ANATOMY - Term Test 3 (Respiratory System) Flashcards
What structures play a role in air distribution?
all parts of the respiratory system except the alveoli
Functions of the respiratory system
- air distribution
- gas exchange
- filtering, warming, and humidifying inspired air
- Respiratory organs also help produce sounds (speech)
- olfaction (due to special sensory epithelium
- important role in regulation/homeostasis of body pH
Where is the cribriform plate located and what is its function?
- Separates the roof of the nose from the cranial cavity (as a barrier to stop nasties from leaking into cranial cavity)
- Has many small openings that permit branches of olfactory nerve responsible for the sense of smell to enter the cranial cavity and reach the brain
Structures of the upper respiratory tract
- nose
- nasopharynx
- oropharynx
- laryngopharynx
- larynx
What type of epithelium is in the respiratory portion of the nasal passage (i.e. respiratory mucosa)?
ciliated pseudostratified columnar epithelium (rich in goblet cells)
goblet cells produce and release mucus
Common name, structure and function of the pharynx
Common name: throat
Structure: tubelike structure (12.5cm/5 inch long) that extends from the base of the skull to the esophagus; lies anterior to cervical vertebrae; made of muscle and lined with mucous membrane (nonkertainized stratified squamous epithelium)
Function: common pathway for the respiratory and digestive tracts (because both air and food pass through before reaching their appropriate tubes (trachea & esophagus); speech production (phonation)
Where is olfactory epithelium found?
- Roof of nasal cavity and over superior turbinate and opposing portion of septum
- contains many olfactory nerve cells and has a rich lymphatic plexus
What is the more accurate term for the adam’s apple?
anterior laryngeal eminence (thyroid cartilage)
The eustachian tube connects the middle ear with what?
nasopharynx (or pharyngotympanic tube)
What is the name of the small leaf shaped cartilage behind the tongue and hyoid bone?
epiglottis (part of larynx)
What is the function of surfactant?
- Mix of phospholipids and proteins that lubricates the alveoli to prevent surface tension/friction between the water and air molecules (helps to decrease work of inspiration during respiratory cycle)
- prevents fluid contraction (due to surface tension) and alveolar collapse
- prevents airflow from small alveoli into larger alveoli (uneven ventilation)
- because without surfactant, smaller aveoli would tend to have higher pressure than larger alveoli causing air to move from small to larger alveoli (but surfactanct is more concentrated on small alveoli so the surface tension is reduced proprtionally)
Accessory organs of the respiratory system
Oral cavity, rib cage and respiratory muscles including the diaphragm
Where does cellular respiration occur?
mitochondria
The cribriform plate is part of which bone?
Ethmoid bone
What are the two parts of the respiratory tract?
- Upper tract (located outside the thorax/chest cavity): nose, nasopharynx, oropharynx, laryngopharynx, and larynx
- lower tract (located almost entirely within the chest cavity): trachea, all parts of bronchial tree, lungs

Which pair of tonsils are located in the oropharynx?
Palatine tonsils→ located in oropharynx behind and below pillars of the fauces (most commonly removed in tonsillectomy)
Lingual tonsils → located in oropharynx at the base of the tongue
Which pair of tonsils located in the nasopharynx?
Pharyngeal tonsils
- located in the nasopharynx (on its posterior wall opposite the posterior nares)
- refered to as “adenoids” when enlarged (may make it difficult for air to travel through from nose to throat if it becomes an obstruction)
*note: tubal tonsils also located in the nasopharynx - near opening of each auditory (eustachian) tube
Gas exchange occurs across which membrane?
respiratory membrane
Function of the turbinates in the respiratory tract
- Also called nasal conchae (superior, middle, inferior) on the lateral wall of the nasal cavity
- acts as baffles to slows and stir the air, as well as provide a large mucus-covered surface over which air must pass before reaching the pharynx (catches unwanted particles due to turbulence)
Role of surfactant
- produced by type II cells
- Covers each alveolus, helps reduce surface tension (force of attraction between water molecules) of the fluid
- Helps prevent each alveoli from collapsing and “sticking shut” as air moves in and out during respiration
How does the right bronchus differ from the left, and what effect might this have on the aspiration of objects?
The right bronchus is slightly larger and more vertical than the left (the heart takes up more room on the left side), making it more likely for aspirated foreign objects to be lodged in the R bronchus
What aspects of the structure of lung tissue make it efficient for gas exchange?
- Walls of alveoli and capillaries form a very thin barrier for gases to cross
- Simple squamous epithelial tissue makes up the respiratory membrane
- each alveolus lies in contact with blood capillaries and there are millions of alveoli in each lung
- alveoli and capillary surfaces have a HUGE surface area
- lung capillaries can accommodate a large amount of blood at one time
- blood is distributed through the capillaries in a layer so thin (diameter of one RBC) that each red blood cell comes close to alveolar air
What are the regulation processes associated with the functioning of the respiratory system?
- External respiration: pulmonary ventilation (breathing) and gas exchange in the pulmonary capillaries of the lungs
- Transport of gases by the blood
- Internal respiration: Gas exchange in the systemic blood capillaries and cellular respiration
- Overall regulation of respiration
Differences between (intra) alveoli and (intra) thoracic pressure after expiration and inspiration. (which is greatest of all those)
Inspiration:
- intrapleural pressure ~758mmHg (-2mmHg compared to atm pressure)
- during normal quiet inspiration, intrapleural pressure decreases further to 756mmHg or less
- as thorax enlarges, alveolar pressure decreases from atm level to -1 to -3 mmHg (therefore air moves into lungs)
Expiration:
- inspiratory muscles relax, causing a decrease in thoracic size and increase in intrapleural pressure (756+ mmHg)
- alveolar pressure increases, positive pressure gradient established from alveoli to atmosphere - expiration occurs
*

