Heart and mediastinum Flashcards
Describe the mediastinum - what does it separate from each other?
What splits the mediastinum into two regions and what are these regions called?
Describe where each of these regions begins/ ends
Describe what one of the regions is further split into and what is it split by?
The mediastinum is a broad central region that separates the two laterally placed pleural cavities (lungs surround the mediastinum).
The mediastinum is split into two regions by an imaginary line that runs from the sternal angle back to T4. Splits into the superior mediastinum and inferior mediastinum.
Superior mediastinum starts at the superior thoracic aperture and ends at the sternal angle
The inferior mediastinum starts at the sternal angle and ends at the diaphragm.
The inferior mediastinum is further split into anterior, middle and posterior region split by the pericardial sac.

What are the superior, inferior, anterior and posterior boundaries of the mediastinum?
Superior- superior thoracic aperture
Inferior - diaphragm
Anterior- sternum
Posterior- thoracic vertebrae (T1-T12)

On the image shown is this xray taken on inspiration or expiration?
How can you tell?
what midline structures can you see?
What structures can be seen entering the lung?
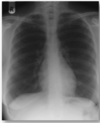
The Xray is taken during inspiration as there is a flattened costodiaphragmatic recess, the lung fields are large and you can clearly see ribs 5-7 anteriorly (the curved ribs) and to rib 10 posteriorly.
Centrally you can see the arch of the aorta (superior)
Inferior to this you can see the pulmonary trunk
On each lung the hilum is shown and the branching vessels entering the lung

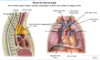
What are each of the arrows pointing to?

1) top arrow points to the anterior mediastinum which is a narrow region that can contain the thymus gland
2) middle arrow pointing to the costodiaphragmatic recess which is a region where fluid can collect especially pleural effusions
3) Most lateral arrow points to the posterior mediastinum which extends inferiorly to the 12th thoracic vertebrae.

Describe the borders of the anterior mediastinum and its contents
The anterior mediastinum begins inferior to the sternal angle and ends inferiorly at the diaphragm. Its anterior border is the sternum and posterior border the pericardium of the heart. It is bordered laterally by the parietal pleura around the lungs (mediastinal pleura).
Its contents includes the internal thoracic arteries and veins, fat and connective tissue and some thymus.

What procedure can the internal thoracic arteries be used for?
What vessels do these arteries give rise to in the thorax?
CABG- Coronary artery bypass graft (Internal thoracic artery used to divert blood past the blockage and is directly connected to the aorta).
Directly off the internal thoracic artery come the anterior intercostal arteries ( that form anastomoses with posterior intercostal arteries. )
Where is the thymus gland located normally?
What sign can this elicit on a chest xray in children?
Why would you not normally see this sign in adults? (how does the thymus change with age? and at what age?)
The thymus gland is normally located in the superior mediastinum and sometimes its inferior portion can project down into the anterior mediastinum.
In infants/children the thymus extends inferiorly and into the anterior mediastinum showing “ thymic sail sign” on chest x-ray.
With age (normally during puberty) the thymus recedes and is replaced by adipose tissue. Therefore would not expect to see thymus sail sign on an adult Xray- this is likely to indicate another pathology.

Describe the borders of the superior mediastinum
Anterior border - manubrium of sternum
Posterior border - Thoracic vertebra 1-4
Lateral borders- pleural cavities
superior border - superior thoracic aperture
Inferior border- continuous with inferior mediastinum at level of the sternal angle.

What structures pass through the superior mediastinum?
Vessels:
1) Aorta giving off the brachiocephalic trunk and L common carotic and subclavian
2) Superior vena cava receiving from the L and R brachiocephalic veins, the azygous vein on R side and supreme intercostal vein on the left which drains directly into the L brachiocephalic.
Nerves:
1) vagus
2) phrenic
3) Sympathetic trunk
Lymphatics: Thoracic duct which passes to the left of the oesophagus on its journey to the left internal jugular and subclavian veins.
Other structures:
1) trachea
2) oesophagus
3) thymus
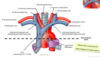
What structures are shown?
Explain what you can see from posterior- middle- anterior
Explain what is seen inferiorly
What is the ligamentous connection between the inferior most structure and middle structure?
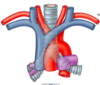
Most posterior structure- trachea, bifurcation into L and R main bronchi.
Most anterior is the superior vena cava, receiving the R and L brachiocephalic veins. The R and L brachiocephalic veins receive from the R and L internal jugular vein.
Middle structure - Arch of aorta, on R side brachiocephalic trunk which splits into the R subclavian and R common carotid. Splits into the L internal carotid and L subclavian.
Inferior stucture is the pulmonary trunk.
Ligamentous connection between the aorta and pulmonary trunk is called the ductus arteriosus. It fuses soon after birth- open in utero to bypass the deoxygenated blood past the lungs and straight into the aorta.
What happens if the ductus arteriosis remains open?
If the ductus arteriosus remains open this is called a patent ductus arteriosus and leads to mixing of deoxygenated blood and oxygenated blood.
This can put a strain on the heart and increase blood pressure in lung arteries.
Phrenic nerve passes ______ and the vagus nerve passes ______ to the hilum of the lung.
Phernic nerve passes anterior and the vagus nerve passes posterior to the hilum of the lung.

