Molavi Chapter 9 - Liver Flashcards
(40 cards)
Liver pathologies grouped by compartment they effect
-
Diseases of hepatocytes:
- Viral hepatitis, autoimmune hepatitis, nonalcoholic and alcoholic fatty liver disease, drug toxicity, metabolic/storage disease
-
Diseases of the biliary system:
- Autoimmune biliary disease (primary sclerosing cholangitis, primary biliary cirrhosis), obstruction, atresia, transplant rejection, GVHD, drug-induced injury
-
Diseases of the vasculature:
- Transplant rejection, GVHD, systemic vasculitides
- The portal tract represents a convergence of all these compartments, therefore inflammation of the portal tract can be found in all of these diseases
In the case of cirrhosis, you often cannot tell what. . .
. . . the original underlying pathology was
Therefore in almost every case of cirrhosis, “clinical correlation is required.”
The best clues you can get will be apparent disproportionate damage to the hepatocytes directly, biliary system, or vasculature.
In viral hepatitis and autoimmune hepatitis, the inflammatory infiltrate will be ___.
In a drug reaction, the inflammatory infiltrate will be ___.
In viral hepatitis and autoimmune hepatitis, the inflammatory infiltrate will be monocytic.
In a drug reaction, the inflammatory infiltrate will be eosinophilic.

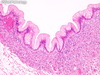
Interface activity
Inflammation (usually lymphocytic) occuring in the limiting plate and damging the hepatocytes along the boundary. Looks almost like portal inflammation spilling out into the hepatocytes.
Suggests hepatocellular injury of some sort.

Portal inflammation (mild in this case)
Inflammatory cells within the portal tract.
Suggests hepatocellular injury. In particular, if monocytic it suggests viral or autoimmune hepatitis, and if eosinophilic, a drug reaction. Plasma cells are also often seen in autoimmune hepatitis.

Lobular inflammation
Often accompanied by histiocyte necrosis, as seen here. Farther out from the portal tracts, unlike interface activity.
Spotty necrosis in these cases is characterized by little clusters of lymphocytes and/or macrophagers destroying individual hepatocytes in the lobules.
Do not count the lymphocytes in the sinuses, as these are physiologic!

Vacuolar degeneration of hepatocytes
aka “balloon cell change,” “ballooning,” “degeneration.”
One way in which hepatocytes become injured and die. The cell swells and the cytoplasm becomes feathery and pale-clear.

Acidophilic bodies in hepatocytes
A sign of hepatocyte death. These cells are similar to dyskeratotic cells in the skin: bright pink, shriveled up, with pyknotic nuclei.

Pure microvesicular steatosis
A special pattern of steatosis indicating mitochondrial injury, usually Reye’s syndrome
Looks like foamy cytoplasm within hepatocytes.

Mallory’s hyaline, or Mallory bodies
Irregular, worm-like, pink blobs of condensed cytoskeleton in the cytoplasm – especially within balloon cells. Indicative of cytoskeletal collapse.
They are associated with steatohepatitis and alcoholic disease in particular.

Megamitochondria
Markedly enlarged mitochondria that look like red cells trapped within the hepatocyte cytoplasm.
Seen in alcoholic liver disease and in nutritional deficiencies.

Alpha-1 antitrypsin deficiency
Note the circular blobs of amorphous hyaline material trapped within hepatocytes.

Bile stasis
Visible as yellow globs or chunks in hepatocyte cytoplasm bile cannaliculi, or less commonly in the bile duct lamina.
Still may be caused by extrahepatic obstruction, intrahepatic obstruction, or impaired excretion by hepatocytes.

Bile duct injury
Identified by lymphocytes in the bile duct epithelium and vacuolar degeneration or dropout of epithelial cells. There is often accompanying neutrophilic infiltrate and a notable pleomorphism of biliary ductule cells. Usually patchy, so multiple ducts must be examined. Indicates a biliary-centric disease such as PBC or transplant rejection. This particular image (front side) is taken from a patient with PBC.
The end stage is ductopeia (shown). Ductopenia is a diagnosis of absence and requires a conscious effort to look for bile ducts in each portal tract.


Vasculitis within the liver
This particular patient has polyarteritis nodosa.
In vasculitis, endothelial cells tend to round-up a bit and become more prominent.

Extramedullary hematopoiesis within the liver
At low power this may look like a pocket of lymphocytic infiltration, but on high power it becomes clear that these islands represent a nest of erythroid or myeloid precursors. Megakaryoctes may occasionally be seen.
The nests may be small, as seen here, or become quite larger.
This would be physiologic in a fetus or infant.


- Acute liver rejection
- A combination of:
- Mixed portal tract inflammation (lymphocytes, neutrophils, eosinophils)
- Venulitis
- Bile duct inflammation and injury
- Note how plump the endothelial cells are in this slide.
- Typically occurs within 5-30 days after transplant

Primary biliary cirrhosis
There is a strong mononuclear and granulomatous inflammation of the portal tract, with destruction of the bile ductule. Importantly, the small bile ducts are largely the target of destruction. These findings alone are really not entirely specific, but anti-mitochondrial antibody will be present in serum labs and confirm the diagnosis.

Primary sclerosing cholangitis
Ductular proliferation and cholestasis due to down-stream obstruction along with “onion-skin” concentric periductal fibrosis. The smaller ducts/ductules are usually spared – it is primarily the extrahepatic and large intrahepatic ducts that are involved from an inflammatory standpoint.
These findings are not entirely specific, but in the right clinical context with supportive cholangiogram and p-ANCA serology, the diagnosis becomes clear.

Autoimmune hepatitis
Chronic immune cells attacking the hepatoycytes themselves. Leads to chronic hepatitis with portal and lobular inflammation, interface activity, and prominent plasma cells. There will be several apoptotic figures at the interface of lymphocytes and hepatocytes.
Findings on this slide are not totally specific, but with the right clinical context and serology for ANA and anti-smooth muscle antibody (ASMA), the diagnosis can be made.

Focal nodular hyperplasia
An “island of cirrhosis” in a sea of normal liver. Not a clonal process, so there will be more than one cell type present.
There is no capsule, but there is often (not always) a central scar. The lesion is composed of hepatocyte nodules divided by bands of fibrosis and thick-walled vessels.

Hepatic adenoma
Benign clonal neoplasm. Occur mainly in noncirrhotic livers of adult women taking OCPs.
Circumscribed, partially encapsulated mass of uniform, bland-looking hepatocytes with no central veins or bile ducts. There are diffuse, prominent arterioles often termed “orphan arteries” or “naked arteries.” Cells may be pale due to steatosis or glycogen, or may be discolored with entrapped bile.
Divided into four groups based on molecular features: steatotic (HNF1a), inflammatory, beta-catenin-activated adenomas, and “none-of-the-above” adenomas.

Well-differentiated hepatocellular carcinoma
Low-grade malignant neoplasm of the hepatocytes. Can be very difficult to distinguish from an adenoma on histology, but often arises out of a background of cirrhosis and/or hepatitis viridae infection.
As with an adenoma, there are no bile ducts or central veins, and you may see intracellular bile. Nuclei may be large, hyperchromatic, and irregularly contoured. Pseudo-acinar formation is a mimic of gland formation which may suggest adenocarcinoma.
Reticulin stain shows a breakdown in architecture, with plates of 3 or more cells in thickness.

Poorly-differentiated hepatocellular carcinoma
High-grade malignant neoplasm of hepatocytes. May be very pleomorphic and hard to identify as hepatic. The presence of bile, if any, is a give-away. Immunostains are also helpful.