Which muscles are used for forced expiration?
abdominal and internal intercosal muscles
What happens when pressure in the lung is greater than atmospheric pressure?
Air moves down its pressure gradient so the air will move from the high pressure lungs, out into the atmosphere (aka expiration)
What is meant by vital capacity?
amount of air that can be forcibly expired after a maximal inspiration and therefore indicates the largest amount of air that can move into and out of the lungs during respiration
- ~4500 to 5000 mL
IRV (inspiratory reserve volume) + TV (tidal volume) + ERV (expiratory reserve volume) = vital capacity (VC)
- can vary with size of thoracic caviy, posture (larger VC when standing erect vs when stooped over/lying down), & various other factors (volume of blood in lungs - more blood = less alveolar air space = less VC)
- larger persion has a larger VC than a smaller person
- excess fluid in pleural or abdominal cavities decreases VC
- emphysema decreases VC (because alveolar walls become stretched, lose elastricity, unable to recoil normally after expiration = increased RV)

Excessive fluid in the pleural cavity would likely cause what?
decreased vital capacity (VC)
Why would a person skiing high in the mountains feel that they having trouble breathing?
- Alveolar air PO2 decreases as altitude increases, thus less oxygen enters the body at high altitudes
- At a certain high altitude, alveolar air PO2 = PO2 of blood entering pulmonary capillaries
- Gases move from an area of high pressure to low pressure, but because the pressure is the same in the pulmonary capillaries and the alveoli no movement or exchange takes place.
- Decreased oxygen diffusion into the blood
- this leads to trouble breathing
What helps determine the amount of oxygen that diffuses into the blood every minute?
1) The oxygen pressure gradient between alveolar air and incoming pulmonary blood (alveolar PO2 - blood PO2)
2) The total functional surface area of the respiratory membrane (area that is freely permeable to oxygen) - decrese in functional SA = decrease in oxygen diffusion
3) The respiratory minute volume (resp rate per minute x volume of air inspired per respiration) - decreased respiraory minute volume = decrease in oxygen entering into blood
4) Alveolar ventilation (the volume of inspired air that actually reaches the alveoli)
A period of hyperventilation leading to a loss of consciousness would be followed by what?
apnea
breathing stops entirely for a few moments (apnea) when arterial PCO2 drops moderately (such as during hyperventilation when lots of CO2 is being blown off)
The major form by which CO2 is transported is what?
Bicarbonate ions (67%)
Other forms:
- dissolved in plasma and transported as a solute - small amount (10%)
- carbaminohemoglobin - CO2 united with NH2 (amine groups) to form carbamino compounds (20-25%)
A sudden rise in arterial blood pressure will cause what?
- arterial blood pressure helps control breathing via respiratory pressoreflex mechanism
- sudden rise in arterial pressure acts on aortic and carotid baroreceptors and causes reflex of slowing respirations
- inversely, a drop in arterial pressure stimulates reflex to increase RR and depth
How is oxygen transported in the blood?
- Oxyhemoglobin (attaches to iron atom in each heme group) - majority
- only 1.5% travels as dissolved O2 in arterial plasma
*note that blood transports oxygen and carbon dioxide either as solutes or combined with other chemicals because fluids can only hold small amounts of gas in solution
Elastic recoil vs compliance
Compliance: ability for lungs/thorax to stretch out on inspiration - essential to normal respiration
- if compliance is reduced by injury/disease, inspiration becomes difficulty
Elastic recoil: tendency for lungs/thorax to return to pre-inspiration volume (if affected by disease, expirations must be forced even at rest)
Where are the inspiratory and apneuistic centers located?
Apneustic center: located in the pons - may provide input to the medullary rhythmicity area to regulate length and depth of inspiration
- damage to the nerves from the apneustic center is thought to produce abnormally long deep inspirations (apneustic breathing)
Inspiratory center: part of medullary rhythmicity area in medulla oblongata (brainstem)
Define internal respiration and external respiration
Internal respiration: gas exchange in the systemic blood capillaries and cellular respiration
External respiration: pulmonary ventilation (breathing) and gas exchange in the pulmonary capillaries of the lungs
Explain the relationship between the gas pressure gradient of the atmosphere and alveoli air that allows for inhalation
Inspiration: When atmospheric pressure is greater than pressure within the lung, air moves down its pressure gradient and air moves into the lungs
Inversely, if the pressure in the lungs becomes greater than the atmosphere, expiration occurs
What would you expect to happen to cellular respiration during exercise?
Cellular respiration increases which increases partial pressure of CO2 which goes down a chemoreceptor chain to increase respiration rate (body has greater requirement for oxygen)
1) Increased cell respiration during exercise cause a rise in plasma PCO2
2) This is detected by chemoreceptors ⇒ info is sent to respiratory centers in the brainstem
3) Respiratory muscles & diaphragm act as effectors which increase respiratory rate
4) As resp rate increases, the rate of CO2 loss increases and PCO2 drops
Why would a collapsed right lung due to a pneumothorax, also collapse the left?
- The pressure between the parietal and visceral pleura is always negative (less than the alveolar pressure) and this negative intrapleural pressure is required to overcome the lungs collapsing.
- A pneumothorax is air in the thoracic cavity and with a pneumothorax, the residual volume is eliminated
- Intrapleural pressure increases to atmospheric level, more pressure than normal is exerted on the outer surface of the punctured lung and causes it to collapse. - this also causes pressure buildup on the functional lung
- This pressure is due to the mediastinum being mobile, and the pressure is pushing the heart and other structures toward the intact side
COPD
Chronic obstructive pulmonary disease
- broad term used to describe conditions of progressive and irreversible obstruction of expiratory airflow
- chronic difficulties with breathing (mainly by emptying their lungs) and have visibly hyperinflated chests
- includes chronic bronchitis, emphysema
- Causes: tobacco use (primary cause); air pollution; asthma; resp infections
- Sx: productive cough, activity intolerance; can lead to acute resp failure, heart failure
- Treatment: brochodilators, corticosteroids
Restrictive pulmonary disorders
- disorders that involve restriction of the alveoli or reduced compliance, leading to decreased lung inflation.
- Hallmark: decreased lung volumes and capacities such as inspiratory reserve volume and vital capacity
- Factors: can originate within or outside lungs
- ex. alveolar scarring 2’ to work exposures (asbestos, fumes)
- immunological diseases (rheumatoid lung)
- obesity
- metabolic disorders (uremia)
- can also be from pain 2’ to inflammation or mechanical injuries
- Sx: dyspnea, intolerance to increased activity
- Tx: cause eliminiation, adequate gas exchange, improving exercise tolerance
Emphysema
- Air spaces distal to the terminal bronchioles are enlarged as a result of damage to lung connective tissue
- Bronchioles collapse and the alveoli enlarge, leading to rupture of alveolar walls and fusion into large irregular spaces (gas-exchange units are destroyed)
- Cause: unknown but potentially caused by proteolytic enzymes that destroy lung tissue
- Hypoxia often develops in people with emphysema

