Respiratory - First Aid Flashcards
Lung Development
- occurs in five stages
- initial development includes development of lung bud from distal end of respiratory diverticulum during week 4
-
Every Pulmonologist Can See Alveoli.
- Embryonic (weeks 4–7)
- Pseudoglandular (weeks 5–17)
- Canalicular (weeks 16–25)
- Saccular (week 26–birth)
- Alveolar (week 36–8 years)

Lung Development:
Embryonic (weeks 4–7)
- lung bud → trachea → bronchial bud → mainstem bronchi → secondary (lobar) bronchi → tertiary (segmental) bronchi
- errors at this stage can lead to tracheoesophageal fistula

Lung Development:
Pseudoglandular (weeks 5–17)
- endodermal tubules → terminal bronchioles
- surrounded by modest capillary network
- respiration impossible, incompatible with life

Lung Development:
Canalicular (weeks 16–25)
- terminal bronchioles → respiratory bronchioles → alveolar ducts
- surrounded by prominent capillary networ
- airways increase in diameter
- respiration capable at 25 weeks
- pneumocytes develop starting at 20 weeks

Lung Development:
Saccular (week 26–birth)
- alveolar ducts → terminal sacs
- terminal sacs separated by 1° septae

Lung Development:
Alveolar (week 36–8 years)
- terminal sacs → adult alveoli (due to 2° septation)
- in utero, “breathing” occurs via aspiration and expulsion of amniotic fluid → ↑ vascular resistance through gestation
- at birth, fluid gets replaced with air → ↓ in pulmonary vascular resistance
- At birth: 20–70 million alveoli
- By 8 years: 300–400 million alveoli

Congenital Lung Malformations:
- poorly developed bronchial tree with abnormal histology
- associated with congenital diaphragmatic hernia (usually left-sided) and bilateral renal agenesis (Potter sequence)
Pulmonary Hypoplasia
Congenital Lung Malformations:
- caused by abnormal budding of the foregut and dilation of terminal or large bronchi
- discrete, round, sharply defined, fluid-filled densities on CXR (air-filled if infected)
- generally asymptomatic but can drain poorly, causing airway compression and/or recurrent respiratory infections
Bronchogenic Cysts
Respiratory Embryology:
- nonciliated
- low columnar/cuboidal with secretory granules
- located in bronchioles
- degrade toxins
- secrete component of surfactant
- act as reserve cells
Club Cells
Alveoli
- Alveoli have ↑ tendency to collapse on expiration as radius ↓ (law of Laplace).
- Pulmonary surfactant is a complex mix of lecithins, the most important of which is dipalmitoylphosphatidylcholine (DPPC).
- Surfactant synthesis begins around week 20 of gestation, but mature levels are not achieved until around week 35.
- Corticosteroids important for fetus surfactant production and lung development.

Alveolar Cell Types:
- 97% of alveolar surfaces
- line the alveoli
- squamous
- thin for optimal gas diffusion
Type I Pneumocytes
Alveolar Cell Types:
- secrete surfactant from lamellar bodies → ↓ alveolar surface tension, prevents alveolar collapse, ↓ lung recoil, and ↑ compliance
- cuboidal and clustered
- also serve as precursors to type I cells and other type II cells
- proliferate during lung damage
Type II Pneumocytes
Alveolar Cell Types:
- phagocytose foreign materials
- release cytokines and alveolar proteases
- hemosiderin-laden macrophages may be seen in pulmonary hemorrhage
Alveolar Macrophages
Neonatal Respiratory Distress Syndrome
- surfactant deficiency → ↑ surface tension → alveolar collapse (“ground-glass” appearance of lung fields)
- Risk Factors:
- prematurity
- maternal diabetes (due to ↑ fetal insulin)
- C-section delivery (↓ release of fetal glucocorticoids; less stressful than vaginal delivery)
- Complications:
- PDA
- necrotizing enterocolitis
- Treatment:
- maternal steroids before birth
- exogenous surfactant for infant
- Therapeutic supplemental O2 can result in (RIB):
- Retinopathy of prematurity
- Intraventricular hemorrhage
- Bronchopulmonary dysplasia
- Screening Tests:
- lecithinsphingomyelin (L/S) ratio in amniotic fluid(≥ 2 is healthy; < 1.5 predictive of NRDS)
- foam stability index
- surfactant-albumin ratio
- persistently low O2 tension → risk of PDA
Respiratory Tree

Respiratory Tree:
Conducting Zone
- large airways consist of nose, pharynx, larynx, trachea, and bronchi
- small airways consist of bronchioles that further divide into terminal bronchioles (large numbers in parallel → least airway resistance)
- warms, humidifies, and filters air but does not participate in gas exchange → “anatomic dead space”
- cartilage and goblet cells extend to the end of bronchi
- pseudostratified ciliated columnar cells primarily make up epithelium of bronchus and extend to beginning of terminal bronchioles, then transition to cuboidal cells
- clear mucus and debris from lungs (mucociliary escalator)
- airway smooth muscle cells extend to end of terminal bronchioles (sparse beyond this point)

Respiratory Tree:
Respiratory Zone
- lung parenchyma
- consists of respiratory bronchioles, alveolar ducts, and alveoli
- participates in gas exchange
- mostly cuboidal cells in respiratory bronchioles, then simple squamous cells up to alveoli
- cilia terminate in respiratory bronchioles
- alveolar macrophages clear debris and participate in immune response

Lung Anatomy
- Right lung has 3 lobes.
- Left has Less Lobes (2) and Lingula (homolog of right middle lobe).
- Instead of a middle lobe, left lung has a space occupied by the heart.
- Relation of the pulmonary artery to the bronchus at each lung hilum is described by RALS:
- Right Anterior
- Left Superior
- Carina is posterior to ascending aorta and anteromedial to descending aorta.
- Right lung is a more common site for inhaled foreign bodies because right main stem bronchus is wider, more vertical, and shorter than the left.
- Aspiration:
- while supine—usually enters right lower lobe
- while lying on right side—usually enters right upper lobe
- while upright—usually enters right lower lobe

Diaphragm Structures
- Structures perforating diaphragm:
- T8: IVC, right phrenic nerve
- T10: esophagus, vagus (CN 10; 2 trunks)
- T12: aorta (red), thoracic duct (white), azygos vein (blue) (“At T-1-2 it’s the red, white, and blue”)
- I (IVC) ate (8) ten (10) eggs (esophagus) at (aorta) twelve (12).
- Diaphragm is innervated by C3, 4, and 5 (phrenic nerve).
- C3, 4, 5 keeps the diaphragm alive.
- Pain from diaphragm irritation (eg. air, blood, or pus in peritoneal cavity) can be referred to shoulder (C5) and trapezius ridge (C3, 4).
- Number of Letters = T Level:
- T8: vena cava
- T10: “oesophagus”
- T12: aortic hiatus
- Other bifurcations:
- The common carotid bifourcates at C4.
- The trachea bifourcates at T4.
- The abdominal aorta bifourcates at L4.

