Bio: Ch 7, 11 Flashcards
cardiovascular system consists of
muscular 3 chambered heart, blood vessels, blood
heart is composed of ____ muscle
cardiac
pulmonary circulation
right side of heart accepts deoxygenated blood returning from body and moves it to the lungs by way of pulmonary arteries
systemic circulation
left side of the heart receives oxygenated blood from lungs by way of pulmonary veins and forces it out to the body through aorta
atria
thin walled structures where blood is received from either the venae cavae or pulmonary veins
contract to push blood into ventricles
ventricles
thick walled structures that send blood to lungs (rt) and systemic circulation (lt)
atria are separated from the ventricles by
atrioventricular valves
bicuspid/mitral (lt) and tricuspid (rt)
(LAB RAT)
ventricles are separated from vasculature by
semilunar valves
tricuspid valve
valve between rt atrium and rt ventricle
(LAB RAT)
mitral/bicuspid valve
valve between lt atrium and lt ventricle
(LAB RAT)


pulmonary valve
valve that separates rt ventricle from pulmonary circulatory circulation
aortic valve
valve that separates left entricle from the aorta
the ___ side of the heart is more muscular than the other side because
left
the blood is pumped to the whole body –> higher resistance and pressure
pathway of blood
venae cavae (from body) > right atrium > tricuspid valve > right ventricle > pulmonary valve > pulmonary artery > lungs > pulmonary veins > left atrium > mitral valve > left ventricle > aortic valve > aorta (to body)

SA node
impulse intiation
systole
ventricular contraction
blood is pumped out of ventricles
when AV valves are closed
bundle of His
spread signal to interventricular septum
purkinje fibers
distribute electrical signal through ventricular muscle
intercalculated disk
connect muscle cells
contain many gap junctions directly connecting cytoplasm of adjacent cells
allows for coordinated ventricular contraction
diastole
heart is relaxed
blood fills ventricles
semilunar valves are closed


electric conduction steps
- SA node: impulse initiation
- atria contract
- AV node: pauses signal to allow the ventricles to fill fully
- bundle of his
- purkinje fibers
- ventricles contract

vagus nerve
slows down the heart rate
cardiac output
CO
total blood volume pumped by a ventricle in a mine
heart rate
HR
beats per minute
stroke volume
SV
volume of blood pumped per beat
cardiac output eq
CO = HR x SV
what does the sympathetic nervous system do to the cardiovascular system?
increases heart rate and contractility
what does the parasympathetic nervous system do to the cardiovascular system?
decreases heart rate
arteries
thick, highly muscular structures with an elastic quality –> allows for recoil and helps to propel blood forward within the system
arterioles
small muscular arteries
control flow into capillary beds
capillaries
have walls that are one cell thick
sites of gas and solute exchange
veins
inelastic, thin walled structures that transport blood to heart
can stretch but do not have recoil capability
compressed by surrounding skeltal muscles and have vales to maintain one way flow
endothelial cells
line blood vessels
help maintain vessel by releasing chemicals that aid in vasodilation and vasoconstriction
allow white blood cells to pass through
why do veins have valves?
bloodflow in most veins is upward against gravity and pressure is high at the bottom of the veneous column
veins need valves to push blood forward and prevent backflow
superior vena cava
returns blood form the body above heart
inferior vena cava
return blood from below heart
portal system
blood passes thorugh two capillary beds in series
hepatic portal system
blood travels from gut capillary beds to liver capillary bed via hepatic portal vein
hypophyseal portal system
blood travels from capillary bed in hypothalamus to capillary bed in anterior pituitary to allow for paracrine secretion of releasing hormones
renal portal system
blood travels from glomerulus to vasa recta through efferent arteriole