Bronchitis
- Production of excessive tracheobronchial secretions that obstruct airflow, bronchial mucus glands are enlarged
- air tubes narrow as a result of swollen tissues and excessive mucus production
- Risk Factors: cigarette smoking, normal decline in pulmonary function due to age, environmental exposure to dust and chemicals
- alveoli impaired and loss of capillary beds results in inefficient gas exchange which produces hypoxia

Asthma
- obstructive lung disorder characterized by recurring inflammation of mucous membranes (edema and ++mucus production) and spasms of the smooth muscles in the walls of the bronchial air passages (narrowing of airways due to inflammation)
- asthma attacks (acute onset) - can be triggered by stress, heavy exercise, infection, or allergen exposure/irritants
- Sx: dyspnea (major Sx); hyperventilation; headaches; numbness and nausea
- Treatment: inhaled or systemic bronchodilators to reduce muscle spasms and open airways; use of anti-inflammatory medications

Eupnea
- describes normal quiet breathing
- when the need for O2 and CO2 exchange is being met (normal breathing!)
- individual is not usually conscious of the breathing pattern
Dyspnea
- Labored or difficult breathing and is often associated with hypoventilation
- person is aware of breathing pattern and is generally uncomfortable/in distress
Biot Breathing
characterized by repeated sequences of deep gasps and apnea, abnormal breathing pattern seen in individuals with increased intracranial pressure
Cheyne-Stokes respiration
periodic type of abnormal breathing seen in terminally ill or brain damaged patients, cycles of gradually increasing tidal volume for several breaths followed by several breaths with gradually decreasing tidal volume.

Apneusis
Cessation of breathing in the inspiratory position. Respiratory arrest is the failure to resume breathing after a period of apnea or apneusis
Hyperventilation
- increase in pulmonary ventilation in excess of the need for oxygen
- sometimes results from a conscious voluntary effort preceding exertion of psychogenic factors (hysterical hyperventilation)
Apnea
temporary cessation of breathing at the end of normal expiration, may occur during sleep or when swallowing
Orthopnea
- dyspnea while lying down and is relieved by sitting or standing up
- common in patients with heart disease
Hyperpnea
- increased breathing that is regulated to meet an increased demand by the body for oxygen
- increase in pulmonary ventilation ocurs
- oxygen deman is met by increases in tidal volume and/or breathing frequency
- causes: exercise
Hypoventilation
- lower rate of breathing; decrease in pulmonary ventilation that results in elevated blood levels of CO2
Air inhaled through the mouth would be different than air inhaled through the nose. How?
Air through the mouth would not be as humidified, warmed or as filtered as air through the nose.
Cell respiration results in the production of what?
CO2
External structures of the nose
- i.e the structures that protrude the face (bony, cartilagenous framework covered by skin with sebaceous glands)
- two nasal bones that meet in the center of the face, below forehead (this is also surrounded by frontal bone)
- base of nose surrounded by maxilla laterally and inferiorly
- nostril openings (ala)
The flaring carilaginous expansion forming/supporting outer side of each oval nostril opening is called
ala
Internal portion of nose (nasal cavity) structure
- lies over roof of mouth where palatine bones separate nasal cavities from mouth cavity
- roof of nose is separated from cranial cavity the cribriform plate
Cleft palate
- When palatine bones fail to unite completely
- mouth is only partially separated from the nasal cavity, results in swallowing and speaking difficulties
The hollow nasal cavity is separated by a midline partition known as _______ into right and left cavities.
What structures is this partition composed of?
septum
4 main structures:
- perpendicular plate of ethmoid bone above
- vomer bone
- septal nasal cartilage
- vomeronasal cartilages
Superior, middle, and inferior meatuses
- nasal passageways in each nasal cavity
- These structures are made by the projection of the conchae/tubrinates curving from lateral walls of the internal portion of the nose
Anterior nares/external nares is also known as what?
What is their function?
nostrils
function: boundary between external environment and nasal cavity
After passing the anterior nares, what area does the air next enter (hint: structure located below inferior meatus)?
- vestibule - lined with skin; vibrissae (coarse hairs), sebaceous glands, and numerous sweat glands are in vestibule skin
- function of vestibule: conducts air between external environment and resp portion of nasal cavity
- vibrissae prevent entry of large contaminants
Sequence in which air passes through from nose to pharynx
Anterior/exteneral nares → vestibule → inferior, middle and superior meatuses (simultaneously) → posterior (internal) nares
respiratory portion (of each nasal passage)
- extends from inferior meatus to small funnel-shape of orifices of posterior (internal) nares
- posterior nares are openings that allow air to pass from nasal cavity into the pharynx
- where the respiratory mucosa is
Paranasal sinuses
- 4 pairs (frontal, maxillary, ethmoid, sphenoid sinuses)
- air-containing spaces that lighten weight of skull and open/drain into nasal cavity
- lined by resp mucosa
- their size and shape varies with ppl and change as we age
- Function: reduce weight of skull; help warm and humidify air