Describe the coarse of the vagus through the thorax and what branches it gives off to the larynx
What do these branches do, what type of fibres does it carry?
On which side would a hilar lymph node cause a hoarse voice?
What pathology could cause a hoarse voice on the other side?
The vagus nerve travels from the brainstem down into the thorax, posterior to the hilum of the lung.
The right vagus gives off the right recurrent laryngeal nerve at the level of the right subclavian artery.
The left vagus nerve gives off the left recurrent laryngeal nerve at the level of the aorta, it arches back up to reach the larynx.
The recurrent laryngeal nerve innervates all the muscles of the larynx except cricothyroid and does all the sensory innervation below the vocal folds. A pancoast tumour could compress the R RLN.
A hilar lymph node could cause a hoarse voice on the left side, swelling of the lymph node at the hilum could compress the left recurrent laryngeal nerve as it passes under the arch of the aorta.
What structures does the vagus nerve form a plexus around?
Which structure does the vagus use to enter the abdomen and what structure does it have to pass through?
What branches are on which side of this structure?
The vagus nerve forms a plexus around the trachea and oesophagus.
The vagus uses the oesophagus to enter the abdomen passing through the diaphragm. The left vagus nerve travels over the anterior surface of the oesophagus whilst the right nerve travels over the posterior.

What structure is very closely related to the left atrium of the heart posteriorly and how could this relationship be used?
The oesophagus lies directly behind the left atrium of the heart.
This can be used to image the heart via a transoesophageal ultrasound - noninvasive way to view the heart.
Can see in the image the left atrium of the heart has been cut away and you’re left with the pulmonary veins.

What are the borders of the posterior mediastinum?
Anteriorly- heart in pericardial sac
Posteriorly- T5-T12 thoracic vertebrae
Laterally- mediastinal pleura covering lungs
Inferiorly- diaphragm
Superiorly- continous with the superior mediastinum at the level of the sternal angle.

What are the contents of the posterior mediastinum?
- oesophagus
- Descending vagal plexus
- Sympathethic chain
- Descending aorta
- Azygous veins (azygous on R, hemiazygous and accessory on L)
- Thoracic duct (largest lymph drainage system in the body, beginning at cisterna chyli, ascending directly over T12-T6, travelling left to empty into left brachiocephalic vein).

Which two mediastinal areas does the oesophagus run in?
How does its muscular structure change as you move down the oesophagus (top 1/3 - bottom 2/3).
What is its innervation and what fibres does this innervation provide?
Oeosphagus travels within both the superior and posterior mediastinum.
Its internal structure changes from skeletal muscle which is under voluntary control in the proximal 1/3 to smooth muscle under autonimc control of the vagus nerve in the distal 2/3rds.
Motor and sensory is provided by the vagus.
What are the borders of the middle mediastinum?
anterior border- anterior margin of the pericardium
Posterior border- posterior margin of the pericardium
Superior- imaginary line continous with the sternal angle (T4)
inferior border- diaphragm
Lateral border- mediastinal surface of the pleura.

What are the contents of the middle mediastinum?
The pericardial sac and heart
The origins of the: aorta, Superior vena cava, pulmonary trunk
The phrenic nerve- splits into L and R phrenic nerves, runs in the middle mediastinum to reach the diaphragm.

What part of the heart attaches to the central diaphragmatic tendon?
The fibrous pericardium attaches to the central diaphragmatic tendon, meaning if the diaphragm moves the thoracic contents also move.

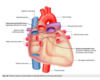
Describe the hearts shape from the anterior view
Apex of the heart hangs the most inferior and to the left, running laterally to the right is the diaphragmatic surface. The appendage (purple) is the right atrium.