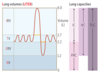
Lung Volumes
A capacity is a sum of ≥ 2 physiologic volumes.
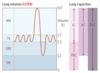
Lung Volumes:
air that can still be breathed in after normal inspiration
Inspiratory Reserve Volume
Lung Volumes:
- air that moves into lung with each quiet inspiration
- ttypically 500 mL
Tidal Volume
Lung Volumes:
air that can still be breathed out after normal expiration
Expiratory Reserve Volume
Lung Volumes:
- air in lung after maximal expiration
- _____ and any lung capacity that includes _____ cannot be measured by spirometry
Residual Volume
Lung Volumes:
- IRV + TV
- air that can be breathed in after normal exhalation
Inspiratory Capacity

Lung Volumes:
- RV + ERV
- volume of gas in lungs after normal expiration
Functional Residual Capacity
Lung Volumes:
- TV + IRV + ERV
- maximum volume of gas that can be expired after a maximal inspiration
Vital Capacity
Lung Volumes:
- IRV + TV + ERV + RV
- volume of gas present in lungs after a maximal inspiration
Total Lung Capacity
Determination of Physiologic Dead Space
- VD = physiologic dead space
- anatomic dead space of conducting airways plus alveolar dead space
- apex of healthy lung is largest contributor of alveolar dead space
- volume of inspired air that does not take part in gas exchange
- VT = tidal volume
- Paco2 = arterial Pco2
- Peco2 = expired air Pco2.
- Taco, Paco, Peco, Paco (refers to order of variables in equation)
- Physiologic Dead Space
- approximately equivalent to anatomic dead space in normal lungs
- may be greater than anatomic dead space in lung diseases with V˙/Q˙ defects

Ventilation:
- total volume of gas entering lungs per minute
- VE = VT × RR
Minute Ventilation
Normal Values:
- Respiratory rate (RR) = 12–20 breaths/min
- VT = 500 mL/breath
- VD = 150 mL/breath
Ventilation:
- volume of gas that reaches alveoli each minute
- VA = (VT − VD) × RR
Alveolar Ventilation
Normal Values:
- Respiratory rate (RR) = 12–20 breaths/min
- VT = 500 mL/breath
- VD = 150 mL/breath
Lung and Chest Wall
- Elastic Recoil
- tendency for lungs to collapse inward and chest wall to spring outward
- At FRC, inward pull of lung is balanced by outward pull of chest wall, and system pressure is atmospheric.
- At FRC, airway and alveolar pressures equal atmospheric pressure (called zero), and intrapleural pressure is negative (prevents atelectasis).
- The inward pull of the lung is balanced by the outward pull of the chest wall.
- System pressure is atmospheric.
- PVR is at a minimum.
- Compliance
- change in lung volume for a change in pressure
- expressed as ΔV/ΔP and is inversely proportional to wall stiffness
- hig compliance = lung easier to fill (emphysema, normal aging)
- lower compliance = lung harder to fill (pulmonary fibrosis, pneumonia, NRDS, pulmonary edema)
- surfactant increases compliance
- Compliant lungs comply (cooperate) and fill easily with air.
- Hysteresis
- lung inflation curve follows a different curve than the lung deflation curve due to need to overcome surface tension forces in inflation

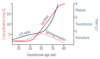
Respiratory System Changes in the Elderly
- ↑ lung compliance (loss of elastic recoil)
- ↓ chest wall compliance (↑ chest wall stiffness)
- ↑ RV
- ↓ FVC and FEV1
- Normal TLC
- ↑ ventilation/perfusion mismatch
- ↑ A-a gradient
- ↓ respiratory muscle strength
Hemoglobin
- Hemoglobin (Hb) is composed of 4 polypeptide subunits (2α and 2β) and exists in 2 forms:
- Deoxygenated form has low affinity for O2, thus promoting release/unloading of O2.
- Oxygenated form has high affinity for O2 (300×). Hb exhibits positive cooperativity and negative allostery.
- ↑ Cl−, H+, CO2, 2,3-BPG, and temperature favor deoxygenated form over oxygenated form (shifts dissociation curve right → ↑ O2 unloading).
- Fetal Hb (2α and 2γ subunits) has a higher affinity for O2 than adult Hb, driving diffusion of oxygen across the placenta from mother to fetus. ↑ O2 affinity results from ↓ affinity of
- HbF for 2,3-BPG.
- Hemoglobin acts as buffer for H+ ions.
- Myoglobin is composed of a single polypeptide chain associated with one heme moiety. Higher affinity for oxygen than Hb.

