Endocrine responses to normal disturbances week 5 Flashcards
(28 cards)
Explain the change in ATP demand and oxygen uptake when going from rest to exercise.
How is ATP initially produced during this transition? (what are the 2 sources of ATP)
• ATP demand & production increases immediately
• Oxygen uptake increases rapidly
Initial Oxygen deficit
– lag of oxygen uptake at beginning of exercise
– uptake reaches steady state after 1-4 min (VO 2)
• Initial ATP production through anaerobic pathways
① ATP- phosphocreatine system
② Glycolysis

Where in the body is 95% of phosphocreatine contained?
What is creatine kinase activated by?
How long do phosphocreatine stores last?

What is lactate threshold? How does lactate threshold compare in trained subjects to untrained?
What is used to buffer lactate in the blood? How does lactate accumulation lead to increased respiration?
- Exercise intensity measured as percentage of max. oxygen uptake (VO2max)
- blood lactate increases with exercise intensity
- Lactate threshold (LT) depicts the VO2 a which lactate exceeds the resting variation
- LT is higher in trained subjects
Lactate then:
- accumulates in the blood
- is buffered by bicarbonate resulting in CO2
- VO2 unrelated respiratory stimulus

What are the fates of lactic acid released into the bloodstream? What is the major pathway?
What type of exercise promotes the most rapid lactic acid removal?
- Classical theory – Majority of lactic acid converted to glucose in liver (Cori Cycle)
- Recent evidence – 70% of lactic acid is oxidized -Lactate shuttle: lactate produced in one muscle/tissue can be transported and used as a substrate by heart, brain and skeletal muscle (pyruvate –> acetyl-CoA –>Krebs cycle)
– 20% converted to glucose
– 10% converted to amino acids
Lactic acid removal
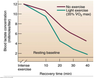
– more rapidly with light exercise in recovery
– Optimal intensity is < 40% VO2 max
Explain the difference in the rest to exercise transition btwn trained and untrained individuals.
What are the differences attributed to? What is the difference in lactate production?

What is respiratory quotient (RQ)?
What is the RQ for glucose?
What does the RQ usually reflect?
What assumption is the RQ based on?
When is the RQ not representative of cellular metabolism?
RQ= CO2 produced/O2 consumed

What is the primary fuel source utilized during low intensity exercise? During high intensity?

What is the primary source of fats during high intensity exercise? What organ produces this fat?
What is the primary source of fat during low intensity exercise? Where in the body is this fat released from? Why is this source more important during prolonged exercise?
• Intramuscular Triglycerides
– primary source of fat during high-intensity exercise
• Plasma Free Fatty Acids
– from adipose tissue lipolysis (TG –> glycerol + FFA depends on lipases) – FFA converted to acetyl CoA –> Krebs cycle – primary source during low-intensity exercise (< 30 % VO2 max)
– more important during prolonged exercise when muscle triglycerides decline
How/why does fat metabolism (B-oxidation) depend on carbohydrate metabolism?
What molecules does reduced levels of glycogen impact? (either result in increased or decreased levels)
Reduced muscle glycogen
• reduces glycolysis
– reduces pyruvate &
– Krebs cycle intermediates (e.g. oxaloacetate)
– reduces fat oxidation-not enough TCA cycle intermediates to process released ACoA
– increases in aceto-acetic and β-hydroxybutyric acid (keto acids)
– increases keto acid release into the blood stream

What is the primary source of glucose during high intesity exercise? (what organ supplies it)
What is the primary source of glucose during low intensity exercise? What organ supplies it? Why is this source important during prolonged exercise?
Muscle Glycogen
–primary source during high intensity exercise
–>70% VO2 max; 1h of exercise
Blood Glucose
–from liver glycogenolysis
–primary source during low-intensity exercise
–important during long duration exercise (muscle glycogen declines)

We always burn a mixture of fuels during exercise.

What hormones act first during exercise to increase plasma glucose? How long is it before their effects are seen?
What effects do these hormones have?
What part of the brain senses glucose? What does it do after it senses glucose?
Glucagon and Epinephrine act within minutes to raise plasma glucose
– Stimulation of hypothalamic glucose sensors –>
- Stimulates sympathetic activity
- Increased activity of the sympathetic nervous system –> – Attenuates β-cell release of insulin
– Increaes α-cell release of glucagon
True or False: E and NE release is proportional to exercise intensity and duration.
True.

True or false: E and NE released from the adrenal gland are of less significance than that released by the sympathetic nervous sytem.
True.

Explain the cellular mechanisms that epinephrine employs to increase muscle glycogenolysis.
In the absence of insulin (which is suppressed by E and NE), how do muscles take up glucose?
Epinephrine controls
• Muscle glycogen utilization
– G-protein – cAMP – glygogen phosphorylase
– increased [Ca]i , calmodulin activation also enhances Phosphorylase activity
Contractile activity of skeletal muscle stimulates continued glucose uptake in the absence of insulin. AMPK is stimulated by ATP/ADP ratios in the cell. During exercise, AMPK stimulates GLUT4 vesicles to fuse with the cell membrane in the absence of insulin.

What happens to aldosterone levels during exercise? (increase or decrease)
Explain the mechanisms.
Aldosterone:
• increases during exercise
– increase depends on %VO2max
- increase proportional to increase in Renin and AngII
- Renin is released due to decreased renal blood flow
-increased renal resistance ( due to epinephrine)
- decreased [Na]o, increased [K]o
- decreased extracellular fluid
stress (via CRH –> ACTH) also stimulates aldosterone release

What are the effects of aldosterone?

What are 2 effects of cortisol and growth hormone? When do these hormones begin to effect metabolism?
Cortisol and Growth Hormone are ‘late responders’
• Stimulation of the Hypothalamic – Pituitary Axis
– Limit glucose utilization
– Facilitate glucose production
– Their impact is delayed (~6 hrs)
Likely play larger role after exercise during recovery
What are the relative levels of ACTH and cortisol (increase or decrease during exercise?

How do cortisol levels change during low intensity exercise? High intensity exercise?
What stimulates the release of cortisol?
• During Exercise
– decreased at low intensity
– increased at high intensity
• Stimulated by
– exercise
– stress (via ADH and ACTH)
• Slow process
– rather repair of damage than maintenance of activity

What are the effects of cortisol on the effectivness of insulin?
In the presence of cortiol, higher insulin levels are required to stimulate glucose production.

What is the effect of cortisol on the immune response?

What induces GH (growth hormone) release?
How long does GH activation take?
What is the overall effect of GH?
Like Cortisol, GH is a long term hyperglycemic hormone
• GH is induced by:
– GHRH release from hypothalamus
– stress
– sharp decrease in glucose, FFAs or increased amino acids
– ghrelin (gastric glands and hypothalamus) stimulates GH release (antagonizing leptin and insulin action in the hypothalamus)
• GH activation takes hours and days
– overall decreases glucose utilization

What are the effects of GH? Explain its effects on the liver, its metabolic effects, and its anabolic effects.
Anabolic Action of GH:
- postnatal somatic growth & development
- modulates metabolism and body composition
- promotes protein synthesis by hypoaminoacidemia
– reflected in nitrogen retention and decreased urea production