Describe the shape of the heart from the posterior view

The base of the heart can be seen from the posterior view and is formed by the meft atrium NOT the diaphragmatic surface.
Below the base of the heart is the diaphragmatic surface formed by the let ventricle.
(can also see the R and L pulmonary arteries, SVC and IVC entering the Right atrium and the arch of the aorta.

The heart is a _________ structure that rotates to the _____ during development.
The heart is a midline structure that rotates to the left during development.
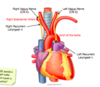
Label the anterior view of the heart explaining where the atria/ventricles are seen and what vessels can be seen.
What forms most of the anterior view of the heart vs posterior?
Starting on the right you can see the superior and inferior vena cava joining the Right atrium (With its auricular appendage shown). Going medially & superiorly there is the artch of the aorta (giving off its brachiocephalic trunk, left common carotid and left subclavian), and to the left of the aorta you can see the pulmonary trunk splitting into R and L pulmonary arteries. Inferior to the pulmonary trunk is the R ventricle forming most of anterior view of the heart. Following this across to the left we see a small part of the left ventricle which forms the apex of the heart. Right sided structures form most of the anterior whereas left sided structures form most of the posterior.

What might form in atrial appendages, especially in the case of atrial fibrillation?
Why is this dangerous?
There is a risk of blood clots forming in the atrial appendages due to small eddies being created that clot the blood when the atria fibrillate. This is dangeraous as the clots may be sent off the other parts of the body e.g. brain & stroke.
How many layers of connective tissue surround the heart and what are they collectively known as?
Describe the outer layer, name it, what is it made up of and what does it connect to? What is the function of this? Are there any negative consequences to its structure?
Describe the inner layer, name it, what forms it and any other names for these layers/what do they contact directly, what separates the layers and what is its function, what is this space called?
Two layers surround the heart and together are called the pericardium
1) Fibrous pericardium - formed by tough fibrous connective tissue that connects to the diaphragm below by its central tendon. It is a rigid structure that prevents overfilling of the heart bu is relatively non distensible which can cause clinical consequences- cardiac tamponade.
2) Serous pericardium layer formed of parietal and visceral pericardium. The visceral pericardium directly surrounds the heart and is known as the epicardium. It is separated from the outer parietal pericardium by serous fluid that helps the heart to beat without the pericardial layers rubbing against each other. This is known as the pericardial cavity. The outer parietal layer directly contacts the fibrous pericardium.

What are the 4 main physiological functions of the pericardium?
1) Fixes the heart by its connection to the central diaphragmatic tendon, limits its motion
2) Prevents overfilling of the heart- tough fibrous pericardium is relatively non-distensible, prevents hypertrophy
3) provides lubrication around the heart helping it to beat and reducing friction, small serous pericardial fluid in pericardial cavity helps this function.
4) protects the heart muscle from infection by forming a physical barrier between heart and structures that can easily become infected e.g. lungs.
What is pericarditis?
What does its pain presentation look like and why?
How does its pain presentation differ from MI?
Inflammation of the pericardial layers. (common causes bacterial/ viral infection/ post MI)
Patients describe continuous severe pain over their central chest that can radiate to either shoulder or arm regions. This is because the phrenic nerve does somatic sensory innervation to the parietal pericardium (C3/4/5) that also innervates the shoulder and parts of the arm. Unlike an MI, the pain can be relived on leaning forward.
What is a haemopericardium and how can this lead to a cardiac tamponade?
What else could lead to a cardiac tamponade?
Haemopericardium is a collection of blood in the pericardial cavity. As the fibrous pericardium is relatively inextensible this leads to clinical problems as the build up of blood compresses the heart tissue (known as cardiac tamponade) and can restrict Cardiac output- even becoming fatal when this compresses the ventricles.
Other causes are general pericardial effusion - where you have a build up of fluid in the pericardial cavity.
What lies within the pericardial sac?
The heart and the origin of the great vessels.

Where does the serous pericardium reflect upon itself in the heart and what does this form?
Which two locations does this occur at?
What does the space created by these reflections of serous pericardium form?
What do these spaces do?
The serous pericardium reflects around the roots of the great vessels and becomes the parietal pericardium.
This occurs at one superior site around the aorta and pulmonary trunk (arteries)
And at one inferior site around the superior and inferior vena cava (veins) and four pulmonary veins.
These reflections of serous pericardium forms the transverse and oblique coronary sinuses.
These spaces separate arterial outflow from venous inflow.