Hemoglobin Modifications
Lead to tissue hypoxia from ↓ O2 saturation and ↓ O2 content.
Hemoglobin Modifications:
Methemoglobin
- Oxidized form of Hb (ferric, Fe3+), does not bind O2 as readily as Fe2+, but has ↑ affinity for cyanide. Fe<strong>2</strong>+ binds O2.
- Iron in Hb is normally in a reduced state (ferrous, Fe<strong>2</strong>+; “just the 2 of us”).
- Methemoglobinemia may present with cyanosis and chocolate-colored blood.
- Methemoglobinemia can be treated with methylene blue and vitamin C.
- Nitrites (eg. from dietary intake or polluted/high altitude water sources) and benzocaine cause poisoning by oxidizing Fe2+ to Fe3+.
Hemoglobin Modifications:
Carboxyhemoglobin
- Form of Hb bound to CO in place of O2. Causes ↓ oxygen-binding capacity with left shift in oxygen-hemoglobin dissociation curve. ↓ O2 unloading in tissues.
- CO binds competitively to Hb and with 200× greater affinity than O2.
- CO poisoning can present with headaches, dizziness, and cherry red skin. May be caused by fires, car exhaust, or gas heaters. Treat with 100% O2 and hyperbaric O2.
Cyanide Poisoning
- Usually due to inhalation injury (eg. fires).
- Inhibits aerobic metabolism via complex IV inhibition → hypoxia unresponsive to supplemental O2 and ↑ anaerobic metabolism.
- Findings:
- almond breath odor
- pink skin
- cyanosis
- Rapidly fatal if untreated.
- Treat with induced methemoglobinemia: first give nitrites (oxidize hemoglobin to methemoglobin, which can trap cyanide as cyanmethemoglobin), then thiosulfates (convert cyanide to thiocyanate, which is renally excreted).
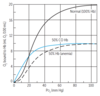
Oxygen-Hemoglobin Dissociation Curve
- Sigmoidal shape due to positive cooperativity (ie. tetrameric Hb molecule can bind 4 O2 molecules and has higher affinity for each subsequent O2 molecule bound).
- Myoglobin is monomeric and thus does not show positive cooperativity; curve lacks sigmoidal appearance.
- Shifting the curve to the right → ↓ Hb affinity for O2 (facilitates unloading of O2 to tissue) → ↑ P50 (higher Po2 required to maintain 50% saturation).
- Shifting the curve to the left → ↓ O2 unloading → renal hypoxia → ↑ EPO synthesis → compensatory erythrocytosis.
- Fetal Hb has higher affinity for O2 than adult Hb (due to low affinity for 2,3-BPG), so its dissociation curve is shifted left.

Oxygen Content of Blood
- O2 content = (1.34 × Hb × Sao2) + (0.003 × Pao2)
- Hb = hemoglobin level
- Sao2 = arterial O2 saturation
- Pao2 = partial pressure of O2 in arterial blood
- Normally 1 g Hb can bind 1.34 mL O2; normal Hb amount in blood is 15 g/dL.
- O2 binding capacity ≈ 20.1 mL O2/dL of blood.
- With ↓ Hb there is ↓ O2 content of arterial blood, but no change in O2 saturation and Pao2.
- O2 delivery to tissues = cardiac output × O2 content of blood.

Pulmonary Circulation
- Normally a low-resistance, high-compliance system. Po2 and Pco2 exert opposite effects on pulmonary and systemic circulation. A ↓ in Pao2 causes a hypoxic vasoconstriction that shifts blood away from poorly ventilated regions of lung to well-ventilated regions of lung.
- Perfusion Limited
- O2 (normal health), CO2, N2O
- gas equilibrates early along the length of the capillary
- diffusion can be ↑ only if blood flow ↑
- Diffusion Limited
- O2 (emphysema, fibrosis, exercise), CO
- gas does not equilibrate by the time blood reaches the end of the capillary
- A consequence of pulmonary hypertension is cor pulmonale and subsequent right ventricular failure.

Pulmonary Vascular Resistance
- Ppulm artery = pressure in pulmonary artery
- PL atrium ≈ pulmonary capillary wedge pressure
- Q = cardiac output (flow)
- R = resistance
- η = viscosity of blood
- l = vessel length
- r = vessel radius

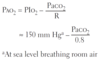
Alveolar Gas Equation
- Pao2 = alveolar Po2 (mmHg)
- PIo2 = Po2 in inspired air (mmHg)
- Paco2 = arterial Pco2 (mmHg)
- R = respiratory quotient = CO2 produced/O2 consumed
- A-a gradient = Pao2 – Pao2
- Normal Range = 10–15 mm Hg
- ↑ A-a gradient may occur in hypoxemia.
- causes include shunting, V˙/Q˙ mismatch, and fibrosis (impairs diffusion)
Oxygen Deprivation:
- ↓ cardiac output
- hypoxemia
- anemia
- CO poisoning
Hypoxia (↓ O2 delivery to tissue)
Oxygen Deprivation:
- Normal A-a gradient
- high altitude
- hypoventilation (eg. opioid use)
- ↑ A-a gradient
- V˙/Q˙ mismatch
- diffusion limitation (eg. fibrosis)
- right-to-left shunt
Hypoxemia (↓ Pao2)
Oxygen Deprivation:
- impeded arterial flow
- ↓ venous drainage
Ischemia (loss of blood flow)
Ventilation/Perfusion Mismatch
- Ideally, ventilation is matched to perfusion (ie. V˙/Q˙ = 1) for adequate gas exchange.
- Lung zones:
- V˙/Q˙ at apex of lung = 3 (wasted ventilation)
- V˙/Q˙ at base of lung = 0.6 (wasted perfusion)
- Both ventilation and perfusion are greater at the base of the lung than at the apex of the lung.
- With exercise (↑ cardiac output), there is vasodilation of apical capillaries → V˙/Q˙ ratio approaches 1.
- Certain organisms that thrive in high O2 (eg. TB) flourish in the apex.
- V˙/Q˙ = 0 = “oirway” obstruction (shunt). In shunt, 100% O2 does not improve Pao2 (eg. foreign body aspiration).
- V˙/Q˙ = ∞ = blood flow obstruction (physiologic dead space). Assuming < 100% dead space, 100% O2 improves Pao2 (eg. pulmonary embolus).

Carbon Dioxide Transport
- CO2 is transported from tissues to lungs in 3 forms:
① HCO3− (70%)
② Carbaminohemoglobin or HbCO2 (21–25%)
- CO2 bound to Hb at N-terminus of globin (not heme)
- CO2 favors deoxygenated form (O2 unloaded)
③ Dissolved CO2 (5–9%)
- In lungs, oxygenation of Hb promotes dissociation of H+ from Hb. This shifts equilibrium toward CO2 formation; therefore, CO2 is released from RBCs (Haldane effect).
- In peripheral tissue, ↑ H+ from tissue metabolism shifts curve to right, unloading O2 (Bohr effect).
- Majority of blood CO2 is carried as HCO3− in the plasma.

