Pectoral Girdle/ Should/Arm/Elbow Flashcards
Describe the bony features shown on the image
What does tenderness at the two bony points on proximal humerus indicate?
What does tenderness inbetween these bony points indicate?

- Shown is the costal surface of the scapula which faces the ribcage
- Contains large concave depresssion = subscapular fossa, subscapularis originates here
- Originating superolaterally is the corcaoid process which is a hook like projection lying underneath the clavicle, palpable below lateral clavicle
- The acromion is the large palpable bony shelf felt above the shoulder
- On the humerus have the greater and lesser tubercles which serve as attachment points for the rotator cuff muscles
- Tenderness at the greater and lesser tubercles indicates potential injury to the rotator cuff muscles
- In between the greater and lesser tubercles is the intertubecular groove, where the biceps tendon sits.
- Tenderness here indicates biceps tendon inflammation

Describe the bony landmarks of the posterior scapula and humerus

- Posterior surface of the scapula faces outwards, it is the site of origin for the majority of the rotator cuff muscles of the shoulder
- Most prominent feature is the spine of the scapula running transversely across
- The acromion is seen laterally, is a projection of the spine that arches over the glenohumeral joint and articulates with the clavicle at the acromioclavicular joint
- above the spine of the scapula is the supraspinous fossa, supraspinatus muscle originates here
- inferiorly is the infraspinous fossa in which infraspinatus muscle originates
- medially is the medial border of the scapula and laterally see the lateral border
- Inferiorly see the inferior angle

What is the triangle of ausculation?
- Triangle of ausculatation of a relative thinning of the musculature on the back
- It lies medially to the medial border of the scapula at the inferior angle (medial border of the scapula forms the lateral boundary)
- inferiorly it is bordered by the superior portion of latissimus dorsi
- superiorly and medially it is bound by the inferior portion of trapezius

What vertebral spinous processes are marked by the:
superior angle
spine
inferior angle

- Superior angle marks the T2 spinous process
- inferior angle marks the T7 spinous process
- the Medial portion of the spine marks the T3 spinous process

What does the medial border of the abducted scapula mark?
- Medial border of the abducted scapula helps mark the oblique fissue of the lungs

What does the clavicle act as in the upper limb?
Clavicle acts as a strut to support the upper limb and transmit forces from the upper limb to the axial skeleton.
Forces move through the humerus, shoulder joint, into the scapula region, with forces passing through the clavicle into the manubrium of the sternum.
It also acts as a guide to keep the scapula away from the axial skeleton which allows the scapula to move freely around the wall of the thorax.

Why is the clavicle at high risk of fracture?
- Clavicle is at high risk of fracture as it acts as a strut that connects the upper limb to the axial skeleton
- Forces are transmitted from the upper limb, into the glenohumeral joint, across into the scapula region and into the clavicle where it articulates with the manubrium of the sternum at the manubrioclavicular joint.
- Clavicle can be fractured by a direct blunt force trauma, or by a fall onto an outstretched hand, transmitting forces to the clavicle.

What the two main joints of the clavicle?
What type of joints are they?
What is the likelihood of dislocation of these joints?
- The acromioclavicular joint --> between the acromion of the scapula and the clavicle, plane synovial joint that permits sliding. AC joint can dislocate and is relatively common
- the sternoclavicular joint --> between the clavicle and the manubrium of the sternum. Functions more like a ball and socket joint. Dislocation of the sternoclavicular joint is rare.

What is the clinical relevance of the sternoclavicular joint?
- Clinical relevance: Sternoclavicular joint:
- When injection or aspiration needs to take place at this site it must be done under ultrasound guidance
- This is due to the proximity of the apex of the lung and the high risk of pneumothorax
- There is also the risk of damaging the internal jugular vein and brachiocephalic vein.

What ligaments support the acromioclavicular joint?
Three main ligamnets that strengthen the acromioclavicular joint:
1) Acromioclavicular ligament runs horizontally from the acromion to the lateral clavicle, covers joint capsule reinforcing it superiorly.
2) Conoid ligament runs vertically from the coracoid process of scapula to the conoid tubercle of the clavicle
3) Trapezoid ligament runs from the coracoid process of the scapula to the trapezoid line of the clavicle.
Collectively conoid and trapezoid = coracoclavicular ligament

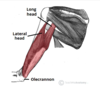
Label the image
What is each joint supported by? Name the ligaments.

- Top arrow (Left) –> Acromioclavicular joint (AC joint). Passes from anterior to posterior, dislocation of this joint leads to visibile deformity.
- Next arrow down –> coracoacromial ligament between the coracoid process and the acromium. It supports the shoulder joint superiorly. It can be ruptured by superiorly directed forces. Can impinge the supraspinatus/ subacromial bursa.
- Next arrow along –> coracoclavicular ligaments, formed of the trapzoid and conoid ligaments from coracoid process to clavicle. If the AC joint is dislocated these ligaments can be torn.
- Last arrow –> Sternoclavicular joint, only joint between upper limb and axial skeleton, supported by the costoclavicular ligament running from the 1st costal cartilage to the clavicle.

What can rupture the coracoclavicular ligaments?
- coracoclavicular ligaments run from the coracoid process to the clavicle, formed of trapezoid and conoid.
- They can be ruptured by acromioclavicular joint dislocation.
What is the pathology shown?

- Top image = normal acromioclavicular joint
- acromioclavicular joint = plane synovial joint, ends of the bone are covered in fibrocartilage (not hyaline) which absorbs xrays less than bone hence gap
- Bottom image = dislocated acromioclavicular joint, ends of the clavicle and acromion are not longer aposed.
- Will mean coracoclavicular ligaments are sprained/ torn, once ligaments are damaged at increased risk of damage recurring.

