Ocular Pathology Flashcards
What ocular abnormality is present?

Corneal edema
MDx

MDx: cataract
Causes of corneal opacity
Corneal edema- MOST COMMON- fluid in the corneal stroma
– Injury to epithelium (ulceration)
– Injury to endothelium
• Cornealendothelial
dystrophy
• Increased IOP (Glaucoma) • Immune-mediated
– Keratitis–neovascularization has leaky capillaries
Corneal deposits – covered later

Corneal edema due to an ulcer
Ulcer stains green with flourescein dye

Corneal edema due to keratitis
Note gross features of inflammation

MDx: diffuse corneal edema
Corneal endothelial dystrophies
Inherited; breed predilections
Old age change
Bilaterally symmetrical foci of opacity which progress to diffuse opacity
Endothelial degeneration of unknown cause
It’s a gross diagnosis! - no histo!

MDx: diffuse corneal edema
Puppy that survived the acute phase of infectious canine hepatitis (CAV-1 infection); immune complex deposition in corneal endothelium
“Blue Eye”

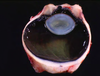
Cataract
The most common disease of the lens
Swelling/degeneration of lenticular fibersopacity

Lens response to injury:
Hydropic swelling of injured fibersfiber fragmentation & disintegration
Hyperplasia and fibrous metaplasia of lens epithelium
Posterior lens epithelial migration
When chronic (“hypermature”): shrinking and wrinkling of lens capsule and mineralization
What causes a cataract?
Radiation
Increased IOP (Glaucoma)
Endophthalmitis
Hereditary defect in lenticular metabolism
Diabetes mellitus (high glucose in aqueous)
Trauma
ANYTHING THAT DAMAGES THE LENTICULAR FIBERS!
What do you evaluate in a fundic exam?
Indications of retinal degeneration (& atrophy)
- Decreased vascularity
- Optic disc atrophy
- Changes in tapetal reflection
If you are loosing retina, the tapendum will become ______ reflective?
MORE
Causes of retinal degeneration & atrophy
Senile change
Inherited metabolic defect of photoreceptor cells
– Collectively known as PRAs (“progressive retinal atrophy”)
– SARD
Toxicity
Metabolic deficiencies – taurine, vitamin A
Increased IOP (glaucoma)
Retinal detachment

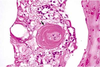
Retina from an adult cat with acquired blindness
Lost photoreceptor and outer nuclear & plexiform layers
Morphologic diagnosis: Retinal atrophy (& degeneration)
Cause:
Enrofloxacin toxicity
histo can’t tell you the etiology

Retina from a horse with increased IOP (glaucoma)
Loss of nerve fiber and ganglion cell layers, but excellent preservation of photoreceptors and outer nuclear layer
MDx: retinal atrophy
Causes of retinal detachment (separation)
Exudative
– Choroiditis, retinitis – Hemorrhage
– Neoplasm
• Tractional
– maturation of fibrin in vitreous (fibrous adhesions between ciliary bodies = “cyclitic membrane”)
Usually due to inflammation

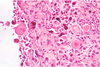
Retinal detachment due to effusion from the growth of metastatic lymphoma within the choroid and subretinal space

Retinal detachment (separation)

Consequence = retinal degeneration & atrophy
Separates between neural and pigmented layers
What is the most likely cause of the corneal opacity?

Glaucoma
Glaucoma
= ↑ IOP
• bad bad BAD
obstruction of the filtration angle
Primary Glaucoma
Cause = goniodysgenesis, a detectable malformation of the trabecular meshwork
Dogs – inherited, common
Other species – severely anomalous eyes

Goniodysgenesis, primary glaucoma
Secondary Glaucoma
Most common type
Causes = anything that obstructs the pupil or trabecular meshwork
– Exudate(endophthalmitis)
– Lens luxation
– Posteriorsynechia
– Peripheralanteriorsynechia
– Compression of the filtration angle
Peripheral anterior synechia- iris adheres to the cornea
Consequences of glaucoma…
Buphthalmos
Corneal edema +/- striae
Retinal degeneration & atrophy
Optic disc cupping
Optic nerve atrophy (because
of loss of ganglion cells)
Cataract
Lens luxation
Iris atrophy
pressure on optic nerve head causes this cuffing; can see on fundic

Dog with iris atrophy
(note, this can also be an old age degenerative change of the iris)

Dog with posterior luxated lens

calf with dermatophytosis

Dog with a chalazion
Blepharitis
Inflammation of the eyelids
Causes = same for skin in
general
• Exception:
– Chalazion – granulomatous inflammation directed against meibomian gland
– Stye – common name for bacterial infection of hair follicle or meibomian gland (usually Staph aureus)- more common in people
Conjunctivitis
Response to injury same as for other mucous membranes
Gross features
– Hyperemia
– Swelling/edema
– Discharge
– Chemosis – severe conjunctival edema
– Pigmentation – chronic lesions
Hyperemia alone does not necessarily indicate conjunctivitis

chemosis in a dog with conjunctivitis, cause unknown

Chemosis in a sheep with photosensitization
Causes of Conjunctivitis
Primary pathogens rare
Exceptions = cats
– Herpesvirus (FHV-1)
– Chlamydophiliafelis
– Mycoplasmafelis–normal resident or secondary pathogen
Histology – unlikely to establish cause!!

Feline conjunctivitis
Primary pathogens are only common in cats:
- herpes
- Chylamdophilia felis
- Mycoplasma
Nodular Granulomatous Episcleritis
Herding breeds esp. collies
Immune-mediated
pathogenesis
Junction of cornea and sclera, often bilaterally symmetrical
Histology = granulomatous keratoconjunctivitis
What would be some ddx for the gross lesion, and how would you establish a dx?

Nodular Granulomatous Episcleritis

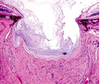
Corneal ulceration
Corneal response to injury
Edema
Epithelial regeneration
Neutrophil mediated stromal lysis
Neovasularization
Stromal fibrosis
If only eroded, epithelial regeneration is very rapid
If ulcerated, stromal repair must proceed epithelial regeneration
If chronic/persistent injury, cutaneous metaplasia may occur (combination of keratinization, epithelial hyperplasia, pigmentation, subepithelial fibrosis and vascularization)
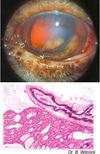
Case of Equine Corneal Ulcer
Owner declines treatment
A few days later the eye now
looks like below
What is the most likely cause?

Most likely cause- opportuntistic bacteria; when bacteria get into the stroma, neutrophils degranulate and also eat up corneal stroma
Etiology of Keratitis
Trauma
Bacterial:
– usually opportunistic, especially Pseudomonas aeruginosa
– primary pathogen = Moraxella bovis
Chlamydia/mycoplasma
Viruses: IBR, MCF, FHV-1
Fungi: Aspergillosis, Mucormycosis
Drying and desiccation: Keratoconjunctivitis sicca
Idiopathic:
– Chronic superficial keratitis (“Pannus”) in
German Shepherd
– Superficial indolent ulcers in Boxers
– Feline eosinophilic keratitis

Cow with “infectious keratoconjuncitivitis” (due to Moraxella bovis)
“Melting ulcers” (Keratomalacia)
Necrosis of corneal epithelium and stroma, usually due to innocent bystander injury from leukocytes
Due to rapidly progressing bacterial infection
In this case we culture a swab for bacteria and fungus – get Pseudomonas aeruginosa

Following a few days of aggressive antibiotic therapy
With a lesion similar to right, a descemetocele- desmes membrane is coming off
Emergency referral to specialist- EYE IS ABOUT TO RUPTURE
What went wrong?