Response to High Altitude
- ↓ atmospheric oxygen (PO2) → ↓ Pao2 → ↑ ventilation → ↓ Paco2 → respiratory alkalosis → altitude sickness
- chronic ↑ in ventilation
- ↑ erythropoietin → ↑ Hct and Hb (due to chronic hypoxia)
- ↑ 2,3-BPG (binds to Hb causing left shift so that Hb releases more O2)
- cellular changes (↑ mitochondria)
- ↑ renal excretion of HCO3− to compensate for respiratory alkalosis (can augment with acetazolamide)
- chronic hypoxic pulmonary vasoconstriction results in pulmonary hypertension and RVH
Response to Exercise
- ↑ CO2 production
- ↑ O2 consumption
- ↑ ventilation rate to meet O2 demand
- V˙/Q˙ ratio from apex to base becomes more uniform
- ↑ pulmonary blood flow due to ↑ cardiac output
- ↓ pH during strenuous exercise (2° to lactic acidosis)
- no change in Pao2 and Paco2, but ↑ in venous CO2 content and ↓ in venous O2 content
Respiratory Pathology:
- obstruction of sinus drainage into nasal cavity → inflammation and pain over affected area
- typically affects maxillary sinuses, which drain against gravity due to ostia located superomedially
- most common acute cause is viral URI
- may lead to superimposed bacterial infection, most commonly S. pneumoniae, H. influenzae, and M. catarrhalis
- infections in sphenoid or ethmoid sinuses may extend to cavernous sinus and cause complications (eg. cavernous sinus syndrome)
Rhinosinusitis
Respiratory Pathology:
- nose bleed
- most commonly occurs in anterior segment of nostril (Kiesselbach plexus)
- life-threatening hemorrhages occur in posterior segment (sphenopalatine artery, a branch of maxillary artery)
- common causes include foreign body, trauma, allergic rhinitis, and nasal angiofibromas (common in adolescent males)
Epistaxis
Kiesselbach drives his Lexus with his LEGS:
- superior Labial artery
- anterior and posterior Ethmoidal arteries
- Greater palatine artery
- Sphenopalatine artery
Respiratory Pathology:
- mostly squamous cell carcinoma
- risk factors include tobacco, alcohol, HPV-16 (oropharyngeal), aand EBV (nasopharyngeal)
- Field Cancerization
- carcinogen damages wide mucosal area → multiple tumors that develop independently after exposure
Head and Neck Cancer
Deep Venous Thrombosis
- blood clot within a deep vein → swelling, redness, warmth, pain
- Predisposed by Virchow triad (SHE):
- Stasis (eg. post-op, long drive/flight)
- Hypercoagulability (eg. defect in coagulation cascade proteins, such as factor V Leiden; oral contraceptive use)
- Endothelial damage (exposed collagen triggers clotting cascade)
- d-dimer lab test used clinically to rule out DVT (high sensitivity, low specificity)
- Most pulmonary emboli arise from proximal deep veins of the lower extremities.
- Use unfractionated heparin or low-molecular-weight heparins (eg, enoxaparin) for prophylaxis and acute management.
- Use oral anticoagulants (eg. warfarin, rivaroxaban) for treatment (long-term prevention).
- Imaging test of choice is compression ultrasound with Doppler.
Pulmonary Emboli
- V˙/Q˙ mismatch, hypoxemia, and respiratory alkalosis
- sudden-onset dyspnea, pleuritic chest pain, tachypnea, and tachycardia
- Large emboli or saddle embolus may cause sudden death due to electromechanical dissociation.
- Lines of Zahn are interdigitating areas of pink (platelets, fibrin) and red (RBCs) found only in thrombi formed before death; help distinguish pre- and postmortem thrombi.
- Types (FAT BAT):
- Fat
- Air
- Thrombus
- Bacteria
- Amniotic fluid
- Tumor
- Fat Emboli
- associated with long bone fractures and liposuction
- classic triad of hypoxemia
- neurologic abnormalities
- petechial rash
- Air Emboli
- nitrogen bubbles precipitate in ascending divers (caisson disease/decompression sickness)
- treat with hyperbaric O2
- can be iatrogenic 2° to invasive procedures (eg. central line placement)
- Amniotic Fluid Emboli
- can lead to DIC
- especially postpartum
- CT pulmonary angiography is imaging test of choice for PE (look for filling defects).
- May have S1Q3T3 abnormality on ECG.
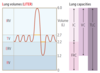
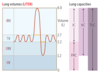
Flow-Volume Loops

