Bone and New Markers Flashcards
What are the 4 main functions of bone?
- Haematopoiesis
- Lipid and mineral storage (a reservoir holding adipose tissue within the bone marrow and calcium within the hydroxyapatite crystals)
- Support
- Protection
What type of tissue is bone?
Connective tissue
What are the 3 types of cells in bone?
- Osteoblasts
- Osteocytes
- Osteoclasts
Function of osteoblasts?
Secrete osteoid (bone forming cells).
Function of osteocytes?
Bone co-ordinating cells. As the osteoid mineralises, the osteoblasts become entombed between lamellae in lacunae where they mature into osteocytes. They then monitor the minerals and proteins to regulate bone mass.
- Mechanosensory mechanisms
- Co-ordinate bone turnover and remodelling
Function of osteoclasts?
- Secretes acid and collagenase in order to break down bone à bone resorption
- Helps regulate levels of blood calcium
Under the microscope, bone can be divided into two types. What are these?
- Woven bone (1ary bone)
- Lamellar bone (2ary bone)
What is woven (1ary) bone?
- Appears in embryonic development and fracture repair, as it can be laid down rapidly.
- It consists of osteoid (unmineralised ECM), with the collagen fibres arranged randomly. It is a temporary structure, soon replaced by mature lamellar bone.
What is lamellar (2ary) bone?
- The bone of the adult skeleton. It consists of highly organised sheets of mineralised osteoid.
- This organised structure makes it much stronger than woven bone.
- Lamella bone itself can be divided into two types – compact and spongy.
What is osteoid? What is it produced by?
Unmineralised portion of bone matrix that forms prior to the maturation of bone tissue. This will late become calcified/mineralised to form bone. Mainly composed of collagen. Secreted by osteoblasts.
What is the ECM of bone composed of?
- Organic matrix (30%)
- Mainly collagen (osteoid)
- Ground substance
- Inorganic components (70%)
- Hydroxyapatite (calcium and phosphate)
- Minerals (magnesium, sodium, potassium)
What 2 types can lamellar bone be divided into?
- Compact/cortical
- Trabecular/spongy
What forms the external protective layer of all bones?
Cortical bone
What type of bone gives bone its smooth, white, and solid appearance?
Cortical bone
What does cortical bone consist of?
- Multiple microscopic columns, each called an osteon
- Each column is multiple layers of osteoblasts and osteocytes around a central canal called the Haversian canal
- Haversian canals connected by horizontal Volkmann’s canals; these contain small vessels that anastomose with the arteries of the Haversian canals.

What is an osteon?
Fundamental functional unit of much compact bone. Roughly cylindrical structures; consisting of concentric layers (or lamellae) of compact bone tissue that surrounds the Haversian canal.

What is a Haversian canal?
Contains the bone’s blood supplies.

What are Haversian canals connected by?
horizontal Volkmann’s canals; these contain small vessels that anastomose with the arteries of the Haversian canals
Each osteon is composed of osteoblasts and osteocytes surrounding which canal?
Haversian canal
Describe the cortical:trabecular ration in vertebrae
Mainly trabecular bone and little cortical bone
What is trabecular bone? Where is it found? Composition?
- Spongy inner layer of bone
- May contain large spaces –> gives it honeycombed appearance
- Doesn’t contain any Volkmann’s or Haversian canals

What is ossification?
The process of producing new bone.
How is bone remodelling carried out?
It is carried out by the cellular component of bone:
- Osteoclasts resorb bone (over weeks)
- Nutriens are resorbed
- Osteoclasts signal to osteoblasts
- Osteoblasts lay down new osteoid
- Osteoid gets mineralised by minerals such as calcium and phosphate etc
- End up with white, hard bone

how long is one cycle of bone remodelling thought to be?
about 3 months
Where are osteoclasts found?
Found on those surfaces of bone which are undergoing resorption.
What are resorption bays?
On the surfaces of bone which are undergoing resorption, the osteoclasts are seen to be located in shallow depressions called resorption bays created by erosive action of osteoclasts on the underlying bone.
Which factors stimulate osteoclast activity?
RANK and RANKL signalling; regulates osteocyte formation, activation and survival in normal bone modelling and remodelling
Which factors inhibit osteoclast activity?
Osteoprotegrin: protects bone from excessive resorption by binding to RANKL and preventing it from binding to RANK; i.e. inhibits osteoclastogenesis and bone resorption

Which hormonal control are osteoclasts under?
- PTH
- Calcitonin
How does PTH affect osteoclast acitivty?
Stimulate bone resorption to increase blood calcium levels
Where is PTH released from?
Parathyroid glands
Where is calcitonin released from?
C cells of thyroid
How does calcitonin affect osteoclast activity?
Inhibits activity of osteoclasts to decrease blood calcium levels
How does IL-6 affect osteoclast activity?
Stimulates bone resorption and osteoclast activity to increase blood calcium levels
How are osteocytes formed?
Osteoblasts become trapped within osteoid and become osteocytes

