PCTH - Head Injuries Flashcards
What % of multi-system trauma patients will presetn with some form of TBI? How does this increase the mortality rate?
40%; increases mortality rate by 2x
List the structures that are considered as part of the head.
1) scalp
2) skull
3) meninges
4) brain tissue
5) CSF
6) vascular components
7) facial structures
What does CSF look like?
straw coloured fluid (typically mixed with blood)
Brain adjusts its own blood flow in response to _____________. Autoregulation is controlled by the level of what?
metabolic needs
CO2
Hypoventilation would cause an (increase/decrease) of CO2 in the brain, leading to (vasodilation/vasoconstriction).
Hyperventilation would cause an (increase/decrease) of CO2 in the brain, leading to (vasodilation/vasoconstriction).
Hypoventilation: increase CO2; vasodilation
Hyperventilation: decrease in CO2; vasoconstriction
Primary brain injuries occur when…..?
when there is immediate damage to the brain (i.e. baseball bat hitting the skull) - results from mechanical injury at the time of the trauma
Secondary brain injuries
- as a result of the initial impact (ex. brain being injured as a result of hitting the inside of the skull, of a bat hitting the skull which is your primary injury)
- can lead to swelling which can cause a decrease in perfusion
- results in hypoxia
- presence of edema increases intracranial pressure and exacerbates reduction in blood flow
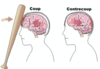
Coup-Contre Coup Injury
A coup injury occurs on the brain directly under the point of impact (primary impact)
A contrecoup injury occurs on the opposite side of the brain from where the impact occurred (secondary impact)
Primary brain injuries are best managed by:
prevention (occupant restraint systems, sports equipment, helmets, etc.
Cerebral Herniation
- sudden increase in ICP
- portions of the brain get pushed down into foramen magnum
- increase pressure on brain stem = cerebral herniation
What is a concern regarding hyperventilating all patients with TBIs?
you are delivering significant amount of oxygen to the patient which causes vasoconstriction and reduced oxygen flow to brain causing cerebral ischemia
oxygen is a vasodilator. true or false?
false. it vasoconstricts
S/S of Cerebral Herniation
- rapidly decreasing LOC
- dilated pupil and downward outward deviation of the eye on the side of the injury
- paralysis of the arm and leg on the side of the injury OR decorticate/decerebrate posturing
- Cushing’s Triad/Reflex
- Rapid decline in sx to cardiac arrest
Cushings Triad/ Reflex
↑ BP (usually 170-180 SBP)
↓ HR (bradycardia)
irregular RR
The purpose of hyperventilating a patient with cerebral herniation is because….?
you want to induce vasoconstriction to reduce swelling pushing into brainstem where respiratory center is
As per the Head Injury Standard of the BLS, the paramedic shall:
*long answer ahead
1) Consider potential life/limb/function threats, such as:
- intracranial and/or intracerebral hemorrhage,
- neck/spine injuries
- facial/skull fractures, and
- concussion;
2) observe for:
- fluid from ears/nose (e.g. CSF)
- mastoid bruising
- abnormal posturing
- periorbital ecchymosis
- agitation or fluctuating behaviours
- urinary/fecal incontinence
- emesis (projectile)
3) ventilate patient if patient is apneic or respirations are inadequate,
- a) if ETCO2 monitoring is available,
- i. attempt to maintain ETCO2 values of 35-45 mmHg,
- however, if signs of cerebral herniation are present after measures to address hypoxemia and hypotension, hyperventilate patient to attempt to maintain ETCO2 values of 30-35mmHg. Signs of cerebral hernation include a deteriorating GCS < 9 with any of the following:
- dilated and unreactive pupils,
- asymmetric pupillary response, or
- a motor response that show either unilateral or bilateral decorticate (check with brian) or decerebrate posturing, or
- b) if ETCO2 monitor is unavailable, and measures to address hypoxemia and hypotension have been taken, and patient shows signs of cerebral herniation (as mentioned above), hyperventilate the patient as follows:
- i. adult: approx 20 breaths/min (1 breath every 3 seconds)
- ii. child: approx 25 breaths/min (1 breath every 2-3 seconds)
- iii. infant < 1 y.o.: approx 30 breaths/min (1 breath every 2 seconds)
4) if protruding brain tissue is present, cover with non-adherent material (eg. moist, sterile dressing; plastic wrap);
5) if CSF leak is suspected, apply a loose, sterile dressing over source opening;
6) if patient is conscious and SMR is not indicated as per SMR standard, position patient in sitting or semi-sitting
7) if patient is on a spinal board or adjustable break-away stretcher, elevate head 30 degrees; and
8) prepare for potential problems, including,
- respiratory distress/arrest,
- seizures,
- decreasing LOC, and
- agitation and combativeness (from hypoxia)
Pupils are controlled by what cranial nerve?
CN III (oculomotor)
How can pupils present in head injuries and what is it an indication of? (4)
1) dilated and fixed - likely dead
2) dilated but reactive - probably gonna die
3) unilateral and dilated reactive - early sign of herniation
4) unilateral dilated unreactive - herniation
What are important factors to assess in TBI/head injury patients?
1) MOI
2) loss of consciousness
3) level of consciousness/behaviour
4) base line vitals, Cushings
5) Estimated blood loss
*always remember to examine things like helmet
How should you manage bleeding in traumatic head wounds?
expect ++ bleeding
large bulky dressings
no hemostatic dressings
avoid direct pressure
As per Neck/Back Injury Standard in the BLS, the paramedic shall:
1) if patient has penetrating neck, injury, assume vascular and airway laceration/tears;
2) auscultate patient’s lungs for decreased air entry and adventitious sounds
3) observe for:
- diaphragmatic breathing
- neurological deficits - weakness, lack of coordination, paralysis (any body part), paresthesia, priapism
- priapism, and
- urinary/fecal incontinence/retention;
4) perform, at minimum, a secondary survery to assess,
- for airway and/or vascular penetration (eg. frothy/foamy hemoptysis)
- lungs, for decreased air entry and adventitious sounds through auscultation,
- head/neck, for JVD and tracheal deviation, and
- chest, for subcutaneous emphysema, and
5) if patient has a penetrating wound,
- assess for entry and exit wounds,
- apply pressure lateral to, but not directly over the airway, and
- apply occlusive dressing to wounds; use non-circumferential bandaging
With impaled objects in the neck/back, what is would a paramedic’s protocol be?
make no attempt to remove!
stabilize with layers of bulky dressing/bandages (i.e. log cabin) unless otherwise specified by the Standards, or the object is compromising the airway
Treatment consideration re: SMR and open neck wounds.
- Apply SMR with caution when treating patients with open neck wounds
- traditional c-collars may impede proper assessment and treatment
- manual stabilization may be required via head blocks/blankets
The #1 cause of non-traumatic back pain is
chronic pain