if all autonomic input to the heart were cut, what would happen?
heart would continue beating at the intrinsic of the pacemaker (SA node)
they would be unable to change their heart rate via the sympathetic or parasympathetic nervous system, but the heart would not stop beating
plasma
liquid portion of blood
aqueous mixture of nutrients, slats, respiratory gases, hormones, and blood proteins
categories of the cellular portions of blood
erythrocytes, leukocytes, platelets
blood cells are formed from
hematopoietic stem cells
erythrocytes lack ____ because…
mitochondria, nucleus, and organelles
to make room for hemoglobin
hemoglobin
protein that binds four molecules of oxygen
hematocrit
percentage of blood composed of erythrocytes
erythrocyte
specialized cell designed for oxygen transport
why are red blood cells biconcave?
assists them in travelling through capillaries
increases cell’s surface area, which increases gas exchange
how do blood cells generate ATP
rely on glycolysis for ATP, with lactic acid as main byproduct
(cannot carry out oxidative phosphorylation)
leukocytes
white blood cells
part of immune system
leukocytes
types
granulocytes and agranulocytes
granulocytes/granular leukocytes
+ex
play role in nonspecific immunity -> contain compounds that are toxic to invaders
neutrophils, eosinophils, basophils
agranulocytes
+ex
play role in immunity
lymphocytes and monocytes
lympthocytes
important in specific immune response
specific immune response
body’s targeted fight against particular pathogens
thrombocytes/platelets
cell fragments from megakaryocytes
blood clotting
hematopoiesis
production of blood cells and platelets
thrombopoietin
secreted by liver and kidney and stimulates mainly platelet develop
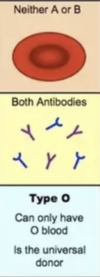
blood antigens
A, B, O, Rh factor (D)
blood antigens dominance
A and B are codominant
i (O) recessive
Rh+ is dominant
universal donors
type O blood
don’t produce any antigens
universal recipients
type AB
don’t produce any antibodies
B+ blood can recieve blood from to
B+, B-, O+, O-
B+ blood can donate to
B+, AB+
why cell types contain nuclei and which do not?
nuclei: leukocytes
none: erythrocytes, platelets
blood pressure
force per unit area that is exerted on walls of blood vessels by blood
divided into systolic and diastolic components
blood pressure must be high enough to ___, but it must be low enough to ___
high enough to overcome the resistance created by arterioles and capillaries
low enough to avoid damaging the vasculature and surrounding structures
sphygmomanometer
measures blood pressure
blood pressure is maintained by
baroreceptor and chemoreceptor reflexes
low blood pressure promotes ___ and ___ release
aldosterone and ADH
high blood osmolarity promotes ___ release
ADH
high blood pressure promotes ____ release
ANP
gas and solute exchange in capillaries relies on
concentration gradients
gas and solute exchange in capillaries
capillaries are leaky
conc gradients
blood vessels
hydrostatic pressure
pressure of the fluid within the blood vessel
psuhes fluid out at arteriole end of capillary
blood vessels
osmotic pressure
due to proteins
draws fluid back into vessel at venule end
largest drop in blood pressure occurs
across the arterioles
important bc capillaries cannot withstand so much pressure
the longer a blood vessel is, the ___ resistance it offers
more
the larger the cross sectional area of a blood vessel, the ___ resistance it offers
less
baroreceptors
detect changes in mechanical forces on the walls of the vessel
chemorecetpors
sense when osmolarity of the blood is too high, which could indicate dehydration
oxygen saturation
percentage of hemoglobin molecules carrying oxygen
cooperative binding in oxygen
each successive oxygen bound to hemoglobin increases the affinity of the other subunits, while each successive oxygen released decreases the affinity of the other subunits
in lungs, there is a ___ partial pressure of oxygen, resulting in…
high
loading of oxygen onto hemoglobin
in tissues, there is a ___ partial pressure of oxygen, resulting in
unlading of oxygen onto hemoglobin
carbon dioxide is largely carried in blood in the form of
carbonic acid, bicarbonate, and hydrogen ions
what can cause a right shift in the oxyhemoglobin dissociation curve? what does this result in?
results in decreased affinity for oxygen
- high PaCO2
- high [H+]/low pH
- high temp
- high [2,3-BPG]
coagulation results from
activation cascade
coagulation cascade steps
- endothelial lining of a blood vessel is damaged
- collagen and tissue factor underlying the endothelial cells are exposed
- results in formation of a clot over damaged area
- platelets bind to collagen and stabilized by fibrin
- clots broken down by plasmin
clots
composed of coagulation factors (proteins) and platelets
prevent blood loss
coagulation factors are secreted by
liver
coagulation factors
sense tissue factor and initiate a complex activation cascade
fibrin is activated by
thrombin
plasmin
breaks down clots
fibrin
stabilizes clots
where should you look on the oxyhemoglobin dissociation curve to determine the amount of oxygen that has been delivered to tissues?
drop in y value (% hemoglobin saturation)
what direction does the oxyhemoglobin dissociation curve shift as a result of exercise?
right
represents hemoglobin’s decreased affinity for oxygen, which allows more oxygen to be unloaded at the tissues
What is the role of the Chordae Tendinae and Papillary Muscles?
The Papillary Muscles contract to pull on the valves via the Chordae Tendinae during a ventricular contraction. This helps prevent blood from flowing back into the Atria from the Ventricles.

