Pharmacology - CNS, GI/Genitourinary, Infection, Pain, Toxicology Flashcards
Types of medications that affect CNS
1) anti-convulsants vs anti-seizures
2) Anti-parkinsons - usually for motor and neural discombobulation
3) Clot busters and thrombolytics for CVAs and TIAs
4) Behavioural meds for Anti-anxiety, neurolytics, and mood disorders
5) Opioids - usually considered analgesia but also greatly depresses CNS pathway (including HR and RR)
6) Anti-histamines
What are the 3 main neurological conditions encountered in pre-hospital settings requiring medications?
1) seizures
2) CVAs & TIAs
3) Mental illness
Two things neurological meds do
excite or suppress the CNS (uppers or downers)
Prime seizure disorder
epilepsy - idiopathic etiology
True or False. ABIs/TBIs can lead to seizures
True
True or false. If epilepsy disorders are not from an organic disorder (like febrile seizures, TBI) these can be corrected.
True
What is a seizure and how will the patient present?
- result of chaotic abnormal high frequent firing of neurons which can cause an altered LOC
- neurons are rapid firing with no organization, no rhythm to body
- patient is unconscious, no lash reflex
- eyes will deviate up to the left/right (to the side of the seizure in the brain)
Time frame for seizures
few seconds to 30 seconds, no more than 2 minutes
if > 2 min, high chance of brain cell death & severe cognitive impairment
True or false. Anti-Epiletic drugs will stop a convulsion once its started
False
Status epilepticus
ongoing and prolonged; starts and doesn’t stop OR continuous intermittent seizures (back to back i.e. one rolling right into the other)
True or False. Seizures typically resolve without treatment
True
What are pseudoseizures and what may a patient present like?
- by scientific definition - a psychiatric disorder brought on by stress or mental illness; a factitious disorder
- aka “fake seizures” - convulsing only, no organic brain involvement
- protected reflexes are still intact (i.e. lash reflex), can follow commands, hear. protect self, etc.
- cannot alter homeostatic balance
- roll eyes up/down or stare off into space
Pseudoseizures are now more commonly replaced with what term?
non-epileptic seizures
Pseudoseizures happen more commonly in what population
adolescence to early 20’s - more often in women
Epilepsy is most commonly diagnosed when?
before onset of puberty (usually in childhood)
Epilepsy
recurring seizures due to a brain disorder (organic brain dysruption)
Why do febrile seizures occur and what would be the appropriate treatment?
Usually triggered by fever/when kid gets too hot, the body is trying rid of excess heat but if the body cannot handle it, it will cause seizures to generate energy and give off this excess heat
Treatment: tylenol (anti-pyretic), remove clothes
Primary vs secondary seizures
Primary (idiopathic): undetermined cause - dx at a young age, accounts for ~50% of epilepsy cases
Secondary (symptomatic): distinct cause is identified
- trauma (sports, etc.); infection (sepsis); cerebraovascular disorders (TBIs, strokes, pregnancy); withdrawal (alcohol)
What are convulsions?
involuntary spasmodic contractions of any or all muscles through the body, including skeletal, facial, and ocular muscles
Is epilepsy the same thing as convulsions?
no. epilepsy is a chronic, recurrent pattern of seizures and a symptom of epilepsy would be convulsions
What are some common causes of seizures?
- TBIs/ABIs
- Epilepsy
- high fevers
- Anoxia (BP dropping so significantly due to lack of blood to the brain)
- Medicines,
- certain diseases
- alcohol/drug withdrawal
- trauma
- infection
- cerebrovascular disorders
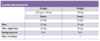
What are the 3 main types of seizures?
Focal - aka partial onset seizures
generalized
unknown
Describe the different categories of focal seizures.
1) Simple partial - aka petite mal/focal aware seizure: these patients are aware during the seizure and the seizure is happening in one small part of the brain
2) Complex partial - aka focal impaired awareness seizure: these patients are confused or their awareness is affected in some way during a focal seizure
3) Secondary generalized tonic-clonic: a seizure that starts in one area of the brain, then spreads to both sides of the brain as a tonic-clonic seizure
Describe what a focal seizure is and its clinical presentation
- abnormal electrical activity that occurs in one or more parts of one brain hemisphere; partial seizure
- It begins in one area (“focal”) and may progress to others, leading to a general seizure (bilateral tonic-clonic)
- they are aware or have impaired awareness
- can have motor or non-motor onset
- eyes will deviate to the side of the brain where the seizure is occurring