Infectious diseases Flashcards
Immunosuppressed states
Chronic kidney disease
Diabetes
HIV
Hematologic malignancies
Chronic immunosuppression
Exam findings for mitral valve prolapse
Late systolic murmur over cardiac apex
Prolongs (occurs earlier in systole) with Valsalva (decreases left ventricular blood volume)
Bacterial endocarditis prophylaxis
- High-risk conditions
- Indicated procedures and appropriate coverage

Community Acquired bacterial meningitis in adults
Organisms
Streptococcus pneumoniae (70%)
Neisseria meningitidis (12%)
Group B Strep
Haemophilus influenzae
Agents
Ceftriaxone (everything)
Vancomycin (S. pneumo resistant to beta lactams)
Ampicillin (Listeria in immunocompromised patients or patients > 50)
Dexamethasone (S. pneumo)
Post-infectious complication of impetigo (group A strep)
Poststreptococcal glomerulonephritis
Post-infectious complication of group A strep pharyngitis
Rheumatic fever
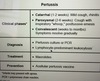
Measles (rubeola)
- Clinical presentation
- Diagnosis
- Prevention
- Treatment
- Complications


Erythema infectiosum (fifth disease)
Caused by Parvovirus B19
Pharyngoconjunctival fever
Caused by adenovirus
Pharyngitis
Non-prurulent conjunctivitis
Fever

Sandpaper-like, erythematous rash
Associated with scarlet fever
Caused by Streptococcus pyogenes (GAS)
Fever, toxicity, pharyngitis, rash, circumoral pallor and strawberry tongue.
Penicilline A is the drug of choice
Live attenuated vaccines
- Which ones
- Recommendations for HIV patients
Varicella
Zoster
Measles-Mumps-Rubella
Can be safely given to individuals with CD4 counts >200

Septic pulmonary emboli
In an IV drug user with infective endocarditis, likely due to staph aureus
Infective endocarditis in IV drug users
Tricuspid regurg
Holocystolic murmur increases with inspiration indicating tricuspid involvement


Miliary tuberculosis

Pneumocystis pneumonia
More common in HIV patients with CD4 counts <200
Subacute symptoms, diffuse infiltrates on chest X ray, increased A-a gradient
HIV in infancy
- Risk factors
- Clinical features
- Diagnosis
- Treatment

X-linked agammaglobulinema (XLA)
Low B cell concentrations
Recurrent bacteriopulmonary sinus infections
Absent lymphoid tissue
Low serum immunoglobulin levels
Ciliary dyskinesia
Recurrent ear, nasal, and sinus infections
Bacterial pneumonia
Adenosine deaminase deficiency
Causes severe combined immunodeficiency
Profound lymphopenia
Recurrent infections
Failure to thrive
Chronic granulomatous disease
Impaired phagocytosis
Recurrent, severe infections due to catalase-positive organisms (Staph aureus, Serratia) and fungal organisms (Aspergillus)
Toxoplasma encephalitis
- Clinical
- Diagnostic
- Therapeutic

Neurocysticercosis
Treatment
Associated with pork consumption or travel to endemic areas (Central or South America)
Causes seizures
Albendazole
Cryptococcal meningitis
Treatment
Fever, malaise, ring-enhancing lesions on MRI
Amphotericin B and flucytosine
Mycobacterium avium complex (MAC)
Treatment
Clarithromycin and ethambutol