R and L front sinuses location
just above their corresponding orbit (so R and L orbit)
Maxillary sinus
- largest of the sinuses and extends into maxilla on either side of the nose
Sphenoid sinuses - location
in the body of the sphenoid bone on either side of the midline in close proximity to the optic nerves and pituitary gland
Which if the sinuses is a collection of small air cells divided into anterior, middle, and posterior groups (instead of a single large cavity)?
Ethmoid sinuses
The paranasal sinuses drain as follows:
- into middle meatus (passageway below middle concha) - frontal, maxillary, anterior, and middle ethmoid sinuses
- into superior meatus - posterior ethmoidal sinuses
- into space above superior conchae (sphenoehtmoidal recess) - sphenoid sinuses
Functions of the nose
- passageway for air going to and from lungs
- filters impurities, warms, moistened and chemically examines (via olfaction) to detecting potentially irritating substances
- nasal hairs (vibrissae) - “initial filter” to screen matter from air coming in
- turburinates/conchae then serve as baffles to slow and stir air & provide a large mucus covered surface area that air has to pass over before reaching pharynx
- mucus secretions in nose - final “trap” of remaining matter to be removed as it travels through nasal passages (along with lacrimal glands that do similar function)
- hollow sinuses act to lighten the skull bones - serves as resonating chambers for speech
- olfaction - swirling of air by middle and superior conchae over olfactory epithelium
The three anatomical divisions of the pharynx
1) Nasopharynx - located behind nose and extends from posterior nares to level of soft palate; conducts air between posterior nares and oropharynx
2) Oropharynx - located behind mouth from soft palate above to level of hyoid bone below; conducts air between nasopharynx and/or oral cavity and laryngopharynx
3) Laryngopharynx - extends from hyoid bone to esophagus; conducts betwen oropharynx and larynx
Openings found in the pharynx
There are 7
- R and L auditory (eustachian) tubes opening into nasopharynx
- 2 posterior nares opening into nasopharynx
- Opening from mouth (fauces) into oropharynx
- opening into larynx from laryngopharynx
- opening into esophagus from laryngopharynx
Common name, location, structure and function of the larynx.
Common nane: voice box
Location: lies between root of tongue and upper end of trachea, anterior to the lowest part of the pharynx; vestibule opening into the trachea from the pharynx
- thyroid gland and carotid artery touch the sides of the larynx
Structure: triangle shaped consisting of mostly cartilage attached to each other and surrounding structures via muscles/fibrous or elastic tissue; lined with ciliated mucous membrane (respiratory mucosa)
Function:
- respiration (part of airway to lungs) & removes dust particles via cilia, warms and humidifies inspired air
- protects airway against entrance of solids/liquids during swallowing
- voice production
Vestibular folds
- upper folds in the mucous membrane lining the larynx
- aka false vocal folds (because not involved in vocalization)
- Function: slow contaminents dripping toward lower airways
Vocal folds
- aka true vocal folds
- the lower pair of folds in the mucous membrane lining the larynx
- lined with nonkeratinized strategied squamous epithelium and supported by vocal ligament
- Function: produce sounds for speech/vocalization; prevent contaminents from entering lower airways
Rima glotidis
slitlike space between the left and right vocal folds, also the narrowest part of the larynx
Glottis
Vocal folds + rima glottidis (the slit-like space between the vocal folds)

The laryngeal cavity above the vestibular folds is called
vestibule
The very short middle portion of the cavity between the vestibular and vocal folds is the _________ of the larynx.
ventricle (or laryngeal ventricle)
The ____________ is the open space below the glottis.
infraglottic cavity (which conducts air between vocal folds and trachea)
Cartilages that make up the framework of the larynx
- 9 in total
- 3 largest - thyroid cartilage, epiglottis, cricoid cartilage (single structures)
- three pairs (so 6 total) of smaller accessory cartilages - arytenoid, corniculate, cuneiform cartilages
Thyroid cartilage
- Largest cartilage of the larynx
- gives larynx its characteristic triangular shape to its anterior wall
- creates the adam’s apple (larger in men than women and has less fat pad lying over it therefore it protrudes more in men)
Epiglottis
- small leaf-shaped cartilage that projects upward behind the tongue and hyoid bone
- attached below to thyroid cartilage
- has a free superior border that can flex to move up and down during swallowing to prevent food or liquids from entering trachea
- covered with nonkeratinized strategied squamous epithelium
Arytenoid cartilages
- pyramind shaped
- the most important of the paired laryngeal cartilages
- base articulates with superior border of cricoid cartilage
- anterior angles serve as points of attachment for the vocal folds
Intrinsic vs extrinsic muscles of the larynx
Intrinsic muscles:
- have both their origin and insertion on the larynx
- important in controlling vocal fold length and tension
- regulates shape of laryngeal inlet
Extrinsic muscles:
- insert on the larynx but have origina on some other structure (therefore, contraction of the extrinsic muscles actually moves or displaces the larynx as a whole)
*both: play important roles in respiration, vocalization, and swalloing
Trachea - Structure
- aka windpipe
Structure:
- tube ~11cm (4.5 inches; 2.5cm wide) long extending from larynx in neck to primary bronchi in the thoracic cavity
- outside of tracheal wall covered with fibrous adventitia
- smooth muscles in C-shaped rings of cartilage make up tracheal wall (and additional elastic fibers in the posterior wall)
- ^ rings are incomplete posteriorly - gives firmness to wall (prevents collapsing/shutting off vital airway) but also allows esophagus to expand as food moves toward stomach during swallowing
- lined with respiratory mucosa (ciliated pseduostratified columnar epithelium) with gobley cells in mucous glands creating mucus
Function of Trachea
- furnishes part of open passageway through which air can reach lungs from the outside (simple but VITAL function)
cutting of an opening into the trachea is known as
tracheostomy
Structure of bronchi/bronchial tree
- trachea divides into two primary bronchi (right slightly larger and more vertical than the left)
- structurally similar to trachea (icomplete cartilaginous rings in sections above the lungs, but complete rings in sections within the lungs)
- lined wtih ciliated mucosa
- enters lungs and immediately divides into secondary bronchi ⇒ tertiary bronchi ⇒ bronchioles and continue branching until terminal bronchioles
- trachea + 2 primary bronchi + their branches = bronchial tree
- 23 levels of branchings - optimum ability to transfer oxygen to pulmonary blood
- cartilagenous rings become irregular and disappear as it divides into small bronchioles
The __________________ are the last branches that serve solely to conduct air
terminal bronchioles
Divisions/Branches after terminal bronchioles
respiratory bronchies ⇒ alveolar ducts ⇒ alveolar sacs (which contain alveoli)