Place the following layers of the heart in order from inside to out.
I. Endocardium
II. Pericardium
III. Myocardium
(A) I > II > III
(B) II > I > III
(C) I > III > II
(D) II > III > I
(C) I > III > II
From inside to outside: Endocardium –> Myocardium –> Pericardium
In questions like these, if you can understand the prefix meanings, it’s a lot easier. For instance, “endo” means inside or within.
Which of the following structures is known for connecting cardiac muscle cells and ensuring this coordination in contracting?
(A) The AV Node
(B) The bundle of His
(C) Interventricular Septum
(D) Intercalated Discs
(D) Intercalated Discs
The Intercalated Discs are known for connecting cardiac muscle and ensuring coordination while contracting.
Which of the following appropriately maps the pathway of Electrical Conduction in the heart?
I. Neural Input
II. Bundle of His
III. AV Node
IV. SA Node
V. Purkinje Fibers
(A) I > II > III > IV > V
(B) I > IV > III > II > V
(C) IV > III > II > V
(D) I > II > IV > V
(C) IV > III > II > V
The Electrical Conduction Pathway in the heart is:
- SA Node
- AV Node
- Bundle of His
- Purkinje Fibers
CRB If neural input is not needed by the SA Node for generating contractions normally, then why is the SA Node innervated?
The SA Node can be affected by neural input to either speed up or slow down the rate of contraction!
CRB True or false? The depolarization wave spreading from the SA Node also causes the atria to contract, increasing cardiac output by up to 30%.
True. The depolarization wave spreading from the SA Node also causes the atria to contract, increasing cardiac output by up to 30%.
Which of the following is the proper description of the Frank-Starling Mechanism, which also affects Cardiac Output?
(A) Stretching the heart will increase stroke volume and cardiac output, so filling the heart with less blood will increase the Cardiac Output.
(B) Heartrates can increase to increase Cardiac Output, but only to a point of diminishing returns.
(C) Stretching the heart will increase stroke volume and cardiac output, so increasing Venous Return will increase Cardiac Output.
(D) Increased Cardiac Output can stress the heart, so Venous Return is always kept to the minimum necessary to power life.
(C) Stretching the heart will increase stroke volume and cardiac output, so increasing Venous Return will increase Cardiac Output.
Match the following terms with their respective function.
(1) Pulmonary Capillaries
(2) Systemic Capillaries
(A) Blood loses oxygen and gains carbon dioxide
(B) Blood loses carbon dioxide and gains oxygen
(1) Pulmonary Capillaries – (B) Blood loses carbon dioxide and gains oxygen
(2) Systemic Capillaries – (A) Blood loses oxygen and gains carbon dioxide
Pulmonary circulation entails blood exchanging CO2 for O2. Systemic circulation entails delivering O2 to the cells of the body in exchange for CO2.
Which of the following occur during the first heart sound (AKA Lub), also called S1.
I. Mitral & Tricuspid valve close
II. Mitral & Tricuspid valve open
III. Pulmonary & Aortic valve open
IV. Pulmonary & Aortic valve close
(A) I only
(B) I and IV only
(C) I and III only
(D) II and IV only
(C) I and III only
During S1, the mitral and tricuspid valves close (which causes the “Lub” sound) and the pulmonary and aortic valves open.

Which of the following occur during the second heart sound (AKA Dub), also called S2.
I. Mitral & Tricuspid valve close
II. Mitral & Tricuspid valve open
III. Pulmonary & Aortic valve open
IV. Pulmonary & Aortic valve close
(A) I only
(B) I and IV only
(C) I and III only
(D) II and IV only
(D) II and IV only
During S2, the pulmonary and aortic valves close (which causes the “Dub” sound) and the mitral and tricuspid valves open.

