Lower GI pathology Flashcards
What are the types of GI pathology?
Congenital
Acquired
Mechanical
Infection
Inflammation
Ischaemia
Tumour
What are the general symptoms of large bowel pathology?
Disturbance of normal function (diarrhoea, constipation)
Bleeding
Perforation/fistula formation
Obstruction
+/- Systemic illness
What are congenital GI disorders?
Atresia/stenosis
Duplication
Imperforate anus
What is Hirschsprung’s disease?
Absence of ganglion cells in myenteric plexus,
Distal colon fails to dilate
80% male
Constipation, abdominal distension, vomiting, ‘overflow’ diarrhoea
Associated with Down’s syndrome (2%)
RET proto-oncogene Cr10 + others
How do you diagnose Hirschsprungs disease?
clinical impression
biopsy of affected segment.
hypertrophied nerve fibers but no ganglia.
Treatment: resection of affected (constricted) segment. (frozen section)
What are mechanical bowel disorders?
Obstruction
Adhesions
Herniation
Extrinsic mass
Volvulus
Diverticular disease
What is a volvulus?
Complete twisting of a loop of bowel at mesenteric base, around vascular pedicle intestinal obstruction +/- infarction small bowel (infants) sigmoid colon (elderly)
What is the pathogenesis of diverticular disease?
High incidence in West
Low fibre diet
High intraluminal pressure
‘Weak points’ in wall of bowel
90% occur in left colon
What are the complications of diverticular disease?
Pain
Diverticulitis
Gross perforation
Fistula (bowel, bladder, vagina)
Obstruction
What are the inflammatory disorders of the large bowel?
Acute colitis
Infection (bacterial, viral, protozoal etc.)
Drug/toxin (esp.antibiotic)
Chemotherapy
Radiation
Chronic colitis
Crohn’s
Ulcerative colitis
TB
What are the infectious colitis’
Viral
Bacterial
Protozoal
Fungal
What are the effects of GI infection?
Secretory diarrhoea (toxin)
Exudative diarrhoea (invasion and mucosal damage)
Severe tissue damage + perforation
Systemic illness
(biopsy)
What is pseudomembranous colitis?
Antibiotic associated colitis
Acute colitis with pseudomembrane formation
Caused by protein exotoxins of C.difficile
How do you diagnose pseudomembranous colitis?
Histology: Characteristic microscopic features on biopsy
Laboratory: C. difficile toxin stool assay
Therapy: Metronidazole or Vancomycin
What is ischaemic bowel?
Acute or chronic
Most common vascular disorder of the intestinal tract
Usually occurs in segments in “watershed” zones, e.g. splenic flexure (SMA and IMA) and the rectosigmoid (IMA and internal iliac artery)
Mucosal, mural, transmural (perforation)
What is the aetiology of ischaemic colitis?
Arterial Occlusion: atheroma, thrombosis, embolism
Venous Occlusion: thrombus, hypercoagulable states
Small Vessel Disease: DM, cholesterol emboli, vasculitis
Low Flow States: CCF, haemorrhage, shock
Obstruction: hernia, intussusception, volvulus, adhesions
What is IBD?
Crohn’s disease or Ulcerative colitis
Diagnosis of exclusion
What is the aetiology of IBD?
?Genetic predisposition (familial aggregation, twin studies, HLA )
?Infection (Mycobacteria, Measles etc)
?Abnormal host immunoreactivity
->Inflammation
What are the clinical features of IBD?
Diarrhoea +/- blood
Fever
Abdominal pain
Acute abdomen
Anaemia
Weight loss
Extra-intestinal manifestations
Who gets Crohn’s?
Western populations
Occurs at any age but peak onset in teens/twenties
White 2-5x > non-white
Higher incidence in Jewish population
Smoking
Where is affected in Crohn’s?
Whole of GI tract can be affected (mouth to anus)
‘Skip lesions’
Transmural inflammation
Non-caseating granulomas
Sinus/fistula formation
‘Fat wrapping’
Thick ‘rubber-hose’ like wall
Narrow lumen
‘cobblestone mucosa’
Linear ulcers
Fissures
abscesses
What are the extra intestinal manifestations of Crohns?
Arthritis
Uveitis
Stomatitis/cheilitis
Skin lesions
Pyoderma gangrenosum
Erythema multiforme
Erythema nodosum
Who gets UC?
Slightly more common than Crohn’s
Whites > non-whites
Peak 20-25 years but can affect any age
What does UC cause?
Involves rectum and colon in contiguous fashion.
May see mild ‘backwash ileitis’ and appendiceal involvement but small bowel and proximal GI tract not affected.
Inflammation confined to mucosa
Bowel wall normal thickness
Shallow ulcers
What are the complications of UC?
Severe haemorrhage
Toxic megacolon
Adenocarcinoma (20-30 x risk)
What are the extra intestinal manifestations of UC?
Arthritis
Myositis
Uveitis/iritis
Erythema nodosum, pyoderma gangrenosum
Primary Sclerosing Cholangitis (5.5% in pancolitis)
What are the tumours of the colon and rectum?
- Non-neoplastic polyps
- Neoplastic epithelial lesions
- Adenoma
- Adenocarcinoma
- Stromal tumours
- Lipoma
- Sarcoma
- Carcinoid tumour
- Mesenchymal lesions
- Lymphoma
What are the polyps of the colon?
Polyps - Non-neoplastic
(Hyperplastic)
Inflammatory (“pseudo-polyps”)
Hamartomatous (juvenile, Peutz Jeghers)
Polyps - Neoplastic
Tubular adenoma
Tubulovillous adenoma
Villous adenoma
What are adenomas?
Excess epithelial proliferation + dysplasia
20-30% prevalence before age 40
40-50% prev. after age 60
Tubular
Villous
Tubulovillous
What increases cancer risk in a polyp?
Size of polyp (> 4 cm approx 45% have invasive malignancy)
Proportion of villous component
Degree of dysplastic change within polyp
What is the evidence of adenomas being a precursor to carcinomas?
High prevalence of adenoma = high prevalence of carcinoma
Colonic distribution similar
Peak incidence of adenomas 10 years before peak for Ca.
Residual adenoma near invasive Ca.
Risk proportional to no. of adenomas
Screening + removal of adenomas reduce Ca.
What are the symptoms of adenomas?
Usually none
Bleeding/anaemia
What are the familial syndromes linked to polyps?
(Peutz Jeghers)
Familial adenomatous polyposis
Gardner’s
Turcot
Hereditary non polyposis colon cancer
What is FAP?
Autosomal dominant - average onset is 25 years old
Adenomatous polyps, mostly colorectal
Minimum 100 polyps, average ~1,000 polyps
chromosome 5q21, APC tumour suppressor gene
virtually 100% will develop cancer within 10 to 15 years; 5% periampullary Ca
What is Gardeners syndrome?
Same clinical, pathological, and etiologic features as FAP, with high Ca risk
Distinctive extra-intestinal manifestations:
- Multiple osteomas of skull & mandible, epidermoid cysts, desmoid tumors
- Dental caries, unerrupted supernumery teeth
- Post-surgical mesenteric fibromatoses
What is HNPCC?
Uncommon autosomal dominant disease
3-5% of all colorectal cancers
1 of 4 DNA mismatch repair genes involved (mutation)
Numerous DNA replication errors (RER)
How does HNPCC present?
Onset of colorectal cancer at an early age
High frequency of carcinomas proximal to splenic flexure
Poorly differentiated and mucinous carcinoma more frequent
Multiple synchronous cancers
Presence of extracolonic cancers (endometrium, prostate, breast, stomach)
What are colorectal carcinomas?
98% are adenocarcinoma
Age: 60-79 years
If < 50yrs consider familial syndrome
Western population
What is the aetiology of colorectal carcinomas?
Diet (low fibre, high fat etc)
Lack of exercise
Obesity
Familial
Chronic Inflammatory bowel disease
What are the symptoms of colorectal carcinomas?
Bleeding
Change of bowel habit
Anaemia
Weight loss
Pain
Fistula
How do you grade/ stage colorectal carcinomas?
Grade = level of differentiation
Dukes’ staging
TNM (tumour, nodes, metastases)
How do you treat ischaemic bowel?
Resect
Do hyperplastic polyps cause cancer?
No!
What is this?