Estimated number of alveoli in lungs
300 million alveoli in total (both lungs)
Structure of alveoli
- spongelike structure
- extremely thin-walled (single layer of simple squamous epithelial tissue)
- lies in contact with blood capillaries
- millions of alveoli in each lung
Function of alveoli
- very effective in changing CO2 and O2 (due to thin walled, beside blood capillaries, and millions of alveoli in lungs)
The barrier across which gases are exchanged between alveolar air and blood is called _______.
What does this barrier consist of?
respiratory membrane
Barrier consists of alveolar epithelium, capillary endothelium, and their joined basement membranes
What keeps the alveoli from collapsing?
- surfactant
- structural interdependence of all the connected alveoli (they exert pull on each other to keep them all open)
The most important air purification mechanism in the respiratory tract is
The layer of protective mucus covering a large portion of the membrane lining the respiratory tree (125+ mL of resp mucus produced daily)
- creates a continuous sheet (mucus blanket)
- cilia moves the mucus upwards from bronchial tree to pharynx (to clear toxin molecules from the airway)
True or false. The cilia of the epithelial cells in the respiratory mucosa are motile, beating or moving in only one direction
True. upwards towards pharynx (to get it out of airway)
Prolonged exposure to toxins (such as smoking) can have what effect on cilia?
- Toxins can paralyze cilia causing the ciliary escalator to gradually fail
- accumulations of mucus trigger typical smoker’s cough (effort to clear secretions)
Function of Upper Respiratory Tract
- Processing of incoming air
- conducts air to and from lungs
- vocalization and phonation
- olfaction
Function of Nasal Cavity
- Conducts air between atmosphere and pharynx
- Warms, humidifies, and cleans inspired air
Function of tonsils
immune protection of respiratory and digestive mucosa
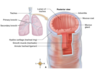
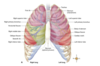
Structure of Lungs
- cone-shaped organs
- extend from diaphragm to just slightly above clavicles, and lie against ribs both anteriorly and posteriorly
- medial surface of each lung is more concave to allow room for other structures (like heart) - more concave on L because of this
Primary bronchi and pulmonary blood vessels (forming root of the lung) enter each lung through a slit on its medial surface called the ______.
hilum
Base vs apex of lung
Base: broad inferior surface of lung, which rests on diaphragm
Apex: pointed upper margin, projects above clavicle
Divisions of lungs
- divided into lobes by fissures
- oblique fissure is present in both lungs
- R lung has horizontal fissure separating superior and middle lobe
- Left lung - partially divided into two lobes (superior and inferior)
- right lung - three lobes (superior, middle, and inferior)
Lobes of the lung can be further subdivided into functional units called
bronchopulmonary segments
- has a lot of tubes of increasingly smaller diameter that make up bronchial tree and serve as air distributors
Visceral vs parietal pleura
Visceral: cover the outer surfaces of the lungs and adheres to them
Parietal: lines the entire thoracic cavity; aheres to the internal surface of the ribs and superior surface of the diaphragm; partitions off mediastinum
Function of the lungs
1) air distribution (by the bronchial tree)
2) gas exchange (via alveoli)
Structure of thoracic cavity
- has three divisions separated from one another by partitions of pleura
- contains the lungs
- space between the lungs is occupied by esophagus, trachea, large blood vessels, and heart
Visceral and parietal pleura are separated by __________.
Pleural space (a potential space) that contains just enough pelural fluid for lubrication
So when lungs inflate with air, the smooth, moist visceral pleura coheres to smooth moist parietal pleura (to avoid friction and painful respirations)
Pleurisy/pleuritis
pleura is inflamed causing respirations to become painful
Functions of the thoracic cavity
- respiration - elliptical shape of ribs and their attachment angle allows thorax to become larger when chest is raised and smaller when lowered
- diaphragm also contributes to thoracic volume - when diaphragm contracts, flattens out and pulls floor of thoracic cavity down (thus enlarges thoracic volume); when it returns to its resting, domelike shape, thoracic volume is reduced
Why does respiratory efficiency decrease with old age?
- ribs and sternum become more fixed and less able to expand during inspiration
- respiratory muscles are less effective
- Hb levels are often reduced
Upper respiratory infection (URI)
any infection localized in the mucosa of the upper respiratory tract (nose, pharynx, and larynx)
Rhinitis
- inflammation of the mucosa of the nasal cavity
- commonly caused by viral infection
