Embryos - Pregnancy Flashcards
how does the uterus change during pregnancy
- myometrium grows markedly
- muscle fibres hypertrophy and increase in number
- 3 LAYERS OF MUSCLE
outer longitudinal
middle interlacing
inner circular
- CT becomes more vascular
uterus and pelvic floor changes
what is the upper uterine segment attached to
peritoneum is intimately attached to upper uterine segment
loose and mobile all over the segment
uterus supports hypertrophy
broad ligaments show hypertrophy of all their content
levatores anii muscles hypertrophy and become softer ⇒ pelvic floor becomes progressively more distensible, thereby facilitating passage of the foetus

change in uterine blood supply
blood supply increases
uterine and ovarian arteries become large and very tortuous
PROTECTIVE FUNCTION:
lymphatics, like BVs, increase in size and number
large lymph spaces beneath the decidua and a well developed plexus under the enveloping peritoneum

what happens from 2nd month onwards
describe blood supply by 9th month
hypertrophy of BVs and lymphatics produces progressive softening of whole body
by 9th month, the whole of uterus and outer pelvic viscera are so engorged with the blood and lymph that the outlines of the various organs become vague and difficult to define
size and position of uterus
how does the position of uterus change throughout pregnancy
non-pregnant uterus = 2.5x5.7.5cm
full term = 23x25x30cm
uterus lies in true pelvis at 1st but by week 12 the fundus is level with the top of the symphysis pubis
by week 16 it lies mid way between the symphysis pubis and the umbilicus

What might a woman experience towards the end of a pregnancy
lightening as the baby moves down
position of uterus @ 20 weeks and 24 weeks
change in position throughout pregnancy
20 weeks - below umbilicus
24 weeks - just above it
⇒ fundus rises 2 fingerbreadths every 4 weeks until 36 weeks when it lies @ xiphisternum
between 36 and 40 weeks it drops by 1 fingerbreadth per week and @ week 40 it lies at the same level that it had reached @ week 32
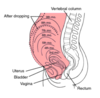
what causes the lightening in the last month
due to descent of foetal head into cavity of true pelvis
although the woman may feel more comfortable and may breathe more easily after lightening has occurred, she may notice frequency of micturition due to lack of space in the pelvis

role of cervix
passive role
cervical blood vessels and lymphatics hypertrophy thereby causing progressive softening which may be detected very early in pregnancy
connective and muscular tissues, although they both become more vascular and softer, they do not undergo hyperplasia

change in cervical mucosa
hypertrophies markedly until it constitutes nearly half of cervix @ full term
eventually, complex of glands resembles a honeycomb full of sticky tenacious mucus
when this protective mucus plug is expelled at onset of labour, it carries most of honeycombed mucosa with it
external os comes to have anterior and posterior lip, especially in multiparae
deep purple - engorged with blood

how does the isthmus and lower uterine segment change
approx upper 1/3 of cervix = isthmus
unaffected in 1st month of pregnancy
dilates and is taken up into body of uterus to form the lower uterine segment
the foetal membranes are less firmly blended with the mucosa in the isthmus than elsewhere
the endometrium lining the lower segment does not undergo a full decidual change
changes in vagina
similar to uterus
blood supply increases enormously - deep violet colour
hypertrophy of wall increases both length and width of vaginal canal
changes in vulva
undergoes similar changes - increased blood and lymphatic supply
progressive softening
changes in breasts
what happens at week 8
during the 1st 6 months - duct system proliferates
during the last 3 months - alveoli proliferate
also in alveoli, there is hypertrophy of BVs and lymphatics which supply them
WEEK 8 - Montgomery’s tubercles (mouths of enlarged sebaceous glands) become prominent in areola
WEEK 12 - darkening of primary areola occurs
WEEK 16 - a paler, secondary areola forms (more noticeable in dark-haired women)

abdominal viscera changes
what is a common complication of pregnancy
stomach is displaced upwards during the 2nd half of pregnancy
diaphragmatic herniation is a common complication of pregnancy

change in pelvis during pregnancy
symphyseal, sacroiliac and sacrococcygeal joint capsules soften and relax
reaches a maximum about week 28 and may cause sacroiliac back ache
may be accompanied by pain and tenderness in the symphysis

changes in skin
deposition of melanin occurs in certain areas in the body - particularly dark haired women
in midline of abdominal wall - linea nigra
chloasma uterinum
melanin deposition on forehead and cheeks

moulding
fetal cranium is relatively deformable
bones of calvaria are thin and elastic and can alter their shape to some extent
they are attached to 1 another by relatively loose fibrous sutures
they can override one another somewhat in response to compression forces as the head is squeezed down through the pelvis
this is limited
must be sufficient prior congruity to permit first engagement and then passage of foetus through the pelvic cavity

boundaries of pelvic inlet
angle it makes with pelvic floor
heart-shaped - bounded posteriorly by sacral promontory, laterally by iliopectineal line and anteriorly by symphysis pubis
plane of pelvic inlet makes an angle of 60° with that of pelvic floor
true conjugate diameter
measured from top of symphysis pubis to sacral promontory and averages about 4.5 inches
oblique diameter of pelvis
measured from sacroiliac joint to obturator foramen of opposite side and averages 4.75 inches
transverse diameter of pelvis
widest measurement from side to side and averages 5.25 inches
boundaries of pelvic cavity
measurement of diameters
bounded anterioly by symphysis pubis and posteriorly by sacrum and coccyx
diameter is usually taken at the level of junction of 2nd and 3rd sacral vertebrae posteriorly and middle of symphysis anteriorly
anteroposterior, oblique and transverse = 12cm