Hirschprungs disease
Similar to bowel obstruction but with Ileus findings due to aganglionosis
What is this?

Volvulus
Bowel rotation and dilation
What is this?

Diverticular disease (Barium enema)
Small outpouchings
What is this?

Pseudomembranous (C Diff) Colitis
Wet Cornflake look
What is this?

Diverticular disease
What is this?
Pseudomembranous colitis
What is this?

Ischaemic bowel
What does this show?

Crohn’s Disease- Skip lesions
What does this show?

Crohn’s Disease- Chronic inflammation and deep tissue damage
What is this?

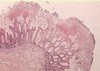
UC
Some continuous areas of damage with superficiality on microscopy.
What does this show?

Hyperplastic polyps
What is this?

Tubular adenoma
Many tube sections can be seen.
What is this?

Villous adenoma
What is this?

Familial Adenomatous Polyposis
What is this?

Apple core lesion (colorectal carcinoma)
What is this?

Colorectal carcinoma
What are the levels of Duke’s Staging?
How do they predict Survival?
A = confined to mucosa (5yrSurv=95%+)
B1 = through muscularis propria (5yrSurv=67%)
B2 = transmural invasion, no lymph nodes involved (5yrSurv=54%)
C1 = In muscularis propria with lymph node metastases (5yrSurv=43%)
C2=transmural invasion, lymph nodes involved (5yrSurv=23%)
D = distant metastases (5YrSurv<10%)