Which bone cell has dendritic processes?
Osteocytes
How does aging affect bone? When is your peak bone mass?
- Decreasing bone mass with age
- Peak bone mass = 20s

Why do post-menopausal women experience a rapid decline in bone mass?
- Drop in oestrogen results in accelerated bone loss
- Osteoblastic activity falls and osteoclastic activity increases
What is effect of aging on osteoblastic activity and osteoclastic acitvity?
Osteoblastic activity falls and osteoclastic activity increases
For biochemical markers of bone turnover, what is being measured?
Bone formation and bone resorption
What biochemical markers are used to measure bone formation?
Products of active osteoblasts:
- Alkaline phosphatase (TAP, BAP)
- Bone-specific alkaline phosphatase (BAP) is synthesised by the osteoblasts
- Osteocalcin (OC)
- Procollagen type I propeptides (P1NP)
What biochemical markers are used to measure bone resorption?
- Degradation products of bone collagen:
- Hydroxyproline
- Pyridinium crosslinks
- Crosslinked telopeptides of type I collagen (NTX, CTX,)
- Osteoclasts enzymes:
- Tartrate-resistant acid phosphatase (TRACP 5b)
- Cathepsin K
What is alkaline phosphatase?
- An enzyme found in high amounts in bone and liver.
- Smaller amounts of ALP are found in the placenta of women who are pregnant, and in the intestines.
- Each of these body parts makes different forms of ALP. The different forms are called isoenzymes.
- What is bone alkaline phosphatase (BAP)?
- What is it synthesised by?
- When is it released?
- Bone-specific alkaline phosphatase (BAP) is synthesised by the osteoblasts
- Phosphatase is involved in mineralisation –> release stimulated by increased bone remodelling
When would you expect to see high levels of BAP?
- Childhood / Pubertal growth spurt
- Fractures
- Hyperparathyroidism
- Primary
- Secondary
- Pagets Disease of the Bone
Due to increased bone remodelling
- What is P1NP?
- What is it synthesised by?
- When is it released?
- Procollagen type 1N propeptide
- Synthesised by osteoblasts
- Precursor molecule of type 1 collagen
- Increased with increased osteoblast activity
- Decreased by reduced osteoblast activity
What are collagen cross-links (NTX, CTX)? When are they released?
- Cross-linking molecules which are released with bone resorption, correlate highly with bone resorption
- Increased in periods of high bone turnover
- Hyperthyroidism, adolescents, menopause
- BUT do not predict bone mineral density
- Decrease with anti-resorptive therapy
What are new bone markers used for?
- Evaluation of bone turnover and bone loss
- NOT diagnosis of disease
What is CTX (collagen cross-links) used to monitor?
response to anti-resorptive therapy
New bone markers can be used to evaluate adherence with medication. What marker is used to monitor:
- compliance with teriparatide?
- compliance/response to anti-resorptive therapy
- P1NP
- CTX
What are T-scores?
Calculates the number of standard deviations you are away from the mean compared to a young, healthy person of the same sex
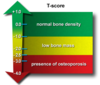
Which T-score is considered:
- normal bone density?
- osteopenia?
- osteoporosis?
- -1 and above
- between -1 and -2.5
- -2.5 and below
What is osteopenia?
Osteopenia is a condition that begins as you lose bone mass and your bones get weaker.
What is osteoporosis?
A systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue, with consequent increase in bone fragility and susceptibility to fracture.
Decreased bone mass + deranged bone microarchitecture = failure of structural integrity

Risk factors for osteoporosis?
- Aging
- Glucocorticoids
- No abnormalities are seen in routine biochemical tests
- Diagnosis relies on DEXA / X-Ray
- Increasing use of bone markers in management
Epidemiology of osteoporosis?
- 1 in 2 women and 1 in 5 men sustain fragility fractures after the age of 50 years.
- After a first fracture – 2-3-fold increased risk of another fragility fracture within the first 2 years.
what is a fragility fracture?
- A fracture caused by injury that would be insufficient to fracture a normal bone.
- Minimal trauma e.g. fall from a standing height
- Common sites:
- Spine
- Neck of femur
- Wrist
2ary causes of osteoporosis

What is FRAX calculator?
Calculates the 10-year probability of fracture with BMD.
What are the 2 main categories of osteoporosis treatment?
- Antiresorptive treatments
- Anabolic treatments

Difference between antiresorptive and anabolic treatments?
Antiresorptive agents reduce fracture risk by reducing the rate of bone remodelling so that fewer BMUs are available to remodel bone.
Anabolic agents reduce fracture risk by stimulating new bone formation, which partly restores bone volume and microstructure.
What are biphosphonates? Used for?
- Antiresorptive treatment
- Inhibit osteoclast formation

What is Denosumab (‘Prolia’)? Function?
- Antiresorptive treatment
- Inhibits RANK-Ligand –> inhibits osteoclast formation, function and survival which decreases bone resorption

