic portal vein, where does it go? (within the liver and how it exits the liver)
What veins form the hepatic portal vein? What part of what organ does this happen posterior to?

Hepatic Portal System - an extensive network of veins that receives the blood flow from the GI tract. (note that the vena cava does not receive blood directly from the GI tract).
• Venous flow is carried to the liver via the hepatic portal vein where it enters the liver sinusoids, which drain to the hepatic veins, which then drain into the IVC.
• The hepatic portal vein is formed by the union of the superior mesenteric and splenic veins posterior to the neck of the pancreas.
• The inferior mesenteric vein usually drains into splenic vein.

What does the caval system drain? What does the IVC drain?
What veins come together to form the IVC? At what vertebral level does this occur?
What side of the body is the IVC on?
At what vertebral level does the IVC enter the diaphragm?
The caval system drains the head and neck, extremities, pelvis and perineum, paired abdominal viscera and body walls.
Inferior Vena Cava (IVC) - forms to the right of the lumbar vertebrae and the abdominal aorta by the union of the 2 common iliac veins at the L5 vertebral level.
• IVC ascends to the right of the midline and passes through the caval hiatus of the diaphragm at the T8 vertebral level.
• IVC receives blood from the lower limbs, pelvis and perineum, paired abdominal viscera, body wall AND the liver.
What are 3 sites of portacaval anastamoses? What are the portal and caval veins that anastomose? What are clinical signs seen when portal vein blood flow into the liver is reduced?
There are sites of anastomoses between the portal system and caval venous flow that can be utilized when portal vein blood flow into the liver is reduced.