Obstructive Lung Diseases
- obstruction of air flow → air trapping in lungs
- airways close prematurely at high lung volumes → ↑ FRC, ↑ RV, ↑ TLC
- PFTs: ↓↓ FEV1, ↓ FVC → ↓ FEV1/FVC ratio (hallmark),
- V˙/Q˙ mismatch
- Chronic, hypoxic pulmonary vasoconstriction can lead to cor pulmonale.
- Chronic obstructive pulmonary disease (COPD) includes chronic bronchitis and emphysema.
- “FRiCkin’ RV needs some increased TLC, but it’s hard with COPD!”
Obstructive Lung Diseases:
- Findings:
- wheezing, crackles, cyanosis (hypoxemia due to shunting), dyspnea, CO2 retention, 2° polycythemia
- hypertrophy and hyperplasia of mucus-secreting glands in bronchi → Reid index (thickness of mucosal gland layer to thickness of wall between epithelium and cartilage) > 50%
- DLCO usually normal.
- Diagnostic Criteria:
- productive cough for > 3 months in a year for > 2 consecutive years
Chronic Bronchitis (“blue bloater”)
Obstructive Lung Diseases:
- Findings:
- barrel-shaped chest, exhalation through pursed lips (increases airway pressure and prevents airway collapse)
- Centriacinar
- associated with smoking
- frequently in upper lobes (smoke rises up)
- Panacinar
- associated with α1-antitrypsin deficiency
- frequently in lower lobes
- Enlargement of air spaces ↓ recoil, ↑ compliance, ↓ DLCO from destruction of alveolar walls.
- Imbalance of proteases and antiproteases → ↑ elastase activity → ↑ loss of elastic fibers → ↑ lung compliance.
- CXR:
- ↑ AP diameter
- flattened diaphragm
- ↑ lung field lucency
Emphysema (“pink puffer”)
Obstructive Lung Diseases:
- Findings:
- cough, wheezing, tachypnea, dyspnea, hypoxemia, ↓ inspiratory/expiratory ratio, pulsus paradoxus, mucus plugging
- Triggers:
- viral URIs
- allergens
- stress
- Diagnosis is supported by spirometry and methacholine challenge.
- hyperresponsive bronchi → reversible bronchoconstriction
- smooth muscle hypertrophy and hyperplasia, Curschmann spirals (shed epithelium forms whorled mucous plugs), and Charcot-Leyden crystals (eosinophilic, hexagonal, double-pointed crystals formed from breakdown of eosinophils in sputum)
- DLCO normal or ↑
- type I hypersensitivity reaction
- Aspirin-induced _____ is a combination of COX inhibition (leukotriene overproduction → airway constriction), chronic sinusitis with nasal polyps, and _____ symptoms.
Asthma
Obstructive Lung Diseases:
- Findings:
- purulent sputum, recurrent infections, hemoptysis, digital clubbing
- Chronic necrotizing infection of bronchi or obstruction permanently dilated
- airways.
- Associated with bronchial
- obstruction, poor ciliary
- motility (eg, smoking,
- Kartagener syndrome),
- cystic fibrosis H, allergic
- bronchopulmonary
- aspergillosis.
Bronchiectasis
Restrictive Lung Diseases
- Restricted lung expansion causes ↓ lung volumes (↓ FVC and TLC). PFTs:↑ FEV1/FVC ratio.
- Patient presents with short, shallow breaths.
- Poor Breathing Mechanics (extrapulmonary, peripheral hypoventilation, normal A-a gradient):
- Poor Structural Apparatus—scoliosis, morbid obesity
- Poor Muscular Effort—polio, myasthenia gravis, Guillain-Barré syndrome
- Interstitial Lung Diseases (pulmonary ↓ diffusing capacity, ↑ A-a gradient):
- Pneumoconioses (eg. coal workers’ pneumoconiosis, silicosis, asbestosis)
- Sarcoidosis: bilateral hilar lymphadenopathy, noncaseating granuloma; ↑ ACE and Ca2+
- Idiopathic Pulmonary Fibrosis (repeated cycles of lung injury and wound healing with ↑ collagen deposition, “honeycomb” lung appearance and digital clubbing)
- Goodpasture Syndrome
- Granulomatosis with Polyangiitis (Wegener)
- Pulmonary Langerhans Cell Histiocytosis (eosinophilic granuloma)
- Hypersensitivity Pneumonitis
- Drug Toxicity (Bleomycin, Busulfan, Amiodarone, Methotrexate)
Respiratory Pathology:
- mixed type III/IV hypersensitivity reaction to environmental antigen
- causes dyspnea, cough, chest tightness, and headache
- often seen in farmers and those exposed to birds
- reversible in early stages if stimulus is avoided
Hypersensitivity Pneumonitis
Respiratory Pathology:
- characterized by immune-mediated, widespread noncaseating granulomas, elevated serum ACE levels, and elevated CD4+/CD8+ ratio in bronchoalveolar lavage fluid
- more common in African-American females
- often asymptomatic except for enlarged lymph nodes findings on CXR of bilateral adenopathy and coarse reticular opacities
- CT of the chest better demonstrates the extensive hilar and mediastinal adenopathy
- Associated with:
- Bell palsy
- Uveitis
- Granulomas (epithelioid, containing microscopic Schaumann and asteroid bodies)
- Lupus pernio (skin lesions on face resembling lupus)
- Interstitial fibrosis (restrictive lung disease)
- Erythema nodosum
- Rheumatoid arthritis-like arthropathy,
- hypercalcemia (due to ↑ 1α-hydroxylase–mediated vitamin D activation in macrophages)
- Treatment: steroids (if symptomatic)
Sarcoidosis
A facial droop is UGLIER.
- Bell Palsy
- Uveitis
- Granulomas
- Lupus pernio
- Interstitial fibrosis
- Erythema nodosum
- Rheumatoid arthritis-like arthropathy
Respiratory Pathology:
- complication of smoke inhalation from fires or other noxious substances
- caused by heat, particulates (< 1 μm diameter), r irritants (eg. NH3) → chemical tracheobronchitis, edema, pneumonia, and ARDS
- many patients present 2° to burns, CO inhalation, cyanide poisoning, or arsenic poisoning
- singed nasal hairs common on exam
- bronchoscopy shows severe edema, congestion of bronchus, and soot deposition
Inhalation Injury and Sequelae
Pneumoconioses
- Asbestos is from the roof (was common in insulation), but affects the base (lower lobes).
- Silica and coal are from the base (earth), but affect the roof (upper lobes).
Pneumoconioses:
- associated with shipbuilding, roofing, and plumbing
- “ivory white,” calcified, supradiaphragmatic and pleural plaques are pathognomonic
- risk of bronchogenic carcinoma > risk of mesothelioma
- affects lower lobes
- ferruginous bodies are golden-brown fusiform rods resembling dumbbells, found in alveolar sputum sample, visualized using Prussian blue stain, often obtained by bronchoalveolar lavage
- ↑ risk of pleural effusions
Asbestosis
Pneumoconioses:
- associated with exposure to beryllium in aerospace and manufacturing industries
- granulomatous (noncaseating) on histology and therefore occasionally responsive to steroids
- ↑ risk of cancer and cor pulmonale
- affects upper lobes
Berylliosis
Pneumoconioses:
- prolonged coal dust exposure → macrophages laden with carbon → inflammation and fibrosis
- also known as black lung disease
- ↑ risk for Caplan syndrome (rheumatoid arthritis and pneumoconioses with intrapulmonary nodules)
- affects upper lobes
- small, rounded nodular opacities seen on imaging
Coal Workers’ Pneumoconiosis
Pneumoconioses:
asymptomatic condition found in many urban dwellers exposed to sooty air
Anthracosis
Pneumoconioses:
- associated with sandblasting, foundries, and mines
- macrophages respond to silica and release fibrogenic factors, leading to fibrosis
- it is thought that silica may disrupt phagolysosomes and impair macrophages, increasing susceptibility to TB
- ↑ risk of cancer, cor pulmonale, and Caplan syndrome
- affects upper lobes
- “eggshell” calcification of hilar lymph nodes on CXR
Silicosis
The silly egg sandwich I found is mine!
Respiratory Pathology:
- malignancy of the pleura associated with asbestosis
- may result in hemorrhagic pleural effusion (exudative) and pleural thickening
- Psammoma bodies seen on histology
- Calretinin ⊕ in almost all _____, ⊝ in most carcinomas
- smoking not a risk factor
Mesothelioma
Respiratory Pathology:
- alveolar insult → release of pro-inflammatory cytokines → neutrophil recruitment, activation, and release of toxic mediators (eg. reactive oxygen species, proteases, etc.) → capillary endothelial damage and ↑ vessel permeability → leakage of protein-rich fluid into alveoli → formation of intra-alveolar hyaline membranes and noncardiogenic pulmonary edema (normal PCWP)
- loss of surfactant also contributes to alveolar collapse
- caused by sepsis (most common), aspiration, pneumonia, trauma, and pancreatitis
- diagnosis of exclusion with the following criteria:
- abnormal chest X-ray (bilateral lung opacities)
- respiratory failure within 1 week of alveolar insult
- decreased Pao2/Fio2 (ratio < 300, hypoxemia due to ↑ intrapulmonary shunting and diffusion abnormalities)
- symptoms of respiratory failure are not due to HF/fluid overload
- causes impaired gas exchange, ↓ lung compliance and pulmonary hypertension
- treat the underlying cause
- Mechanical Ventilation:
- ↓ tidal volumes
- ↑ PEEP
Acute Respiratory Distress Syndrome
ARDS:
- Abnormal chest X-ray (bilateral lung opacities)
- Respiratory failure within 1 week of alveolar insult
- Decreased Pao2/Fio2 (ratio < 300, hypoxemia due to ↑ intrapulmonary shunting and diffusion abnormalities)
- Symptoms of respiratory failure are not due to HF/fluid overload
Respiratory Pathology:
- repeated cessation of breathing > 10 seconds during sleep → disrupted sleep → daytime somnolence
- diagnosis confirmed by sleep study
- normal Pao2 during the day
- nocturnal hypoxia → systemic/pulmonary hypertension, arrhythmias (atrial fibrillation/flutter), sudden death
- hypoxia → ↑ EPO release → ↑ erythropoiesis
Sleep Apnea
Sleep Apnea:
- aespiratory effort against airway obstruction
- associated with obesity, loud snoring, and daytime sleepiness
- caused by excess parapharyngeal tissue in adults and adenotonsillar hypertrophy in
- children
- Treatment:
- weight loss
- CPAP
- surgery
Obstructive sleep Apnea
Sleep Apnea:
- impaired respiratory effort due to CNS injury/toxicity, HF, and opioids
- may be associated with Cheyne-Stokes respirations (oscillations between apnea and hyperpnea)
- treat with positive airway pressure
Central Sleep Apnea
Sleep Apnea:
- obesity (BMI ≥ 30 kg/m2) → hypoventilation → ↑ Paco2 during waking hours (retention); ↓ Pao2 and ↑ Paco2 during sleep
- also known as Pickwickian syndrome
Obesity Hypoventilation Syndrome
Respiratory Pathology:
- results in arteriosclerosis, medial hypertrophy, intimal fibrosis of pulmonary arteries, and plexiform lesions
- Course:
- severe respiratory distress → cyanosis and RVH → death from decompensated cor pulmonale
Pulmonary Hypertension (≥ 25 mm Hg)
- normal mean pulmonary artery pressure = 10–14 mmHg
Pulmonary Hypertension:
- oten idiopathic
- heritable PAH can be due to an inactivating mutation in BMPR2 gene (normally inhibits vascular smooth muscle proliferation); poor prognosis
- pulmonary vasculature endothelial dysfunction results in ↑ vasoconstrictors (eg. endothelin) and ↓ vasodilators (eg. NO and prostacyclins)
- other causes include drugs (eg. amphetamines, cocaine), connective tissue disease, HIV infection, portal hypertension, congenital heart disease, and schistosomiasis
Pulmonary Arterial Hypertension
Pulmonary Hypertension:
sauses include systolic/diastolic dysfunction and valvular disease
Left Heart Disease
Pulmonary Hypertension:
- destruction of lung parenchyma (eg. COPD)
- lung inflammation/fibrosis (eg. interstitial lung diseases)
- hypoxemic vasoconstriction (eg. obstructive sleep apnea, living in high altitude)
Lung Diseases or Hypoxia
Pulmonary Hypertension:
recurrent microthrombi → ↓ cross-sectional area of pulmonary vascular bed
Chronic Thromboembolic
Pulmonary Hypertension:
causes include hematologic, systemic, and metabolic disorders, along with compression of the pulmonary vasculature by a tumor
Multifactorial
Lung—Physical findings