What are the most common sites of clavicular fracture? (in order of frequency)
What is the weakest point of the clavicle?
- in order of frequency the most common sites of clavicular fracture occur middle third > lateral third > medial third
- Weakest point of the clavicle is reported between the middle and lateral thirds.
- Note the fracture shown in image is a multifragmented, comminuted type fracture. (break of bone into two or more fragments).

How might a fractured clavicle present and why?
- Fractured clavicle presents as a distinct step often seen proximal to the individuals neck.
- Separated parts of a fractured clavicle move in opposite directions due to muscle contractions and gravity
- The sternocleidomastoid pulls the proximal fragment superiorly, wherease the weight of the upper limb pulls the distal fragment downwards.

Label the image
What is the clinical relevance of two of the bony landmarks of the humerus?

- Top arrow pointing to the articular head
- Then anatomical neck
- neck surgical neck = most common site for proximal humerus fracture, the axillary nerve is at risk of damage here
- shaft of humerus –> the radial nerve runs down the posterior of the humeral shaft in a spiral groove and is at risk of damage in a shaft fracture, along with profunda brachii artery.

Which nerve is at risk during a fracture of the surgical neck of the humerus?
- The surgical neck runs distal to the greater and lesser tubercles of the humerus to the shaft of the humerus
- The axillary nerve and posterior circumflex artery lie against the surgical neck at are at risk of damage
- surgical neck = frequent site of fracture either due to direct blow or fall on outstretched hand
- axillary nerve damage will result in paralysis to the deltoid and teres minor muscles
- patient will have difficulty performing abduction of affected limb
- axillary nerve also innervates skin over the deltoid, resulting in impaired sensation.

What type of joint is the shoulder joint?
What is it formed between?
what are the ends of the bones covered with?
how does the size of the humeral head compare to the glenoid fossa?
What function does this allow and at what cost?
what structure stabilised the joint?
- shoulder joint = ball and socket joint formed by the head of the humerus and the glenoid cavity/ fossa of the scapula (hence glenohumeral joint).
- Articulating surfaces are covered in hyaline cartilage
- head of humerus much larger than glenoid fossa giving wide range of movement at the cost of inherent stability
- Glenoid fossa is deepened by fibrocartilage rim called glenoid labrum.
What ligaments reinforce the glenohumeral joint?
- The glenohumeral ligaments (superior, middle and inferior) form the joint capsule and connect the humerus to the glenoid fossa. Main source of stability preventing anterior dislocation.
- Coroacohumeral ligament which attaches at coracoid process to greater tubercle of humerus supporting superiorly
- coracoclavicular ligament composed of trapezoid and conoid ligaments runs from clavicle to coracoid process of scapula.
- coracoacromial ligament from coracoid process to acromium, forms coracoacromial arch, prevents superior displacement of humeral head.

Label the image and describe the joint capsule of the glenohumera joint

- Top –> 3 x glenohumeral ligaments, form the joint capsule, support the joint anteriorly, projects from the glenoid to the humerus
- Bottom –> lax lower part of the joint capsule, permits range of movement -> to allow abduction
- Downward force applied at the joint capsule can lead ot dislocated shoulder.

Label the shoulder joint and describe the relevance of these features

- Top –> glenoid fossa = shallow socket that articulates with the head of the humerus, allows wide range of movement
- glenoid labrum surrounds the glenoid fossa, formed of fibrocartilage and deepens the socket to stabilise it. It can tear from overuse injury, producing a snapping sensation or pain on abduction or lateral rotation.
- superiorly the shoulder joint is supported by the coracoacromial arch, formed between the acromion, coracoid process and coracoacromial ligament
- The coracoid process acts as anatomical landmark, can access the shoulder joint via needle 2cm inferiorly to the coracoid process. Angle needle superolaterally.

What structures are present in the shoulder joint that reduce friction of the shoulder joint?
What is the clinical relevance of these structures?
Joint capsule = fibrous sheath that encloses the shoulder joint and extends from the anatomical neck of the humerus to the border of the glenoid fossa. It is lined with synovial membrane which produces synovial fluid to reduce friction between articular surfaces.
Several synovial bursae are present:
- Subacromial bursa –> deep to deltoid and acromion, superficial to supraspinatus tendon and joint capsule. Subarcomial bursa reduces friction beneath deltoid, promotes free motion of rotator cuffs.
- Subacromial bursitis can be cause of shoulder pain
- Subacromial bursa is subject to wear/ impingement and inflammation, especially in people with high level of upper arm activity.
- Subscapular located between subscapularis tendon and scapula.

Where can you inject the subacromial bursa?
- injection into subacromial bursa can take place via acromiodeltoid groove

Label the image and state the function of the superficial muscles shown

Left hand side = superficial muscles
- Top three arrows pointing to Trapezius:
- origin: base of skull, cervical vertebrae C7 and thoracic vertebrae down to T12 vertebra.
- Insertion: scapula, spine and acromium
- Action: upper fibres elevate the scapula, medial fibres retract the scapula, lower fibres depress the scapula
- Innervation: CN IX Accessory nerve
-
Latissimus dorsi:
- origin: from spinous processes of T6-T12, inferior 3 ribs
- Insertion: fibres converge into a tendon that attaches to intertubercular sulcus of humerus
- Action: extends, adducts and medially rotates the upper limb. Can raise the trunk to the arm during climbing.
- Innervation: Thoracodorsal nerve