Which of the following statements about Venules is true?
(A) Venules are larger than Veins.
(B) Venules lead to the Veins.
(C) Venules have lower blood pressure than Veins.
(D) At least two of the above statements are true.
(B) Venules lead to the Veins.
The order of bloodflow goes capillary > Venule > Larger Vein.

The heart is pumping the blood out, so arteries are under ____ pressure with ____ volume. Veins are under ____ pressure with ____ volume.
(A) High; Low; High; Low
(B) High; Low; Low; High
(C) High; High; Low; Low
(D) High; High; High; High
(B) High; Low; Low; High
Arteries have high pressure and low volume.
Veins have low pressure and high volume.

High resistance would result from vasoconstriction or vasodilation?
Vasoconstriction would cause a high resistance.

Increasing which of the following could increase Blood Pressure?
I. The force of Cardiac Contractions
II. The rate of Cardiac Contractions
III. Increasing Precapillary Sphincter Diameters
(A) I and II only
(B) I and III only
(C) II and III only
(D) I, II and III
(A) I and II only
Each of the following could increase Blood Pressure:
I. The force of Cardiac Contractions
II. The rate of Cardiac Contractions
III. Decreasing Precapillary Sphincter Diameters
Which of the following relationships between Systolic and Diastolic Pressure is accurate in a healthy adult?
(A) Systolic Pressure > Diastolic Pressure
(B) Systolic Pressure = Diastolic Pressure
(C) Systolic Pressure < Diastolic Pressure
(D) More than one of the above answers is possible
(A) Systolic Pressure > Diastolic Pressure
As a sign that the heart is effectively pumping blood, Systolic Pressure must be higher than Diastolic Pressure in a healthy adult.
Which of the following are present inside the blood vessel under normal conditions, floating around with blood cells?
I. Platelets
II. Collagen
III. Fibrin
(A) I and II only
(B) II and III only
(C) III only
(D) I only
(D) I only
Of the following choice, only platelets are floating around in the blood vessel with blood.
Collagen is present outside of the blood vessel.
Fibrinogen is found inside the blood vessel under normal conditions, not fibrin.
True or False? While red blood cells do not have a nucleus, their precursors do.
True. While red blood cells do not have a nucleus, their precursors do.
In a normal adult, blood has the least amount of:
(A) Plasma
(B) White Blood Cells
(C) Red Blood Cells
(D) Water
(B) White Blood Cells
Less than 1-percent of blood is made up of white blood cells and platelets.

Which of the following cannot be found in the Plasma Layer?
(A) Antibodies
(B) Electrolytes
(C) Platelets
(D) Clotting Factors
(C) Platelets
Blood Plasma is composed of:
90% Water
8% Proteins (Albumin, Antibodies, etc)
2% Hormones, Electrolytes, and Nutrients
Platelets and White Blood Cells are found in the Buffy Coat Layer.
The Red Blood Cell Layer only contains Red Blood Cells. But don’t forget that Hemoglobin and other proteins are found within Red Blood Cells.

True or False? The only way for oxygen to be transported in the blood is through hemoglobin.
False. A very small percentage of oxygen will diffuse right into the plasma.
Which of the following are reasons for oxygen delivery into the tissues?
I. High partial pressure of oxygen in the tissues
II. H+ competes with oxygen for hemoglobin
III. CO2 competes with oxygen for hemoglobin
(A) I only
(B) II only
(C) II and III only
(D) I, II, and III only
(C) II and III only
H+ and CO2 compete with oxygen for hemoglobin, decreasing the affinity of oxygen for hemoglobin, causing oxygen to be released into the tissues.
The partial pressure of oxygen is LOW in the tissues, which is another reason why oxygen diffuses into the tissues.
In which direction, right or left, does the below reaction move when oxygen delivery to the tissues is occurring? What about when carbon dioxide is being delivered to the lungs?
CO2 + H20 <=> H2CO3 <=> HCO3 + H+
The equation is moving to the right during oxygen delivery to the tissues. This is due to the increasing amount of CO2 entering from the blood stream.
The equation is moving to the left during carbon dioxide delivery to the lungs. This is due to the decreasing amount of CO2 in the blood stream.
These two scenarios are based on Le Chatlier’s Principle.
During inhalation in the lungs, the partial pressure of carbon dioxide is _______, and the partial pressure of oxygen is _________.
(A) high, high
(B) high, low
(C) low, low
(D) low, high
(D) low, high
During inhalation in the lungs, the partial pressure of carbon dioxide is low, and the partial pressure of oxygen is high.
Draw the oxygen-hemoglobin dissociation curve. What is on the y-axis? What is on the x-axis? What is the shape of the curve and why?
The y-axis is the percent saturation of hemoglobin with oxygen.
The x-axis is the partial pressure of oxygen.
The curve is sigmoidal due to the cooperativity effect.
Once one oxygen binds to hemoglobin, it is easier for the remaining oxygens to bind, until there are no more spots for oxygen.

