Lecture 20: Immune Deficiencies Flashcards
The infections associated with immunodeficiences have what typical features
- They are often chronic, severe, or recurrent
- They are not responsive well to an antibiotic therapy
- The microbes involved may be atypical or opportunistic
What are Primary imune deficiences (PIDs)
- Oftne clinically manifested during the first years of life (after 5-6 months):
- Because of Maternal IgG being in blood till about month 6, immune deficiences are not detected in the newborn
Maternal IgG in the infant begins to disappear after birth and has a half life of
25-30 days
What are the warning signs of Immunodefieciency disorder
- Medical History:
- Eight or more ear infections in one year
- Two or more serious sinus infections in one year
- Two or more bouts of pneumonia in one year
- Two or more deep-seated infections, or infections in unusual areas
- Recurrent deep skin or organ abscesses
- Need for IV antibiotic therapy to clear infection
- Infections with unusual or opportunistic organisms
- Family history of primary immunodeficiency
Adenosine Deaminase Deficiency (ADA) is considered a combined immune deficiency affecting:
- B cells
- T cells
- NK cells
X-linked Agammaglobulinemia
- an inherited immunodeficiency disease caused by mutations in BTK gene coding the Bruton Tyrosine Kinase (BTK)
- X-linked
- Diagnosis: in 5-6 month old
- Caused by defect in rearrangement of the Ig Heavy chain genes
- Early B-cell development is arrested at the pre-B cell stage → circulating B cells are usually absent or present in very low numbers (thus plasma cells are absent)
- IgG, IgA, and IgM are low or totally absent
- The Reticuloendothelial and lympohid organs in which B cells proliferate, differentiate, and are stored are poorly developed or absent:
- Spleen
- Tonsils
- Adenoids
- Peyer patches
- Peripheral lymph nodes

Autosomal recessive Agammaglobulinemia

Common Variable Immune Deficiency
- A heterogeneous group of diseases associated with hypogammaglobulinemia
- Both mlaes and females are equally affected (genetic inheritance pattern is not completely determined)
- Age of diagnosis
- greater than 2 years of age (can be in 20s or 30s)
- Onset
- is frequently after 4-5 years of age (between 2-80 years)
- Low IgG, IgA, Normal/Low IgM
- All paitents have hypogammaglobulinemia
- all isotypes or IgG only
- About 1/3 of patients have low B cells
- T cell deficience may alos occur
- may be caused by:
- Defects in B-cell formation
- (inherited)
- Abs against B cells (immune targeting)
- (inherited)
- Defects in B-cell formation
- Susceptible to reccurent bacterial infections
*

IgA deficiency
- incidence is relatively high
- 1:700
- Diagnosis
- often remain asymptomatic
- Prevalence may be higher in male patients
- Pathogenic mecahnism involves IgA secreting B cells:
- Disorder of maturation or Terminal differentiation
- Low IgA, normal IgG and IgM
Hyper IgM syndromes (HIGM)
- A group of diseases characterized by imparied Ig class switching and somatic hypermutation
- Patients with these sysndromes have an increased susceptibility to bacterial infection
- Normal numbers of peripheral B cells but low memory B cells
- Genetics:
- X-linked
- CD40L deficiency is responsible for 2/3 of cases of HIGM
- Without CD40L you can not have class switching and somatic hypermutation in B cells
- CD40L deficiency is responsible for 2/3 of cases of HIGM
- Autosomal CD40 deficiency
- Deficiency acounts for 1/3 of cases of HIGM
- X-linked
- High IgM, Low IgG and IgA

