MSCT Week 1: Connective Tissue, Cartilage and Bone Flashcards
The stroma
structural support and connecting framework provided by connective tissue
ECM AKA
Extracellular Matrix
Ground Substance AKA
ECM
Ground substance consists of?
represents a combination of collagens, noncollagenous glycoproteins, and proteoglycans surrounding the cells of connective tissue
The resident cell of connective tissue is?
The fibroblast which is responsible for the production and maintenance of the ECM
Immigrint cells to the connective tissue include…
- macrophages
- mast cells
- plasma cells
has an important role in immune and inflammatory responses and tissue repair after injury
connective tissue
types of connective tissue proper

Types of specialized connective tissue
4 listed

Where is loose connective tissue typically found?
surrounding blood vessels, nerves, and muscles
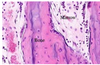
Identify


Dense connective tissue contains more _________ than _____________.
- fibers
than
- Cells
Loose connective tissue contains more _________ than _____________.
- Cells
than
- Fibers
When the collagen fibers are preferentially oriented as in tendons, ligaments, and the cornea the tissue is?
Dense Regular connective tissue
when collagen fibers are randomly oriented as in the dermis of the skin and wall of the intestine the tissue is called?
Dense irregular connective tissue
Dense _______ connective tissue is poorly vascularized.
Regular
Identify

Dense regular Connective Tissue

Identify
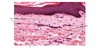
Dense irregular connective Tissue

Glycosaminoglycans AKA
GAGs
GAGs AKA
Glycosaminoglycans
Glycosaminoglycans are?
- long unbranched polysaccharides consisting of repeating disaccharide units
- Thes molecules are highly negatively charged and associate with large amounts of water to create hydrated gels with high viscosity and low compressibility
Glycosaminoglycans charge
Glycosaminoglycans are highly negatively charged and associate with large amounts of water to create hydrated gels with high viscosity and low compressibility
Glycosaminoglycans of physiological significance
6 Listed
- hyaluronic acid
- dermatan sulfate
- chondroitin sulfate
- heparin
- heparan sulfate
- keratan sulfate
What are these?