What shape is formed by the reflection of serous pericardium around the great vessels?
Describe where each sinus is
A J shape is formed by the reflection of the serous pericardium, the oblique portion running vertically down the posterior surface of the left atrium - oblique pericardial sinus.
The transverse pericardial sinus is located superior to the left atrium, posterior to the arch of the aorta and pulmonary trunk and anterior to the superior vena cava.
How do the pericardial sinuses come to be formed during development?
The pericardial sinuses are formed during development because the heart originally begins as a tube with separate ends for arterial outflow and venous inflow. This tube develops a kink in it as it takes on the shape of the heart and as it does so brings with it the pericardial layers that reflect at the great vessels, separating arterial outflow from venous inflow.

What is the clinical relevance of the transverse pericardial sinus?
As the transverse pericardial sinus separates the venous inflow from arterial outflow, it can be used in surgery to clamp the arterial outflow from the heart. A finger placed in the transverse sinus separates arterial outflow from venous inflow.

What valves lie between the atria and ventricles? what does this allow for? Describe the valves.
What are the valves anchored by?
What does the anchor attach to?
What is this attachment an extension of?
The atrioventricular valves lie between the atria and the ventricles and allow for unidirectional flow of blood from the atria to the ventricles. The valves are formed by flap-like cusps.
The valves are anchored by the chorda tendinae and these attache to the papillary muscles. The papillary muscles are an extension of the ventricular muscle.

What does papillary msucle contraction do?
Contraction of the papillary muscles pulls the chorda tendinae tight which keeps the AV valves from being blow back into the Atria and allowing backflow of blood.
What might happen after MI with damage to the papillary muscle?
What could you hear if this happened?
After MI, if the papillary muscles are damaged they will not be able to contract and pull on the chorda tendinae, therefore the valves could become incompetent and you end up with regurgitation of blood back into the atria.
You might hear a cardiac murmur with valve incompetency.

What three functions does the dense fibrous connective tissue (fibrous skeleton) of the heart provide?
Which node is the only route for signal conduction from the atria to the ventricles?
1) Mechanical stability
2) provides an anchor point for the heart valves and cardiac muscle
3) Electrical insulation: prevents “free” conduction of electrical signals from the atria to the ventricles- channels it down particular route (AV node) to allow proper timing of the contraction of the heart.
AV node is the ONLY route for signal conduction from atria to the ventricles

What is the fibrous skeleton of the heart?
Is a dense fibrous network that consists of 4 bands/rings of collagen each surrounding 1 of the 4 valves of the heart (aortic, pulmonary, bicuspid on left, tricuspic on right). Also attached to membranous bit of interventricular septum.

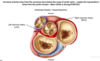
What are each of the arrows pointing to?

1) fibrous skeleton
2) bicuspid/ mitral valve
3) tricuspid valve

Describe the aortic and pulmonary valves
What spaces are behind each cusp?
Describe the movements of the cusps during ventricular systole and diastole
What other important structure fills during diastole?
Aortic and pulmonary valves are semilunar and each has 3 cusps that meet in the midline.
Pocket like spaces exist behind each of the three cusps - sinuses.
During ventricular systole, blood is forced upwards and out of the pulmonary trunk/aorta, which forces the cusps of the valves against the arterial wall and opens the valve.
During ventricular diastole, the ventricles relax and there is some blood flow back towards the ventricles as pressure in the ventricles becomes lower than that in the vessels. This backflow of blood fills the sinus of each cusp forcing them shut - closes the valve.
The coronary arteries also fill during diastole.
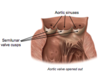
Aortic valve cusp nomenclature:
How does this change from the embryo to the adult and why?
In the embryo the heart has not yet rotated, therefore the two anterior cusps are known as left and right and one cusp at the back is posterior. The heart then rotates to the left, bringing with it the cusps which change their name.
There is one cusp anteriorly known as the anterior cusp and two other cusps posteriorly known as the L and R posterior cusps.

Pulmonary valve cusp nomeclature:
How does this alter from embryo to adult and why?
Again the heart has not yet rotated to the left in the embryo. In the embryo the pulmonary cusps are arranged with one cusp anteriorly and two posterior cusps (L and R).
Adult: rotation occurs to the left, the two L and R posterior cusps become anterior (LA & RA) and the formerly known anterior cusp becomes known as the posterior cusp.