- colder temps in nasal cavity during winter allow rhinoviruses (that cause common cold) to replicate more quickly (which increases common cold cases in the cold)
- can also be caused by nasal irritants, allergic reaction to airborne allergens
- Sx: excessive mucus production that drips down into throat and lower resp tract leading to sore throat, coughing, upset stomach, sneeze reflex
- Treatment: remove factor, rest, use of antihistamines, decongestants
Pharyngitis
- inflammation/infection of the pharynx
- aka “sore throat”
- often due to viral invasion
- includes strep throat - sore throat, redness, difficulty swallowing
- Treatment: throat lozenges, rest, fluids, antibiotics (if more severe)
Laryngitis
- inflammation of the mucous lining of larynx
- characterized by edema of vocal folds resulting in hoarseness (dysphonia) or loss of voice
- Causes: infections, toxic inhalation, endotracheal intubation, vocal abuse, alcohol infestion
- may lead to croup
- Treatment: conservative (limit talking)
Epiglottis
A rare but more severe and rapidly progressive viral form of laryngeal edema that needs medical treatment due to potential for airway obstruction
Tonsillitis
- inflammation of one or more masses of lymphatic tissue embedded in the mucous membrane of the pharynx
- most cases is inflammation of palatine tonsils (in oropharynx) and pharyngeal tonsils/adenoids (in nasopharynx)
- Tx: antibiotics, tonsillectomy
Why is it not uncommon to see common colds progress to sinus or middle ear infections?
because upper respiratory mucosa is continuous with mucous lining of the sinuses, eustachian tube (auditory tube), middle ear, and lower respiratory tract (which allows infections to spread)
Deviated septum
- displacement of nasal septum from midline of nasal cavity, may cause nasal obstruction
- common problem with deviated septum is snoring
sleep apnea
- condition where during sleep, there are periods of complete cessation of breathing
- periods of apnea are characterized by restlessness and often end in a loud “snort” before a normal breathing pattern resums
- can cause excessive daytime sleepiness and other sx related to chronic lack of oxygen
Acute bronchitis
- condition characterized by acute inflammation of tracheobronchial tree (most commonly caused by infection)
- prevalent in winter
- predisposing factors: chilling, fatigue, malnutrition, and exposure to air pollutants
- excessive fluid accumulates in bronchi
- Sx: nonproductive cough, potential malaise, fever, back and muscle pain, and sore throat
- Tx: rest, cough suppresants
Pneumonia
- common condition characterized by acute inflammation of the lungs
- alveoli and bronchi may become swolln and plugged with mucous secretions
- pus forms in bacterial pneumonia
- aspiration pneumonia: lung infections caused by inhalation of vomit or other infective material (common in acute alcohol intoxication and as a complication of anesthesia)
- Sx of pneumonia: high fever, chills, headache, cough, chest pain, leukocytosis, hypoxia
- Tx: antimicrobrial drugs, oxygen, removal of secretions
Tuberculosis (TB)
- chronic bacillus infection caused by Mycobacterium tuberculosis
- highly contagious, transmitted via airborne mechanisms
- inflammatory lesions (tubercles) form around colonies of TB bacteria in the lung and produce sx of cough, fatigue, chest pain, weight loss, and fever
- TB progression leads to lung hemorrhage and dyspnea
- can lead to scar tissue and reduced lung volume and restrictive lung disease
- can spread to other systems/organs
- tx: antimicrobials
Lung cancer
- malignancy of pulmonary tissue that destroys gas-exchange tissues and may also invade other body parts
- most often develops in damaged or diseased lungs (most common: cigarette smoking; other causes: asbestos, chromium, coal products, petroleum products, rust, ionizing radiation)
- Tx: surgery (removing lung or lobe); chemo; radiation therapy
Pulmonary ventilation
- term for “breathing”
- involves inspiration (moves air into lungs) and expiration (moves air out of lungs)
Primary principle of ventilation
This means that a fluid moves from the area where its pressure is higher to the area where its pressure is lower (with re: flow of air in pulmonary airways)
Under standard conditions, air in the atmosphere exerts a pressure of _______.
Air in the alveoli at the end of one expiration and before the begining of another inspiration exerts a pressure of ___________.
Both are 760mmHg
explains why at that moment, air is neither entering nor leaving the lungs
Air in the alveoli at the end of one expiration and before the begining of another inspiration exerts a pressure of ___________.
760 mmHg
when atmospheric pressure is greater than pressure within lung, air flows down gas pressure gradient meaning what?
air moves from atmosphere into lungs (inspiration)
When pressure in the lungs becomes greater than atmospheric pressure, air moves down gas pressure meaning what?
air moves out of lungs into atmosphere (expiration)