Respiratory Pathology:
- excess accumulation of fluid between pleural layers → restricted lung expansion during inspiration
- can be treated with thoracentesis to remove/reduce fluid
Pleural Effusions
Pleural Effusions:
- ↓ protein content
- due to ↑ hydrostatic pressure (eg. HF) or ↓ oncotic pressure (eg. nephrotic syndrome, cirrhosis)
Transudate
Pleural Effusions:
- ↑ protein content, cloudy
- due to malignancy, pneumonia, collagen vascular disease, and trauma (occurs in states of ↑ vascular permeability)
- must be drained due to risk of infection
Exudate
Pleural Effusions:
- also known as chylothorax
- due to thoracic duct injury from trauma or malignancy
- milky-appearing fluid
- ↑ triglycerides
Lymphatic
Respiratory Pathology:
- accumulation of air in pleural space
- dyspnea and uneven chest expansion
- chest pain, ↓ tactile fremitus, hyperresonance, and diminished breath sounds, all on the affected side
Pneumothorax
Pneumothorax:
- due to rupture of apical subpleural bleb or cysts
- occurs most frequently in tall, thin, young males and smokers
Primary Spontaneous Pneumothorax
Pneumothorax:
- diseased lung (eg. bullae in emphysema, infections)
- mechanical ventilation with use of high pressures → barotrauma
Secondary Spontaneous Pneumothorax
Pneumothorax:
- caused by blunt (eg. rib fracture) or penetrating trauma (eg. gunshot)
- can be iatrogenic (eg. central line placement, lung biopsy, barotrauma due to mechanical ventilation)
Traumatic Pneumothorax
Pneumothorax:
- air enters pleural space but cannot exit → increasing trapped air
- trachea deviates away from affected lung
- needs immediate needle decompression and chest tube placement
- may lead to ↑ intrathoracic pressure → ↓ venous return → ↓ cardiac function
Tension Pneumothorax
Pneumonia:
- S. pneumoniae most frequently, also Legionella and Klebsiella
- Intra-alveolar exudate consolidation A ; may
- involve entire lobe B or the whole lung.
Lobar pneumonia
Pneumonia:
- S. pneumoniae, S. aureus, H. influenzae, Klebsiella
- acute inflammatory infiltrates from bronchioles into adjacent alveoli
- patchy distribution involving ≥ 1 lobe
Bronchopneumonia
Pneumonia:
- Mycoplasma, Chlamydophila pneumoniae, Chlamydophila psittaci, Legionella, viruses (RSV, CMV, influenza, adenovirus)
- diffuse patchy inflammation localized to interstitial areas at alveolar walls
- diffuse distribution involving ≥ 1 lobe
- generally follows a more indolent course (“walking” pneumonia)
Interstitial (Atypical) Pneumonia
Pneumonia:
- etiology unknown
- secondary organizing pneumonia caused by chronic inflammatory diseases (eg. rheumatoid arthritis) or medication side effects (eg. amiodarone)
- ⊝ sputum and blood cultures, no response to antibiotics
- formerly known as bronchiolitis obliterans organizing pneumonia (BOOP)
- noninfectious pneumonia characterized by inflammation of bronchioles and surrounding structure
Cryptogenic Organizing Pneumonia
Natural History of Lobar Pneumonia