What is the aortic sinus?
The aortic sinus is an anatomical dilation of the ascending aorta occuring just above the aortic valve. Widenings are between the wall of the aorta and each of the three cusps of the aortic valve.
Coronary arteries:
Where do they arise from, at what postion, what do they supply, when are they filled with blood?
What are the two main branches of coronary artery?
Arise directly off the aorta, just above the aortic valve in the coronary sinus. Fill with blood during ventricular diastole and they supply the myocardium (i.e the heart muscle itself).
Two main branches: Left and Right coronary arteries
What makes someone either Right or left coronary artery dominant?
Dominance of either the left or right coronary artery is dictated by which artery gives off the posterior interventricular artery (PIVA).
What is more common: right sided coronary artery dominance or left sided? (give reference to percentages)
Right sided coronary artery is more dominant (60%) vs left sided (40%)
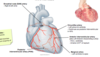
Where is the RCA vs the LCA?
What are the arrows pointing to?
what area does each branch supply?

The RCA comes off the aorta more medially. The first branch given off is the sinoatrial node artery (SAN) artery which supplies the SAN and R and L atria.
The next arrow down are the atrioventricular arteries that supply the AV node.
Next arrow down is the marginal artery which reaches the apex - supplies right ventricle and apex
Most medial arrow points to the PIVA which supplies the posterior 1/3 of the interventricular septum.

Which artery is the LCA?
What branches are each of the arrows pointing to?
What areas do they suppy?
Which artery has special clinical significance?

The LCA is shown coming off the back of the aorta.
The most superior arrow given off is the SAN artery that will supply the SAN, R and L Atria.
The next arrow down is the circumflex artery that supplies the LA and the LV, in 40% of people it continues inferiorly as the PIVA. (posterior interventricular artery).
The next arrow down is pointing to the LAD (left anterior descending) or the AIVA (anterior interventricular artery). This supplies the R and L ventricles and anterior 2/3rds of the septum.
Last arrow (most inferior) is the left marginal artery, supplies the left ventricle to the apex.
The LAD has special clinical significance as it is the most common site for plaque build up and occlusions.
LCA normally supplies?
Left atria and ventricle
AV node bundle
R and left bundle branches
Anterior IV septum (majority of the septum)
What type of imaging is this?
Is this the R or L coronary artery?
What are the arrows pointing to?
Is there any pathology in this image?

This is a coronary angiogram
This is the RCA.
Top arrow- RCA
next arrow down- SAN artery
next- AVN artery
next- right marginal artery
most inferior arrow- Posterior interventricular artery (PIVA)
Yes there is a slight RCA stenosis.
Is this a R or L coronary artery?
What are the arrows pointing to?

This is a left coronary artery- top arrow points to LCA curving around the left auricle.
Next arrow down points to the circumflex artery, which if you follow down gives of the left marginal artery
The medial arrow is pointing to the LAD - left anterior descending or anterior interventricular artery.
How does blood from the myocardium get drained?
What structure does it drain into and where does this sit in relation to the heart?
What does it drain directly into?
Via cardiac veins (great, small and middle) that empty into the coronary sinus.
The coronary sinus is the main vein of the heart located on the posterior of the heart in the coronary sulcus running between the left atrium and left ventricle.
The coronary sinus empties directly into the RA.

What are the three main veins that drain blood from the heart and where are they situated on the heart?
1) great and small cardiac veins are both on the anterior side of the heart.
Great cardiac vein originates at the apex of the heart, follows the anterior interventricular groove and goes into the coronary sinus around the left side of the heart.
The small cardiac vein passes around the right side of the heart to join the coronary sinus.
2) the middle cardiac vein is located on the posterior of the heart

Surface anatomy: The heart can be mapped out using 4 key points:
What are these points?
On the right side:
- In the 3rd costal cartilage, 1cm from the sternum is the R atrium and SVC.
- In the 6th costal cartilage, 1cm from the sternum is the bottom of the R atrium and IVC.
On the left side:
- In the 2nd costal cartilage, 1cm lateral to the sternum is the auricle of the left atrium and pulmonary trunk
- In the 5th intercostal space, just medial to the midclavicular line is the apex and left ventricle.