Isolated IgG subclass Deficiency
- Characterized by decreased concentrations of one or more IgG subclass
- Total IgG, IgM, IgA, and IgE are normal
- usually asymptomatic
- Low levels of IgG2 are frequent in children (association with poor responses to polysaccharide Ags)
- The IgG4 vary widely and many healthy people have no IgG4
- These deficiencies may be associated with recurrent viral/bacterial infections, frequently involving the respiratory tract
Transient Hypogammaglobulinemia of Infancy
- Low IgG/IgA, IgM can be normal
- Maternal IgG in the infant disappears after birth with a half-life of 25-30 days
- Intrinsic IgG production usually begins immediately after birth
- In transient hypogammaglobulinemia of infancy, intrinsic Ig production is delayed for up to 36 months
- Results in low IgG and IgA concentrations, but IgM concentration may be normal or low
- increased susceptibility to sinopulmonary infections
- in the majority of patients Ig concentrations normalize between 2 and 4 years of age
Wiskott-Aldrich Syndrome
- Low IgM; IgG normal, IgA and IgE are elevated
- X-linked recessive syndrome with progressive decrease in T cells
- The defect appears to be in a cytoskeletal protein called Wiskott Aldrich Syndrome Protein (WASP):
- WASP expression is limited to cells of hematopoietic lineage
- Clinical manifestations:
- Thrombocytopenia
- Small platelets
- Platelet dysfunction
- Eczema
- Susceptibility to infections
- in infants:
- prolonged bleeding from circumcision site
- Bloody diarrhea
- Excessive bruising
- Recurrent infection by Encapsulated Bacteria
- at risk for:
- Autoimmune diseases
- Cancer
Severe Combined Immune Deficiency (SCID)
- Associated with profound Deficiencies of T-cell and B-cell funciton (sometimes NK cell function)
- Typically demonsrate severe Lymphopenia
- At risk abortion of pregnancy:
- Inability to reject the maternal T cells that T cells that cross into the fetal circulation in utero
- Characterized by
- SEVERE OPPORTUNISTIC INFECTIONS
- or by chronic diarrhea and failure to thrive

Defects in T-Cell Function







Common Gamma Chain Deficiency (gammaC or IL-2Rgamma)
- Most common form of SCID
- X-linked
- Gene encodes Gamma-Chain shared by the T-cell gowth factor receptor (IL-2Rgamma) and other growth factor receptors
- There are no funcitonal B cells since T cells are unable to help
- T-,B+,NK-
- Susceptiable to:
- Opportunistic fungal infections, chronic diarrhea, skin, mouth, and throat lesions
Adenosine Deaminase Deficiency (ADA)
- Autosomal Recessive trait
- mutations in ADA gene
- second most common form of SCID
- ADA is essential for metabolic funciton of various cells especialy T cells
- ADA leads to an accumulation of toxic metabolic by-products adenosine and deoxy-ATP → lymphocytes die
- Susceptiablity to:
- Opportunistic fungal infections, chronic diarrhea, skin mouth, and throat lesion
- T-,B-,NK-
Deficiency of Jak3
- Autosomal recessive trait
- Defect in IL-2 receptor signaling
- Susceptible to:
- Opportunistic fungal infections
- Chronic diarrhea
- Skin, mouth, and throat lesions
- T-,B+,NK-
DiGeorge Syndrome (DGS)
- T-Cell deficiency
- caused by abnormalities in embryogenesis
- Features:
- Hypocalcemia (key feature)
- Parathyroid hypoplasia
- Thymic hypoplasia
- malformation of outflow vessels of the heart
- Delation of 22q11 chromosome
- Diagnsosis:
- Facial abnormalities
- Major outflow tract defect of the hear or history of recurrent infections
- Susceptible to:
- Oportunistic infections
- Fungal
- Viral
- Protozoal
- Recurrent with intracellular bacteria
- Oportunistic infections
MHC Class I Deficiency
- Caused by inability of TAP1 molecules to transfer peptides to ER
- CD8+ cells are deficient
- This leads to recurring viral infections
- CD4+ Are normal
- normal Ab production
- Normal DTH (delayed type hypersensitivity)

Bare Lymphocyte Syndrome
- A rare recessive disease
- No MHC Class II expression on professional APCS
- Gens for MHC class II on chromosome 6 are intact though
- Deficiency in CD4+ T cells
- Variable hypogammaglobulinaemia (mainly IgA and IgG2)
- Leas to recurrent infections and frequently to death in early childhood
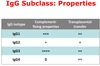
IgG subclass: Properties

What IgG subclass has the most complement fixing-properties
IgG3


