Lecture 7- Pharmacovigilance and pharmacogenetics Flashcards
what is pharmacovigilence
“Process and science of monitoring the safety of medicines and taking action to reduce the risks and increase the benefits of medicines” – European commission

The most common clinical adverse event is
- a drug reaction
- ~6.5% of hospital admissions in the UK related to an ADR
- Extended clinical significance (beds, duration of stay, lost productivity)
Example of poor pharmacovigilance: Thalidomide
- Introduced in Germany in 1957 as a sedative and hypnotic
- Then used to treat morning sickness
- R-enantiomer has sedative effect, whereas the s- isomer is teratogenic
- Resulted in limb malformation (phocomelia)
- 10,00 babies affected, 2000 death
The changes
- Thalidomide produced non-lethal but significant visible effect.
- Why had so many damaged babies were born before anything was done?
- Today 10 cases would be enough
- Lessons learnt: adequate testing, reporting system
thalidomide risk vs harm
- Thalidomide now usen to treat cancer and leprosy
- Particularly useful in those not pregnant
- Used when risk is outweighed by potential benefit
One of the major roles of trials is to
determine serious ADRs

Adverse drug reaction vs events
- An adverse drug event is “an injury that occurs during treatment, and is not necessarily caused by the drug itself
- An adverse drug reaction is a “response to a drug which is noxious and unintended and which occurs at doses normally used in man - causal link.
Broadly 4 MOA of ADR
- Exaggerated response
- Desired pharmacological effect at alternative/additional site (GTN – headache)
- Additional/secondary pharmacological effect (QT length)
- Triggering an immunological response (anaphylaxis)
ADRs usually mimumic
disease or syndromes that occur natrually- may have non therapeutic causes
Managing and communicating risk to pt
Must make sure you are able to explain based on research the risk vs potential benefits to pts.
Example of scares to the public which have lead to poor public health outcomes
- 1960’s through spontaneous ADR reporting it became apparent COCP ↑risk of VTE
- therefore dose was reduced – efficacy was maintained and ↓VTE
- Risk became public - “pill scare”
- ↓OC without alternative contraception
- ↑abortion
- Further scares identified including MI and breast cancer which again resulted in ↓OC use
- Pregnancy is much riskier than use of OC inc. VTE!
Limitations of pre marketing clinical studies and ADR
- Small no. if pts
- Limited age and gender
- Selected following precise diagnoses
- Short, well define duration
- Specialist doctors and continuous follow up
- Concomitant therapeutics excluded (cant detect adverse drug reaction)
Detection of an ADR
- There may not been enough people in the trial to detect rare ADR
Spontaneous reporting of ARDs
*
Everyone’s responsibility to report ADR
- Producing a signal that creates further questions
- Lead to ↑↑ ADR reporting to MHRA
- Yellow card scheme in place to report:
- recently introduced products – all suspected ADRs inc. minor ones, all reactions to vaccines
- Established products – serious or unusual suspected reactions (life threatening, disabling or prolonging hospitalisation)
why are yellow cards used
- Simple
- Accessible
- Can report common and rare reactions for all drugs

drug efficacy
efficacy describes the maximum response that can be achieved with a drug
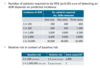
Poor drug efficacy
- present a substantial problem to medicine
- Majority of commonly prescribed drugs are only effective in 30-50% of individua’s
- 6.5% all hospital admissions
- 15% all hospital in patients
- 8000 overnight stays
- £1billion
- Majority of commonly prescribed drugs are only effective in 30-50% of individua’s

Factors Contributing to Interindividual Variability in Drug response
- Age
- Race/ethnicity
- Weight
- Gender
- Concomitant Diseases
- Concomitant Drugs
- Compliance
- Social factors
- Biomarkers
- GENETICS