Lung Cancer
- leading cause of cancer death
- Presentation:
- cough, hemoptysis, bronchial obstruction, wheezing, pneumonic “coin” lesion on CXR or noncalcified nodule on CT
- Sites of Metastases from Lung Cancer:
- adrenals
- brain
- bone (pathologic fracture)
- liver (jaundice, hepatomegaly)
- In the lung, metastases (usually multiple lesions) are more common than 1° neoplasms. Most often from breast, colon, prostate, and bladder cancer.
-
SPHERE of Complications:
- Superior vena cava/thoracic outlet syndromes
- Pancoast tumor
- Horner syndrome
- Endocrine (paraneoplastic)
- Recurrent laryngeal nerve compression (hoarseness)
- Effusions (pleural or pericardial)
- Risk factors include smoking, secondhand smoke, radon, asbestos, and family history.
- Squamous and Small cell carcinomas are Sentral (central) and often caused by Smoking.
Lung Cancer:
- central
- undifferentiated → very aggressive
- may produce ACTH (Cushing syndrome), SIADH, or antibodies against presynaptic Ca2+ channels (Lambert-Eaton myasthenic syndrome) or neurons (paraneoplastic myelitis, encephalitis, subacute cerebellar degeneration)
- amplification of myc oncogenes common
- managed with chemotherapy +/– radiation
- neoplasm of neuroendocrine Kulchitsky cells → small dark blue cells
- Chromogranin A ⊕, Neuron-Specific Enolase ⊕, Synaptophysin ⊕
Small Cell (Oat Cell) Carcinoma
Lung Cancer:
- non–small cell
- peripheral
- most common 1° lung cancer
- more common in women than men, most likely to arise in nonsmokers
- activating mutations include KRAS, EGFR, and ALK
- associated with hypertrophic osteoarthropathy (clubbing)
- Bronchioloalveolar subtype (in situ):
- CXR often shows hazy infiltrates similar to pneumonia
- better prognosis
- bronchial carcinoid and bronchioloalveolar cell carcinoma have lesser association with smoking
- glandular pattern on histology, often stains mucin ⊕
- Bronchioloalveolar subtype:
- grows along alveolar septa
- apparent “thickening”
- of alveolar walls. Tall,
- columnar cells containing
- mucus.
Adenocarcinoma
Lung Cancer:
- non–small cell
- central hilar mass arising from bronchus, cavitation
- cigarettes, hypercalcemia (produces PTHrP)
- keratin pearls and intercellular bridges
Squamous Cell Carcinoma
Lung Cancer:
- non–small cell
- peripheral highly anaplastic undifferentiated tumor
- poor prognosis
- less responsive to chemotherapy
- removed surgically
- strong association with smoking
- pleomorphic giant cells
Large Cell Carcinoma
Lung Cancer:
- non–small cell
- central or peripheral
- excellent prognosis
- metastasis rare
- symptoms due to mass effect or carcinoid syndrome (flushing, diarrhea, wheezing)
- nests of neuroendocrine cells
- Chromogranin A ⊕
Bronchial Carcinoid Tumor
Respiratory Pathology:
- localized collection of pus within parenchyma
- caused by aspiration of oropharyngeal contents (especially in patients predisposed to loss of consciousness [eg. alcoholics, epileptics]) or bronchial obstruction (eg. cancer)
- Treatment: antibiotics
- air-fluid levels often seen on CXR
- fluid levels common in cavities
- presence suggests cavitation
- due to anaerobes (eg. Bacteroides, Fusobacterium, Peptostreptococcus) or S. aureus
- _____ 2° to aspiration is most often found in the right lung
- location depends on patient’s position during aspiration
Lung Abscess
Respiratory Pathology:
- also known as Superior Sulcus Tumor
- carcinoma that occurs in the apex of lung may cause _____ syndrome by invading cervical sympathetic chain
- compression of locoregional structures may cause array of findings:
- recurrent laryngeal nerve → hoarseness
- stellate ganglion → Horner syndrome (ipsilateral ptosis, miosis, anhidrosis)
- superior vena cava → SVC syndrome
- brachiocephalic vein →brachiocephalic syndrome (unilateral symptoms)
- brachial plexus → sensorimotor deficits
Pancoast Tumor
Respiratory Pathology:
- an obstruction of the SVC that impairs blood drainage from the head (“facial plethora”; note blanching after fingertip pressure), neck (jugular venous distention), and upper extremities (edema)
- commonly caused by malignancy (eg. mediastinal mass, Pancoast tumor) and thrombosis from indwelling catheters
- medical emergency
- can raise intracranial pressure (if obstruction is severe) → headaches, dizziness, ↑ risk of aneurysm/rupture of intracranial arteries
Superior Vena Cava Syndrome
Respiratory Drugs:
reversible inhibitors of H1 histamine receptors
Histamine-1 Blockers
First Generation Histamine-1 Blockers
- Diphenhydramine
- Dimenhydrinate
- Chlorpheniramine
Respiratory Drugs:
- used for allergy, motion sickness, and sleep aid
- causes edation, antimuscarinic and anti-α-adrenergic effects
First Generation Histamine-1 Blockers
- Diphenhydramine
- Dimenhydrinate
- Chlorpheniramine
Second Generation Histamine-1 Blockers
- Loratadine
- Fexofenadine
- Desloratadine
- Cetirizine
Respiratory Drugs:
- used for allergies
- far less sedating than 1st generation because of ↓ entry into CNS
Second Generation Histamine-1 Blockers
- Loratadine
- Fexofenadine
- Desloratadine
- Cetirizine
Respiratory Drugs:
- expectorant
- thins respiratory secretions
- does not suppress cough reflex
Guaifenesin
Respiratory Drugs:
- mucolytic
- liquifies mucus in chronic bronchopulmonary diseases (eg. COPD, CF) by disrupting disulfide bonds
- also used as an antidote for acetaminophen overdose
N-Acetylcysteine
Respiratory Drugs:
- antitussive (antagonizes NMDA glutamate receptors)
- synthetic codeine analog
- has mild opioid effect when used in excess
- Naloxone can be given for overdose
- mild abuse potential
- may cause serotonin syndrome if combined with other serotonergic agents
Dextromethorphan
Respiratory Drugs:
- α-adrenergic agonists
- used as nasal decongestants
- used to reduce hyperemia, edema, and nasal congestion
- open obstructed eustachian tubes
- causes hypertension
- rebound congestion if used more than 4–6 days
- can also cause CNS stimulation/anxiety
- Pseudoephedrine—CNS stimulation/anxiety
- Phenylephrine
Pulmonary Hypertension Drugs:
- competitively antagonizes endothelin-1 receptors → ↓ pulmonary vascular resistance
- hepatotoxic (monitor LFTs)
- Example: Bosentan
Endothelin Receptor Antagonists
Pulmonary Hypertension Drugs:
- inhibits PDE-5 → ↑ cGMP → prolonged vasodilatory effect of NO
- also used to treat erectile dysfunction
- contraindicated when taking nitroglycerin or other nitrates
- Example: Sildenafil
PDE-5 Inhibitors
Pulmonary Hypertension Drugs:
- PGI2 (prostacyclin) with direct vasodilatory effects on pulmonary and systemic arterial vascular beds
- inhibits platelet aggregation
- Side Effects: flushing, jaw pain
- Examples: Epoprostenol, Iloprost
Prostacyclin Analogs
Asthma Drugs
- Bronchoconstriction is mediated by:
- inflammatory processes
- parasympathetic tone
- Therapy is directed at these 2 pathways.

