2.9 - 2.10 Cancer Flashcards
What is the difference between normal cells to cancer cells?

What sort of changes is cancer caused by?
- Cancer is caused by genetic changes that affect gene expression or function.
- These can be caused by:
- Mutations (due to DNA damage)
- chromosomal abnormalities such as translocations
- Introduction of genes by viruses
What is cancer defined as?
A disease featuring abnormal and improperly controlled cell division resulting in invasive growths, or tumours, that may spread throughout the body
What is carcinoma?
Cancers of epithelial cells
Account for about 80% of human cancers (lung, breast, bowel, prostate, etc)
What is sarcoma?
Cancers of connective tissue
Bone, cartilage, fat, muscle vascular tissues
What is melanoma?
Cancers of melanocytes (pigment producing cells in the skin)
What are leukaemias?
Cancer of white blood cells
What are lymphomas?
Cancers of the lymphatic system
What are cancers of the cells of the nervous system (neurons and glia) known as?
Retinoblastoma, glioblastoma, medulloblastoma, neuroblastoma
What is the relationship between age and cancer?
Age increases cancer incidence
What is the relationship between mutagens and cancer incidence?
Exposure to mutagens increases cancer incidence

What is a tumor?
Abnormal growth of tissue
What is tumorigenesis?
Formation of tumors
What are benign tumors?
- Moles for example
- They generally stop growing or grow slowly
- Do not spread to other parts of the body
- Can still cause problems (e.g brain tumor) and progress to malignancy
What are malignant tumours?
- They can proliferate endlessly
- Can invade healthy tissues and spread to other parts of the body to create secondary tumors (metastasise)
- They can draw in blood vessels (angiogenesis) to get nutrients and oxygen for more growth
- Can interfere with body functions
What are the five hallmarks of cancer?

Which of the hallmarks of cancer are responsible for tumorigenesis?

Which of the hallmarks of cancer are responsible for metastasis?

How does cancer progression occur by accumulated mutations?
- The transition from a normal cell to cancerous involves successive mutations
- First mutation could give a slight proliferative advantage to the cell
- Second mutation greatly increase proliferation and start to affect the tissue structure
- Third mutation allow cells to break into their surrounding environment and metastasise

What are the two pathways to tumorigenesis?
In a normal tissue, the birth and apoptosis (i.e. death) of cells is balanced. If this balance is disturbed by INCREASED cell birth, or DECREASED apoptosis then tumors can form.

What is an oncogene?
A gene that, when mutation or expressed at high levels, helps turn a normal cell into a CANCER cell (this process is called transformation)
What is a proto-oncogene?
The normal form of the gene
What is a tumor supressor gene (TSG)?
A gene that acts to prevent a normal cell from turning into a cancer cell (also known as anti-oncogenes)
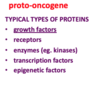
Typically what sort of proteins do proto-oncogenes?