Draw the carbon dioxide-hemoglobin dissociation curve. What is on the y-axis? What is on the x-axis? What is the shape of the curve and why?
The y-axis is the percent saturation of hemoglobin with carbon dioxide.
The x-axis is the partial pressure of carbon dioxide.
The curve is a straight line because there is no cooperativity in the binding of CO2 to hemoglobin.

What antigens do people with Blood Type A contain? What antibodies do people with Blood Type A contain? People with Blood Type A may receive a blood donation from individuals of which blood types?

Why does a person with Blood Type A have antibodies against Antigen B but not against Antigen A?
A person with Blood Type A will generate antibodies against foreign antigens because these are likely part of an invader. For this reason, people with blood type A will generate antibodies against Antigen B (an antigen not found in its own body) and not against Antigen A (an antigen found in its own body).

Why can’t a person with Blood Type A receive blood from a person with Blood Type B?
The recipient with Blood Type A contains Anti-B Antibodies in their bloodstream. If they received a blood donation from a donor with Blood Type B, the Anti-B Antibodies in the recipient’s bloodstream would attack the donor’s blood cells since they have Antigen B on them. This results in serious inflammation and stress within the recipient’s bloodstream.

What antigens do people with Blood Type O contain? What antibodies do people with Blood Type O contain? People with Blood Type O may receive a blood donation from individuals of which blood types?
main types of muscle
skeletal, smooth, cardiac
skeletal muscle
function
support and movement
propulsion of blood in venous system
thermoregulation
skeletal muscle
structure
striated
polynucleated
skeletal muscle
types
red fibers, white fibers
skeletal system is under ___ control
somatic/voluntary
red fibers
aka slow twitch fibers
have high myoglobin content
carry out oxidative phosphorylation
white fibers
aka fast twitch fibers
have less myoglobin
carry out anaerobic metabolism
smooth muscle
respiratory, reproductive, cardiovascular, and digestive system
capable of more sustained contractions than skeletal muscle
can display myogenic activity
smooth muscle
structure
nonstriated
uninucleated
smooth muscle is under ___ control
autonomic
myogenic activity
do not require nervous system input to contract
(still respond to nervous input)
cardiac muscle
contractile tissue of the heart
can display myogenic activity
cardiac muscle is under ___ control
autonomic
cardiac muscle
structure
striated
uninucleated (sometimes binucleated)
cells connected with intercalated discs
sarcomere
basic contractile unit of striated muscle
made of thick (myosin) and thin (actin) filaments

tonus
constant state of low level contraction
seen in blood vessels
all muscles require ____ for contraction
Ca2+
thick filaments
organized bundles of myosin
thin filaments
organized bundles of actin
contain troponin and tropomyosin
titin
acts as a spring and anchors actin and myosin filaments together, preventing excessive stretching of the muscle
Z-lines
define the boundaries of sarcomere
M-line
located in middle of sarcomere
M - middle
I-band
contains only thin filaments
(I is a thin letter)
H-zone
contains only thick filaments
(H is a thick letter)
A-band
contains the thick filaments in their entirety
only part of sarcomere that maintains a constant size during contraction
during contraction, which parts of sarcomere change and how?
H-zone, I-band, distance between Z-lines, and distance between M-lines decrease
myofibrils
sarcomeres attached end to edn
myocyte/muscle fiber
contains many myofibrils
myofibrils are surrounded by ___
sarcoplasmic reticulum
sarcoplasmic reticulum
modified endoplasmic reticulum
contains high conc of Ca2+ ions
sarcolemma
cell membrane of myocyte
t-tubules
connected to sarcolemma and oriented perpendicularly to myofibrils
allow action potential to reach all parts of the muscle
muscle contraction steps
- acetylcholine released from neuromusclar junction
- acetylcholine binds to receptors on sarcolemma –> depolarization
- depolarization spreads to t-tubules –> Ca2+ ions released
- Ca2+ binds to troponin –> shift in tropomyosin and exposure of myosin binding sites on actin
- myosin heads bind to exposed sites on actin –> sarcomere shortens –> cross bridges form and pull actin along thick filament –> contraction