What are 2 potential side effects of Denosumab?
- Osteonecrosis of the jaw
- Atypical femur fractures
What are bone metastases?
Bone metastasis occurs when cancer cells spread from their original site to a bone.
Which 5 cancers are most likely to metastasise to bone?
- Breast
- Kidney
- Lung
- Prostate cancer
- Thyroid
What are ‘lytic’ bone mets?
- Spots of bone damage that result from cancerous plasma cells building up in your bone marrow so bones can’t break down and remodel as they should.
- These metastases break down bone –> increased osteoclastic activity
Which type of bone mets lead to hypercalcaemia? Why?
Lytic bone metastases –> due to increased osteoclastic activity
What are sclerotic/osteoblastic bone mets?
- Unusual hardening or thickening of bone which can either be benign or malignant.
- Deposition of new bone
- Usual sites of spread:
- Spine, pelvis, femur,
- Humerus, skull
How do bone mets present?
-
Pain
- Often worse at night and gets better with movement initially
- Usually becomes constant
-
Broken bones
- Pathological fractures
- Commonly femur, humerus, vertebral
-
Numbness, paralysis, trouble urinating
- Spinal cord compression from bone metastases
-
Loss of appetite, nausea, thirst, confusion, fatigue
- Symptoms of hypercalcaemia
-
Anaemia
- Disruption of bone marrow
What is important to note about pain with bone mets?
- Often worse at night and gets better with movement initially
- Usually becomes constant
Why are the mild symptoms of hypercalaemia?
- Polyuria, polydipsia
- Mood disturbance
- Anorexia
- Nausea
- Fatigue
- Constipation
What are the severe effects of hypercalcaemia?
- Abdo pain
- Vomiting
- Coma
- Pancreatitis
- Dehydration
- Cardiac arrhythmias
What does a high calcium but low PTH indicate
Likely cancer
What does a high calcium and a high PTH indicate
Parathyroid problem
What are the causes of non-PTH mediated hypercalcaemia?

What is the next blood test you would do in anyone with a high calcium level?
Parathyroid hormone test
What is PTH secreted by?
Secreted by chief cells of parathyroid gland
Regulation of PTH levels diagram:

Describe the:
- Calcium
- PTH
- Phosphate
levels for 1ary, 2ary and 3ary hyperparathyroidism

Symptoms of 1ary hyperparathyroidism?
- Symptoms related to hypercalcaemia
- Renal disease (nephrolithiasis, chronic kidney disease)
- Bone disease (osteoporosis, osteitis fibrosa cystica)
- Proximal muscle wasting
What is the most common cause of 1ary hyperparathyroidism?
-
Adenomas (benign)
- Single adenoma account for 85% of cases of primary HPT
- Adenoma secretes PTH
What are 3 other causes of 1ary hyperparathyroidism?
- Glandular hyperplasia
- Ectopic adenomas
- Parathyroid carcinoma (malignant)
How does glandular hyperplasia present?
All 4 glands enlarged
What causes ectopic adenomas secreting PTH?
Parathyroid cells which migrated during embryogenesis
When does a parathyroid adenoma progress to a carcinoma?
- Features of invasion on histology
- Usually aggressive disease, with significant hypercalcaemia and possibility of distant metastases
Treatment for 1ary hyperparathyroidism?
In symptomatic patients:
- Surgery (unless patient doesn’t want)
- In asymptomatic patients with primary HPT only done if:
- Renal stone disease
- Bone disease
- Age <50 yrs
- Osteoporosis at any site or history of fragility fracture
- Medical: Calcimimetics (Cinacalcet)
In asymptomatic patients with 1ary hyperparathyroidism, when would surgery be done?
- Renal stone disease
- Bone disease
- Age <50 yrs
- Osteoporosis at any site or history of fragility fracture
What is Paget’s disease of bone?
- Rapid bone turnover and formation
- Leading to abnormal bone remodelling
- Clinical features:
- Bone pain
- Bone deformity
- Fractures
- Arthritis
- Cranial nerve defects/compression if skull affected
- Hearing and vision loss
- Risk of osteosarcoma due to high turnover
- Most commonly affects pelvis, femur and lower lumbar vertebrae
What are the ALP levels like in Paget’s disease of bone?
Elevated alkaline phosphatase reflecting increased bone turnover
What is osteomalacia? Commonest cause?
Osteomalacia refers to a marked softening of your bones, most often caused by severe vitamin D deficiency. Lack of mineralisation of bone.
Causes of osteomalacia?
- Insufficient calcium absorption from intestine
- Due to lack of dietary calcium or Vit D deficiency/resistance
- Excessive renal phosphate excretion
- Rare genetic forms (e.g. hereditary hypophosphataemic rickets)
Clinical features of osteomalacia?
- Diffuse bone pains
- Usually symmetrical
- Muscle weakness
- Bone weakness
Who is at risk of osteomalacia?
- Nursing home residents/ elderly
- Asian population (Hijab/ Burka wearing)
- Malabsorption
Describe the:
- Alk Phos
- Ca
- Phosphate
- PTH
In hyperPTH, osteomalacia, osteoporosis, Paget’s and bone mets