Pressure gradients are established by changes in what?
size of thoracic cavity, which is produced by contraction and relaxation of respiratory muscles
Boyle’s law
volume of a gas varies inversely with pressure at constant temp
can be applied to expansion of the thorax (increase in volume) resulting in decreased intrapleural (intrathoracic) pressure ⇒ leads to decreased intralaveolar pressure ⇒ causes air to move from outside into lungs

Charles’ Law
volume is directly proportional to temperature (V ∝ T) when pressure is constant
Application to ventilations: during inspiration, air expands in volume as it is warmed by respiratory mucosa

Dalton’s Law
- the total pressure exerted by a mixture of gases is the sum of the pressure of each individual gas
- aka the law of partial pressures
- Application to ventilations: used to determined partial pressure of oxygen (Po2) in air

Henry’s law
- the concentration of a gas in a solution depends on the partial pressure of the gas and its solubility, as long as temperature remains constant
- application: explains how plasma concentration of a gas such as oxygen relates to its partial pressure

The constant alternation between inspiration and expiration is called the:
respiratory cycle
Hyaline membrane disease (HMD)
- deficiency of surfactant in premature infants (because surfactant formation is not fully underway until 7th or 8th month of prenatal development)
- lack of surfactant decreases lung compliance, causing preemie to try and inflate alveoli by increasing effort of inspiratory muscles (which may eventually cause death by exhaustion) - known as respiratory distress syndrome (RDS)
- treatment:
- CPAP - artifically inflates baby’s lungs and maintains enough pressure during expiration to prevent collapse (to relieve baby’s inspiratory muscles)
- artificial surfactant
Quiet inspiration involves which muscles
- contraction of the diaphragm alone (descends to make thoracic cavity longer) OR
- ^ and contraction of external intercostal muscles (pulls anterior end of each rib up and out; also elevates attached sternum and enlarges thorax from front to back, side to side)
Chest-elevating muscles during inspiration
sternocleidomastoid
pectoralis minor
external intercostals
Why is the intrapleural pressure always lower than alveolar pressure?
- negative intrapleural pressure is required to overcome “collapse tendency” of the lungs caused by surface tension of fluid lining the alveoli and the stretch of elasti fibers that are constantly attempting to recoil
- difference (PIP - PA) is called transpulmonary pressure (which must always be negative to maintain inflation of the lungs)
Tidal volume
the volume of air exhaled normally after a typical inspiration
at rest in an adult: ~500mL (0.5L)

expiratory reserve volume (ERV)
the largest additional volume of air that can be forcibly expired after expiring tidal air
avg: 1000-1200mL (1 to 1.2L)
Inspiratory reserve volume (IRV)
amount of air that can be forcibly inspired over and above a normal inspiration
Normaly IRV: ~3300mL (3.3 L)
residual volume (RV)
amount of air that cannot be forcibly expired and remains trapped in the alveoli
~1200mL (1.2L)
between breaths, oxygen and CO2 exchange occurs between the trapped residual air in the alveoli and blood to help “level off” the amounts of oxygen and Co2 in the blood during breathing cycle
What happens to residual volume in pneumothorax?
residual volume is eliminated when the lung collapses BUT there is still a little bit of trapped air left called minimal volume which is about 40% of the RV
Inspiratory capacity (IC)
max amount of air an individual can inspire after nromal expiration
IC = TV + IRV
Functional residual capacity (FRC)
amount of air left in the lungs at the end of a normal expiration (without contracting expiratory muscles)
FRC = ERV + RV
~2200 - 2400 mL (2.2-2.4L)
Total lung capacity
the total volume of air a lung can hold
TLC = TV + IRV + ERV + RV
Alveolar ventilation
- volume of inspired air that actually reaches or “ventilates” the alveoli
- only this volume of air takes part in gas exchange (because a portion of air does not descend into any alveoli and therefore is not involved in this)
- alveolar ventilation volume = TV - dead space volume
Anatomical dead space vs alveolar dead space
- Anatomical dead space: the large air passageways that contains the “dead air” (i.e. the air that does not ventilate the alveoli but fills our air passageways) - ~30% of the TV
- Alveolar dead space: when some alveoli are not able to perform gas exchange and therefore also “dead space”
- both of those^ make us physiological dead space
Emphysema and its effect on dead space air/physiological dead space
- increases the amount of dead space air/physiological dead space
- so alveolar ventilation decreases which decreases oxygen getting to the blood aka inadequate air-blood gas exchange
Total minute volume
volume moved per minute (at rest ~6000mL)
TV (ml/cycle) x RR (cycles per min) = Total minute volume
500 ml/cycle x 12 breaths/min = 6000 mL
Maximum oxygen consumption (VO2 max)
- represents amount of oxygen taken up by the lungs, transported to the tissues, and used to do work
- predictor of a peron’s capacity to do aerobic exercise
- largely determined by herditary factors, but aerobic training can increase it by up to 35%
Forced expiratory volume (FEV) test
- can determine presence of respiratory obstruction by measuring volume of air expired per second during forced expiration
- volume forcefully expired during first second (FEV1) ~83% of VC
- volume forcefully expired during first 2 seconds (FEV2) ~94% of VC
- volume forcefully expired by end of 3rd second (FEV3) ~97% of VC

How is alveolar perfusion matched with alveolar ventilation?
- the idea behind this is to increase efficiency by detouring blood flow away from poorly ventilated alveoli towards well-ventilated alveoli so that blood flow doesn’t get wasted
- done by vasoconstraction of certain pulmonary arterioles to reduce perfusion to poorly ventilated alveoli