muscle relaxation steps
- acetylcholine degraded by acetylcholinesterase –> terminates the signal and allows Ca2+ to be brought back into SR
- ATP binds to myosin head, allowing it to release from actin
- sarcomere returns to original width
simple twitch
all or nothing response of muscle cells
consists of a latent period, contraction period, and relaxation period

motor end plate
nerve terminal in neuromsucular junction
motor unit
motor neuron and all of the myocytes innervated by the neuron’s axon terminals, including the neuromuscular junctions between the neuron and the fibers
actin myosin cross bridge cycle

sliding filament model
repetitive binding and releasing of myosin heads on actin filaments allows the thin filament to slide along thick filament, causing sequential shortening of sarcomere
latent period
time between reaching threshold and onset of contraction
actional potential spreads along muscle and allows for calcium to be released from SR
frequency summation
addition of multiple simple twitches before the muscle has an opportunity to fully relax
tetanus
simple twitches that occur so frequently that the muscle is unable to relax at all
oxygen debt
difference between the amount of oxygen needed and the amount present
muscle cells have additional energy reserves to…
reduce oxygen debt and forestall fatigue
additional energy reserves that muscle cells have include:
creatine phosphate and myoglobin
creatine phosphate
transfer a phosphate group to ADP, forming ATP
myoglobin
heme containing protein that is a muscular oxygen reserve
binds oxygen with a high affinity
muscles use them to keep aerobic metabolism going when muscles run out of oxygen
which zone or band in the sarcomere does not change its length during muscle contraction? why?
A-band - entire length of myosin filemnt
filaments do not change length, but instead slide over each other –>A band maintains a constant length
endoskeletons
internal skeletons
exoskeletons
external skeletons
human skeletal system can be divided into:
axial and appendicular skeletons
axial skeleton
consists of structures in midline
skull, vertebral column, rib cage, hyoid bone
appendicular skeleton
consists of the bones of the limbs, pectoral girdle, pelvis
bone is derived from
mesoderm
compact bone
provides strength
dense
spongy/cancellous bone
has lattice-like structure consisting of trabeculae
trabeculae
bony points
cavities between trabeculae are filled with
bone marrow
red marrow
filled with hematopoietic stem cells
yellow marrow
composed primarily of fat and is relatively inactive
long bones
contain shafts called diaphyses that flare to form metaphyses and terminate in epiphyses
epiphysis contains
epiphyseal (growth) plate
epiphyseal plate
causes linear growth of bone
periosteum
layer of connective tissue that surrounds the bone
ligaments
bone to bone
tendons
bone to muscle
bone matrix
has organic components (collagen, glycoproteins, peptides) and inorganic components (hydroxyapatite)
bone is organized into
concentric rings called lamellae
around a central haversian/volkman’s canal
osteon
structural unit of bone
lacunae
between lamellar rings
where osteocytes reside
canaliculi
connect lacunae
allow for nutrient and waste transfer
bone remodeling is carried out by
osteoblasts and osteoclasts
osteoblasts
build bone
osteoclasts
resorb bone
bones and parathyroid hormone
inc resportion of bone –> inc calcium and phosphate conc in blood
bones and vitamin D
increase resportion of bone –> increased turnover –> production of stronger bone
