Week 4 - A - Multiple Sclerosis - Symptoms, Ix, Diagnosis, Tx Flashcards
What is multiple sclerosis?
Multiple sclerosis is an autoimmune inflammatory demyelinating disorder of the CNS
What is the inflammatory process of multiple sclerosis caused by?
T cells
Apart from demyelination, the other sign of the disease is inflammation. Fitting with an immunological explanation, the inflammatory process is caused by T cells, a kind of lymphocyte that plays an important role in the body’s defenses. T cells gain entry into the brain via disruptions in the blood–brain barrier. The T cells recognize myelin as foreign and attack it, explaining why these cells are also called “autoreactive lymphocytes”
What gender is multiple sclerosis more common in? WHat age group does it usually present in?
MS is more common infemales 3:1 and initial diagnosis is usually at 20-30 years of age
Is MS genetic or multifactorial? What is a factor in MS?
MS is a multifactorial disease
The more northern you live the more likely someone is to get multiple sclerosis - vit D deficiency
WHat genetic haplotype is linked to multiple sclerosis?
HLA DRB1 is linked to multiple sclerosis
What are the different types of multiple sclerosis?
Relapse Remitting - most common - more than 8 out of 10 with condition have this
Primary progressive - 1 in 10 with condition have this
Secondary progressive
Progressive relapsing
Describe the different types of multiple sclerosis?
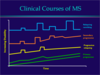
Relapsing remitting - periods of remission with steadily worsening relapses occuring
Primary progressive - steady increase in disability
Secondary progressive - Begins as relapsing remitting then a progressive decrease in disability
Progressive relapsing - steady decline superimposed with relapses
What percentage of patients will go on to develop secondary progressive MS after having relapsing remitting?
Around half of patients with relapsing remitting MS will have developed secondary progressive by 15-20 years after diagnosis
What are the clinical features of MS?
Optic neuritis
Cerebellar and brainstem features
Lower urinary tract dysfunction
Sensory symtpoms Pyramidal
dysfunction (and cognitive impairment)
Trigeminal nerualgia
How does pyramidal dysfunction present in multiple sclerosis?
Hyperreflexia
Increased tone in the limbs
Hyperflexion in the upper limbs
Hyperextension in the lower limbs
Spasciticity
Also weakness in the limbs (paraparesis) (partial loss of voluntary motor function)
In pyramdial dysfunction, what tract is affected? Is it the upper or lower motor neurons? (think how they would correlate to the signs and sympotms)
It is the corticospinal (pyramidal) tract which is affected It is the upper motor neurons affect (as MS affects the CNS, would not affect lower motor neurons) Thereofre the hypereflexia, spasciticty, increased tone, flexion in upper limbs, extension in lower limbs
What is the sign in the foot indicative of an upper motor neuron lesion that can be seen in pyramidal dysfunction due to MS? (MS will causes plaques along the corticospinal tract)
This would be Babinski’s sign - scrape with a blunt edge along outside of the foot and into the middle of the foot Normal - toes curl Abnormal - Toes fan outwards - indicates UMN lesions
When is the fanning of toes normal in response to a blunt instrument?
This is physiological in a neonate as the corticospina tract is not fully myelinated as of yet
How does optic neuritis present?
Pain behind the eye when moving the eye Usually a central loss of vision known as a central scotoma Relevant afferent pupillary defect
What is the central loss of vision in optic neuritis known as?
This is a central scotoma
Where are the cells important for colour vision located? What are these cells?
These cells are called cones - they are photoreceptors for colour located in the back of the retina The cetral fovea is populated only by cones and no rods which are used in dim light (black and white vision) C for colour
What test can be carried out to detect a relevant afferent pupillary defect as seen with optic neuritis?
A swinging light test
What is seen in the swinging light test when looking for a relevant afferent pupillary defect? Where is the lesion usually present to cause of RAPD?
The patient’s pupils constrict less (therefore appearing to dilate) when a bright light is swung from the unaffected eye to the affected eye. The affected eye still senses the light and produces pupillary sphincter constriction to some degree, albeit reduced - efferent response is normal The defect would be in the optic nerve
What is a relative afferent pupillary defect sometimes known as?
Relative afferent pupillary defect (RAPD) or Marcus Gunn pupil is a medical sign observed during the swinging-flashlight test[1] whereupon the patient’s pupils constrict less (therefore appearing to dilate) when a bright light is swung from the unaffected eye to the affected eye. The affected eye still senses the light and produces pupillary sphincter constriction to some degree, albeit reduced.
What are some of the sensory symptoms seen in a patient with Multiple sclerosis? Why is there pain in mutliple sclerosis?
Loss of sense to vibration and proprioception Pain Paraesthesia IF a nerve is irritated by a plaque compressing it, this can cause pain
stabbing or burning sensations down the side of the face, usually on one side only is common in mutliple sclerosis What is this known as? What test can be performed that will be psootiive in testing proprioception loss in MS?
This is trigeminal neuralgia Patient will be rhomberg’s test positive as they have a proprioceptive loss
What drug can be used to treat trigeminal neuralgia? (it can be used for neuropathic pain in general)
Carbamezapine
What is seen in cerebellar dysfunction? (another clinical sign of multiple sclerosis) What is the cerebellum important in?
Disdiadokinesis Ataxia - slurred speech, ataxis gait (balance), lack of coordination Nystagmus Iintention tremor Staccato/slurred speech Hypotonia Cerebellum plays an important role in co-ordination

What are the type of reflexes seen in cerebellar disorders known as?
Pendular reflexes