Surface anatomy and ausculation points:
Why are the surface marking points of the 4 cardiac valves and their ausculation points different?
The ausculation points are different as we want to listen to the flow of blood through the valves.
What are the ausculation points for:
1) aortic valve
2) pulmonary valve
3) tricuspid valve
4) bicuspid valve
1) Aortic- 2nd ICS, just lateral to sternum on the Right
2) pulmonary- 2nd ICS just lateral to the sternum on the left
3) Tricuspid- 4th/5th ICS just lateral to the sternum on left
4) Bicuspid/mitral- 5th ICS lateral to sternum, midclavicular line on the left

Right atrium receives venous flow from the upper and lower body and the heart muscle itself. Label the image shown.

Top to bottom from left to right:
SVC
Crista terminalis
Pectinate muscles
Fossa ovalis
Opening of coronary sinus
Tricuspid valve cusp
AVN
SAN
What is the fossa ovalis a remnant of?
What was its role in the embryo?
Fossa ovalis is a remant of the foramen ovale which was an opening that allowed blood to be shunted from the RA to the LA in the embryo, bypassing blood to the lungs which are relatively nonfunctional.
When the baby takes its first breath a pressure change induces the foramen ovale to close off, there appears only as a shallow impression in the adult.

The left atrium receives highly oxygenated blood from 4 pulmonary veins.
Label the image shown.
Top arrow is the left auricular appendage
Next arrow is the bicuspid valve (mitral valve)
Next arrow round to the right is the fossa ovalis
Last two arrows on the right are 2 of the 4 pulmonary veins.

How does the thickness of the Right ventricle walls differ to the right atrium and vs the left ventricle? Why?
The right ventricle walls are thicker than the right atrium as it needs to force blood a greater distance- to the lungs. The left ventricle walls are 3x thicker than the right as it reflects function: LV needs to overcome systemic resistance and ensure perfusion to the entire body.
What ligamentous structure exists between the pulmonary trunk and the aorta?
What is this a remnant of?
The ligamentum arteriosum a remnant of the ductus arteriosus exists between the pulmonary trunk and aorta.
Allowed blood to flow from the pulmonary trunk into the aorta in the embryo, bypassing the lungs which are relatively nonfunctional at this stage.
Label the image

From right to left going down:
1) ligamentum arteriosum
2) semilunar valve of pulmonary artery
3) Conus arteriosus - region before pulmonary artery
4) moderator band- component of the electrical conduction system
5) papillary muscle
6) chorda tendinae
7) Tricuspid valve

Label the image

Top to bottom left to right:
1) aortic valve
2) papillary muscle
3) trabeculae carnae
4) chorda tendinae
5) mitral valve

Describe the conduction of an electrical signal from the pacemaker down to the ventricles
Pacemaker: SAN produces the initial electrical impulse, this is conducted to the AVN and only to the AVN due the presence of a fibrous cardiac skeleton. At there AVN there is a slight delay and the impulse is carried forward down the interventricular septum, in the R and L bundle of His which reflect back up at the apex of the heart, becoming R and L purkinje fibres that carry the impulse from the apex across the ventricles- causing coordinated contraction.

What might be the consequence of a ventricular septal defect or an infarct?
Septal defect: E.g a hole in the interventricular septum could affect the conduction down R & L bundle branches
Infarct: necrosis of tissue that could affect conduction of impulse
How does the parasympathetic NS affect HR?
Where do the fibres come from?
Where do cardiac fibres arise?
Where do postganglionic fibres arise?
where is the cardiac plexus located and what fibres are contained in this plexus?
Decreases HR
Fibres come from Vagus nerve (CNX)
The cardiac fibres off the vagus nerve arise in the thorax
The postganglionic fibres arise from ganglia that are actually located on the heart.
The cardiac plexus is located between the posterior of the aorta and the anterior aspect of the trachea. It is formed from both parasympathetic and sympathetic fibres.

How does the sympathetic NS affect the heart?
Where does the sympathetic innervation to the heart come from? How does it travel to the heart?
Why during an MI can pain be referred to the central chest region and arm?
Sympathetic stimulation increases both the HR and the force of contraction.
The sympathetic innervation to the heart comes from the sympathetic chain either side of the vertebral column, arising at levels T1-T4.
The sympathetic cardiac nerves descend through the neck to the heart.
During an MI, visceral organ pain is transmitted via visceral afferent nerves that travel alongside the sympathetic supply, and enter the spinal cord at T1-T4 levels. At the same time, the spinal cord is receiving visceral afferent information from the periphery (dermatome). The brain processes the visceral organ pain as peripheral sensory pain and so pain is referred to the T1-T4 dermatomes. (T2/3/4 on central chest, T1 in arm).