Week 5 - E(1) - Kidneys in systemic disease - Diabetes & renovascular disease (causes) Flashcards
(40 cards)
What are macrovascular complications of diabetic nephropathy?
This would be Stroke Myocardial infarction Peripheral vascular disease
What are examples of microvascular complications of diabetic disease?
Retinopathy Neuropathy Nephropathy
What are the four types of diabetic neuropathy?
Peripheral neuropathy Autonomic neuropathy Proximal neuropathy Focal neuropathy
What are the features of peripheral neuropathy?
Peripheral neuropathy is usually where there is damage to the peripheries and there is a loss of sensation and ulceration can form in the feet and hands
What type of neuropathy would gastroparesis come under?
Would come under autonomic neuropathy - the autonomic nervous system is affected
What happens to the kidneys in the first stage of diabetic nephropathy?
In the first stage the GFR increases by about 25-50% due to renal hypertrophy
What does the plasma glucose stimulate in the kidneys to cause the increase in GFR at the beginning of diabetic nephropathy?
Plasma glucose stimulates the production of vasocative mediators eg IGF1 (insulin-like growth factor 1) This causevasodilation of the afferent arteriole and therefore an increase in filtration
After the renal hypertrophy that occurs in diabetic nephropathy, what takes place?
Mesangial expansion with glomerular basement membrane thickening
Nodule Formation and diffuse glomerulosclerosis follows the mesangial expansion What are the nodules known as on histology?
These nodules are known as Kimmelstiel Wilson nodyles
What happens in the overt diabetic nephropathy stage?
In the overt stage, there is proteinuria due to GBM thickening and podocyte dysfunction also with tubulointerstitial fibrosis
12 What is the first step in diabetic kidney disease? A – Inflammation B – Increased albuminuria C –Mesangial expansion D – Tubulo-interstitial fibrosis E – Increased eGFR F – Decreased eGFR G– Nodular diabetic sclerosis
E - Increased eGFR - also accompanied by renal hypertrophy in the pre nephropathy stage

What occurs in the overt stage of diabetic nephropathy?
Proteinuria - due to glomerular basement thickening and podocyte dysfunction Mesangial nodules (kimmelstiel Wilson nodules) and tubulointersitisal fibrosis
History of Diabetes Mellitus Albuminuria / Proteinuria Presence of other diabetic complications eg retinopathy What is a late finding in diabetic nephropathy?
Renal impairment

If already suspecting a histoy of diabetic nephropathy, a renal biopsy may not be required When would you carry out a renal biopsy?
Haematuria or if you supect there may be something that would alter your treatment plan
When measuring urine albumin excretion per day What is normal, what is microalbuminuria and what is overt nephropthy?
Normal is less than 30mg/day Microalbuminuria - 30-300mg/day Overt diabetic nephropathy - >300mg/day
In treating diabetic nephropathy, what is important as the initial treatment? (BP, glucose, astherosclerosis - what are the values for HbA1c and BP)
Get patinet under tight glycaemic control - HbA1c less than 7 (53%) Control blood pressure using ACEinhibitors or ARBs Lipids by giving statins
So for, diabetes - control is to give an ACEinhibtor, lipid control and tight glycaemic control What should you advise regarding diet?
Low salt diet and low fluid intake
If there is declining GFR below 20, what shoudl you inform the patinet about?
Inform the patinet about the likeliness to need dialysis
Is an older or younger type 1 diabetic likely to experience diabetic nephropathy?
A younger patient as they have more time for the kidney function to decline
Renal Replacement Therapy for Diabetic Nephropathy What are the three options?
Simultaneous kidney and pancreas transplant (type 1 only) Renal transplant Dialysis (haemo or peritoneal dialysis)
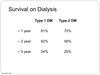
The survival on dialysis in a diabetic patinet is better in T1DM than T2DM What is the survival rates in T1DM? (at one, two and five years)
One year - 81% Two years - 62% Five years - 24%
What is the most common cause of renal failure in the UK? What does the microalbuminaemia progress to?
Diabetes is the most common cause Microalbuminaemia progresses to proteinuria and this produces to frank nephropathy
What drugs are used to treat proteinuria in diabetic nephropathy as this is very good for slowing down progression?
ACEinhibtors and ARBs
How do diabetic patients tend to cope on dialysis?
Diabetic patients tend to do badly on dialysis and cope better on transplant