The basic rhythm of the respiratory cycle of inspiration and expiration is generated by the _____________.
medullary rhythmicity area
- consists of two centers: dorsal resp group (DRG) and ventral resp group (VRG)
- DRG integrates info from chemoreceptors for PCO2 and signals VRG to alter breathing rhythm to restore homeostasis
Pontine respiratory group (PRG)
- previously known as pneumotaxic center
- in the pons
- may regulate both the apneustic center and medullary rhythmicity area
Hiccup
- describes an involuntary, spasmodic contraction of the diaphragm
- contraction generally occurs at the beginning of an inspiration
- glottis suddenly closes producing a characteristic sound
- may be produced by irritaiton of the phrenic nerve or sensory nerves in he stomach; direct injury or pressure on certain areas of the brain
Cough reflex
- stimulated by foreign matter in the trachea or bronchi
- epiglottis and glottis reflexively close
- contraction of expiratory muscles cause air pressure in lungs to increase
- epiglottis and glottis then open suddenly, resulting in upward burst of air to remove contaminants
Sneeze reflex
- similar to cough reflex except stimulated by contaminants in the nasal cavity
- burst of air is directed through the nose and mouth, forcing contaminants (and mucus) out of respiratory tract
Yawn
- slow deep inspiration through an unusually widened mouth
- several theories for cause: thought to be done to prepare muscles and circulatory system for action; that it cools the brain (to regulate body temp); potentially triggered by NT related to mood
Diving reflex
- protective physiological response to cold water immersion
- the colder the water, the better chance of survival
- immediate shunting of blood to core body areas with peripheral vasoconstraction and bradycardia; slowed metabolism and decreased tissue requirements fo oxygen and nutrients
How does the cerebral cortex influence breathing?
- impulses to respiratory center from motor area of cerebrum may either increase or decrease rate and strengths of respirations (i.e. person can voluntarily speed up/slow down RR)
- voluntary control is limited though (because holding breath will cause increase in CO2 which will stimulate respirations)
The feedback sensors providing information to the medullary rhythmicity area are:
-
central chemoreceptors in the brain
- sensitive to ongoing changes in pH that is diff than peripheral chemoreceptor sensitivity
- CO2 crossing the BBB is not buffered by CSF or IF (different than in the blood where it can be buffered)
- best at detecting LT changes in CO2 rather than rapid changes in CO2/pH
- therefore respond to high CSF PCO2 and/or low CSF pH
-
peripheral chemoreceptors in peripheral sensory nerves in carotid bodies and aorta
- stimulated by large increases in arterial PCO2, low PO2, low plasma pH
- responds to rapid changes
- results in faster breathing
What would you expect to happen when there is a drop in arterial Pco2?
- inhibition of central and peripheral chemoreceptors leading to inhibition of medullary rhythicity area and slower respirations
How may a decrease in arterial blood PO2 (<70 mmHg, at a low but not critical level) regulate respiratory mechanisms?
- decrease in arterial blood PO2 may stimulate chemoreceptors in the carotid and aortic bodies and cause reflex stimulation of the inspiratory neurons of the medullary rhythmicity area
- makes a “backup” respiratory control mechanism
- *note: Po2 does not regulative respirations under normal conditions
Hering-Breuer reflexes
- reflex that also helps control respirations (depth and rhythmicity when TV is high)
- on large TV inspired: expansion of lungs stimulate stretch receptors that send inhibitory impulses to the inspiratory neuron ⇒ relaxation of inspiratory muscles occur ⇒ expiration follows Hering-Breuer expiratory reflex
- on large TV expired: lungs are delated to inhibit lung stretch receptors and allow inspiration to start again (Hering-Breuer inspiratory reflex)
Miscellaneous factors that may also influence breathing
- sudden painful stimulation - produces reflex apnea, but continued pinful stimuli cause faster and deeper respirations
- sudden cold stimuli - applied to skin cause reflex apnea
- stimulation of pharynx or larynx - by irritating chemicals or by touch causes temporary apnea (choking apnea - prevents aspiration of food or liquids during swallowing)
How are respirations affected during exercise?
- respirations increase abruptly at the beginning of exercise and decrease markedly as it ends
- unknown mechanism (changes in arterial blood PCO2, PO2, and pH are not enough to produce the degree of hyperpnea observed)
Obstructive vs. restrictive pulmonary disorders
Obstructive: obstruction of airways (such as bronchial constriction); may obstruct inspiration and expiration
Restrictive: restriction of alveoli, reduced compliance, leading to decreased lung inflation; typically restricts inspiration
Sudden Infant Death Syndrome (SIDS)
- “crib death”
- occurs most commonly in babies with no obvious medical problems who are younger than 3 months
- exact cause unknown
Physiologically spekaing, air in the lung is not part of our body. True or False.
True. inspired air is not part of the internal environment (as the airways are merely inward extensions of the external environment and have not crossed the barrier ie the respiratory membrane, into the body yet)

Partial pressure
pressure exerted by any one gas in a mix of gases or in a liquid
Gas mixture in atmospheric air
78% nitrogen
21% oxygen
1% CO2 & other gases
Exchange of gases in the lungs - what is happening during this exchange?
1) oxygen diffuses down its pressure gradient (moving from alveolar air to blood because PO2 in alveolar air is > PO2 of incoming blood)
2) CO2 exits from the blood by diffusing down the CO2 pressure gradient out into alveolar air (PCO2 of venous blood is bit higher than PCO2 in alveolar air)
*note that alveolar partial ressures stay relatively the same/constant whereas the partial pressures of gases in blood change to equilibrate with alveolar partial pressures (this is because alveoli are continually ventilated)

Fick’s Law
- principle that describes diffusion of CO2 and oxygen across respiratory membrane
- net gas diffusion rate across a fluid membrane is proportional to the membrane SA, gas solubility in the membrane, partial pressure difference; inversely proportional to membrane thickness
- each gas diffuses more efficiently if SA is large, if membrane thickness is small, if solubility of gas is high, and if partial pressure gradient is high
Avg oxygen saturation of Hb in systemic arterial blood and venous blood
arterial blood: 97%
venous blood: 75%

Which direction does oxygen and CO2 move during systemic gas exchange?
1) oxygen diffuses out of arterial blood into interstitial fluid/intracellular fluid because arterial blood PO2 is ~100mHg and IF/ICF is lower (pressure varies)

Right shift
- right shift of oxygen-Hb dissociation curve resulting from increased PCO2 (Bohr effect)
- when increased PCO2 decreases the addinity between Hb and oxygen
Haldane effect
refers to increased total CO2 loading caused by decrease in PO2
(decreased plasma PO2 commonly observed in systemic tissues increases the CO2 content of the blood, shown as a left shift of the CO2 dissociation curve)


