Molavi Chapter 4 - Complex Epithelia Flashcards
(24 cards)
Dyskeratosis
Abnormal, premature keratinization below the stratum granulosum.
In this case, note also the loss of cell-cell adhesions and the pyknotic nucleus – the cell indicated by the arrow is dying.

What’s going on in this skin biopsy?

Invasive squamous cell carcinoma
Note the irregular nests of keratinocytes and abberant keratinization in the stroma.
Eggs-nuclei vs boulder-nuclei
Reactive nuclei may enlarge, but should stay smooth and round to oval. Chromatin is grey-blue.
Dysplastic or immature nuclei appear to have too much chromatin for their nuclear membrane to contain and appear angulated with irregular borders. Chromatin is uniformly dense and dark, like charcoal.
Presence of a nucleolus
Generally suggestive of reactive changes rather than dysplasia
Squamous cells usually don’t take acquire large dark nucleoli until they become invasive.
N/C ratio in a squamous epithelium
Should decrease as you get closer to the surface.
If not, this is suggestive of dysplasia
Parakeratosis
Retention of small pyknotic nuclei in the surface keratin
Orthokeratosis
“Normal” anucleate keratin with a basket-weave pattern
Hyperkeratosis
Too much keratin, often accompanied by parakeratosis
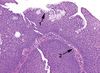
What’s going on in this skin biopsy?

This is a squamous papilloma
It has squamous epithelia overlying a branching fibrovascular core.
Pseudoepitheliomatous hyperplasia
Benign, reactive condtion that can mimic invasive squamous cell carcinoma.
It has a characteristic look “as though someone dragged the epithelium down into the stroma with a toothpick.” The individual nuclei should look reactive, not dysplastic, and there should be no deep keratinization.
May be provoked by a granular cell tumor.

Verrucous
Warty, exophytic growth pattern with prominent hyperkeratosis (and often parakeratosis)
“Church-spire” (pointy) or “cauliflower” (rounded) projections.

What’s going on in this cervical biopsy?

These are koilocytes.
Note the perinuclear halo with prominent, crinkled, dark nuclei. The nuclei get larger as you approach the surface, indicating dysplasia. Bunicleate cells are also present.
What’s going on in this cervical biopsy?

Normal glycogenated cervical epithelium. Don’t be fooled into thinking that these are koilocytes!
They have prominent perinuclear halos, but the nuclei at the surface are tiny and pyknotic. They are also more uniform than you may expect in HPV-mediated dysplasia.
Cervical cancer microstaging/grading (LSIL, CIN)

Condyloma vs LSIL
Shown in condyloma accuminata
They have the same changes as LSIL, but with a verrucous architecture.

Features of benign urothelium
- 5-7 cells thick
- Umbrella cell layer at the top
Flat vs papillary urothelial carcinomas
Flat: Progress from dysplasia to CIS to invasive carcinoma without making an exophytic lesion
Papillary: For urothelial lesions, may be graded as benign (papilloma), borderline (papillary urothelial neoplasm of low malignant potential), or cancer (low- and high-grade papillary urothelial carcinoma).
von Brunn’s nests
Invaginated folds of normal urothelium, which can simulate invasion

Features of urothelial cancer
- Increased number of cell layers (usually in papillary lesions)
- Loss of polarity (loss of parallel array of nuclei)
- Increased mitoses, above the basal layer
- Enlarged, irregular, or hyperchromatic nuclei
- Discohesive cells or partially denuded epithelium

Features of a laryngeal/oropharyngeal squamous lesion concerning for carcinoma
- Usually HPV driven, so benign lesions may have the typical low-grade HPV changes
- More concerning lesions have:
- High-grade dysplasia
- Significant atypia
- Warty architecture (church-spire keratosis)
- Severe keratinizing dysplasia (Note: In the orophaynx/larynx, unlike the cervix, mucosa tends to keratinize in dysplasia. These lesions may not be full thickness, but may still behave like carcinoma-in-situ)
Features of squamous dysplasia in the oropharynx/larynx
- Loss of cell polarity and maturation arrest
- Dyskeratosis, hyperkeratosis, acanthosis
- Increased mitoses or mitoses above the basal layer
- Cellular and nuclear pleoorphism (Note: in the oropharynx unlike other places, dysplastic nuclei tend to show prominent nuclei and nuclear membranes, more like an invasive carcinoma).
- Variable N/C ratio
- Not necessarily full-thickness involvement, even in severe dysplasia
What’s going on in this biopsy of an oral lesion?

Squamous dysplasia
Note: The parakaratosis present at the surface will appear as a white oral plaque clinically.
Note: Unlike in the cervix, prominent nucleoli may be a feature of dysplasia and do not necessarily suggest carcinoma.
Schneiderian papillomas
- Fancy name for “sinonasal” papillomas
- Lined with nonkeratinizing squamous or transitional epithelium, 5-30 cells thick
- May have ciliated or mucous lining
- Neutrophils are common
- May be fungiform (exophytic, septal) or inverted (inward growing)
- Should have only mild atypia, orderly cells, and few mitoses
- Features that suggest carcinoma instead: atypia, pleomorphism, increased mitotic activity, cells invading as nests and cords
Generally in the esophagus, squamous mucosa is not usually. . .
. . . a bad actor
More often it is glandular, seen in the setting of Barret’s esophagus.
Mild reactive changes are very common and correspond to reflux changes, and sometimes to infection.
If squamous dysplasia or carcinoma is found, it is typically in the upper esophagus in the setting of alcohol + smoke.