bones and calcitonin
increases bone formation
dec calcium concentrations in blood
cartilage
firm elastic material
avascular and not nucleated
found in areas that require more flexibility or cushioning
cartilage is secreted by
chondrocytes
chondrin
cartilage matrix
endochondral ossification
bone forms from cartilage during fetal life
intramembranous ossification
bones that form directly from undifferentiated tissue (mesenchyme)
ex skull
mesenchyme
undifferentiated embryonic connective tissue
joints may be classified as
immovable or movable
immovable joints
fused together to form sutures or similar fibrous joints
movable joints
contain synovial capsule
usually strengthened by ligaments
synovial fluid
aids in motion by lubricating the joint
synovial fluid is secreted by
synovium
articular cartilage
coats the bones in the join to aid in movement and provide cushioning
antagonistic pairs
muscles that serve opposite functions
when one muscle contracts, the other lengthens
origin
end of the muscle with a larger attachment to bone (usually the proximal connection)
insertion
end of the muscle with the smaller attachment to bone (usually the distal connection)
synergistic muscles
work together to accomplish the same function
flexor muscle
decreases the angle across a joint
extenso muscle
increases or straightens the angle across a joint
abductor muscle
moves a part of the body away from the midline
adductor muscle
moves a part of th ebody toward the midline
what chemical forms most of the inorganic component of bone?
hydroxyapatite crystals
Which of the following important proteins in muscles have ATPase activity?
I. Actin
II. Myosin
III. Titin
(A) II only
(B) I and II only
(C) I and III only
(D) I, II and III
(A) II only
Only Myosin has ATPase activity.
The myosin-actin crossbridge cycle consists of 4 main steps in which ATP is altered, resulting in the movement of a myosin head in relation to an actin filament. State what the myosin head does in response to each of the following:
(1) ATP binds to the myosin head.
(2) ATP is hydrolyzed, forming ADP and Pi.
(3) ADP and Pi dissociate from the myosin head.
Bonus: Be sure to use the terms “cocked” and “powerstroke”
(1) ATP binds to the myosin head. - The myosin head dissociates from the actin filament.
(2) ATP is hydrolyzed, forming ADP and Pi. - The myosin head cocks forward into its higher energy “cocked” conformation, binding to actin one rung higher than before.
(3) ADP and Pi dissociate from the myosin head. The myosin head does its powerstroke, pulling the actin filament. The myosin head remains attached to the actin filament as it waits for another molecule of ATP to bind and restart the cycle.
Note: This likely feels like a lot to memorize, but the AAMC will test you on it!
Which of these steps of myosin-actin crossbridge cycle could not occur if there was no actin?
(A) ATP binds to the myosin head.
(B) ATP is hydrolyzed, forming ADP and Pi.
(C) ADP and Pi dissociate from the myosin head.
(D) None of the above would fail to occur
(C) ADP and Pi dissociate from the myosin head.
This is the step that cannot occur if there is no actin, since the ADP dissociates due to conformational changes during the power-stroke that occurs when the myosin head is bound to actin.
Why doesn’t the actin filament slip back into its starting position each time the myosin head detaches from the actin?
This is due to the fact that there are many myosin heads interacting with the actin filament at a given time.