Asthma Drugs:
- β2-agonist
- relaxes bronchial smooth muscle (short acting β2-agonist)
- used during acute exacerbation
Albuterol

Asthma Drugs:
- β2-agonist
- long-acting agents for prophylaxis
- adverse effects are tremor and arrhythmia
- Salmeterol
- Formoterol

Asthma Drugs:
- inhibit the synthesis of virtually all cytokines
- inactivate NF-κB, the transcription factor that induces production of TNF-α and other inflammatory agents
- 1st-line therapy for chronic asthma
- use a spacer or rinse mouth after use to prevent oral thrush
Inhaled Corticosteroids
- Fluticasone
- Budesonide

Asthma Drugs:
- competitively block muscarinic receptors, preventing bronchoconstriction
- also used for COPD
Muscarinic Antagonists
- Tiotropium—long acting
- Ipratropium

Asthma Drugs:
- antileukotrienes
- block leukotriene receptors (CysLT1)
- especially good for aspirin-induced and exercise-induced asthma
- Montelukast
- Zafirlukast

Asthma Drugs:
- antileukotriene
- 5-lipoxygenase pathway inhibitor
- blocks conversion of arachidonic acid to leukotrienes
- hepatotoxic
Zileuton

Asthma Drugs:
- binds mostly unbound serum IgE and blocks binding to FcεRI
- used in allergic asthma with ↑ IgE levels resistant to inhaled steroids and long-acting β2-agonists
Anti-IgE Monoclonal Therapy
- Omalizumab

Asthma Drugs:
- likely causes bronchodilation by inhibiting phosphodiesterase → ↑ cAMP levels due to ↓ cAMP hydrolysis
- usage is limited because of narrow therapeutic index (cardiotoxicity, neurotoxicity)
- metabolized by cytochrome P-450
- blocks actions of adenosine
Methylxanthines
- Theophylline

Asthma Drugs:
- prevent release of inflammatory mediators from mast cells
- used for prevention of bronchospasm, not for acute bronchodilation
Mast Cell Stabilizers
- Cromolyn
- Nedocromil

Respiratory Drugs:
- nonselective muscarinic receptor (M3) agonist
- used in bronchial challenge test to help diagnose asthma
Methacholine