Describe the relationship between Ca2+, tropomyosin, troponin, myosin, and actin.
Tropomyosin is wrapped around the actin filament, covering up the mysosin binding sites. Troponin is what holds the Tropomyosin in place on the actin, and when Ca2+ binds to troponin, it will pull tropomyosin away from the binding sites, allowing myosin to bind to the actin filament, allowing the cross-bridge cycle to begin.
Via what mechanism does Ca2+ get back into the sarcoplasmic reticulum when it is time for muscle relaxation?
(A) Passive diffusion through the membrane
(B) Secondary active transport
(C) Passive diffusion through the ryanodine channels
(D) Primary active transport
(D) Primary active transport
When it is time for muscle relaxation, Ca2+ is transported back into the sarcoplasmic reticulum via a pump that utilizes ATP and is known as the Sarco-Endoplasmic Reticulum Calcium ATPase (SERCA).
The role of titin is to anchor _____________ to the ____________.
(A) myosin, Z-line
(B) myosin, M-line
(C) actin, Z-line
(D) actin, M-line
(A) myosin, Z-line
The role of titin is to anchor myosin to the Z-line.

True or False? All skeletal muscles are attached to tendons.
False. Not every skeletal muscle is attached to a tendon/bone. For instance, the external oblique muscle is attached to a different fibrous tissue known as an aponeurosis.
Which of the following muscle types are striated?
What does that mean? What is responsible for giving the muscle a striated appearance?
I. Smooth Muscle
II. Cardiac Muscle
III. Skeletal Muscle
(A) I Only
(B) III Only
(C) I and III Only
(D) II and III Only
(D) II and III Only
Cardiac and skeletal muscle are striated. They are striped due to the presence of sarcomeres arranged end-after-end, and the z-lines linking these sarcomeres gives that dark band appearance.
Which of the following are characteristics of smooth muscles?
I. Spindle shaped
II. Only 1 nuclei
III. Nuclei located in the periphery of the cell
(A) I only
(B) I and II only
(C) II and III only
(D) I, II and III
(B) I and II only
Smooth muscles are spindle shaped with only one nuclei in the center.

Which of the following are characteristics of cardiac muscles?
I. Branched
II. Can be Uninucleate or Multinucleate
III. Nuclei located in the periphery of the cell
(A) I only
(B) III only
(C) I and II only
(D) I, II and III
(C) I and II only
Cardiac muscles are branched. They typically have 1-3 nuclei that are located in the center of the cell.

Which of the following are ways that the force of contraction could be increased physiologically?
I. Recruiting larger motor units to contract.
II. Increasing the frequency of stimulation.
III. Increasing the activation of the Antagonistic muscles.
(A) I only
(B) I and II only
(C) II and III only
(D) I, II and III
(B) I and II only
Recruiting larger motor units to contract and increasing the frequency of stimulation can increase the force of contraction.
Do type 1 or type 2 muscle fibers fatigue easily? Do type 1 or type 2 muscle fibers resist fatigue?
Type 2 muscle fibers fatigue easily. Type 1 muscle fibers are fatigue resistant.
What is the role of Myoglobin in the muscles? Does it exhibit cooperativity?
Myoglobin is the oxygen storage molecule for the muscle. It is not cooperative, because it is made of only one subunit and can only bind one oxygen molecule.
Which of the following are sites for Hematopoiesis in adults?
I. Cancellous Bone
II. Compact Bone
III. Metaphysis
(A) I Only
(B) II Only
(C) I and II Only
(D) I, II, and III Only
(A) I Only
Cancellous Bone, also known as Spongy Bone, is the site of Hematopoiesis. In adults, this Hematopoiesis occurs in Red Bone Marrow, which is located in the Epiphysis (NOT the Metaphysis).
CRB True or false? Hematopoiesis depends upon its own Pluripotent stem cells, called Hematopoietic Stem Cells.
False. Hematopoiesis depends upon its own Multipotent stem cells, called Hematopoietic Stem Cells.
Draw a Long Bone and label it with the following parts:
(1) Diaphysis
(2) Metaphysis
(3) Epiphysis

Compare the role of red bone marrow versus yellow bone marrow.
Red bone marrow is responsible for hematopoeises while yellow bone marrow is responsible for fat storage.
In which part of an osteon will you find lymphatic vessels, blood vessels, and nerves?
(A) haversian canal
(B) lamellae
(C) canaliculi
(D) lacunae
(A) haversian canal
You will find lymphatic vessels, blood vessels, and nerves in the haversian canal of the osteon.
In which part of an osteon will you find osteocytes?
(A) haversian canal
(B) lamellae
(C) canaliculi
(D) lacunae
You will find osteocytes in the lacunae of osteon.
Which of the following cells are derived from monocytes?
(A) Osteoprogenitors
(B) Osteocytes
(C) Osteoblasts
(D) Osteoclasts
(D) Osteoclasts
Osteoclasts are derived from monocytes.
What effect does increased osteoblast activity have on the blood calcium and phosphate levels? What effect does increased osteoclast activity have on the blood calcium and phosphate levels?
Increased osteoblast activity will decrease the amount of calcium and phosphate in the bloodstream due to the use of calcium and phosphate in the formation of hydroxyapatite.
Increased osteoclast activity will increase the amount of calcium and phosphate in the bloodstream due to the release of calcium and phosphate from hydroxyapatite.
Too little calcium in the blood will result in which of the following?
I. Lethargy
II. Muscle cramps
III. Convulsions
(A) I and II only
(B) II and III only
(C) I and III only
(D) I, II, and III
(B) II and III only
Too little calcium in the blood will lead to muscle cramps and convulsions.


