Basic Nephrology: The Renal Tubules Flashcards
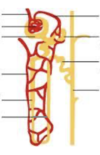

Note: Reabsorption in PCT

reabsorption/secretion in early PCT
ISOTONIC ABSORPTION

how does PTH an ATII affect early PCT reabsorption
PTH: inhibits Na+/PO43- cotransport, causes increase phosphate excretion
ATII: stimulates Na+/H+ exchange, increases sodiun, water and HCO3- reabsorption (permitting contraction alkalosis).
reabsorption in thin descending loop of henle
passively reabsorbs H2O via medullar hypertonicity (impermable to Na+). Concentrating segment, makes urine hypertonic.

reabsorptionin the ascending loop of hele
salt reabsorption, impermeable to water. makes urine less concentrated as it ascends.

reabsorption in early distal convoluted tubule
+−
Early DCT—reabsorbs Na , Cl . Impermeable to H2O.
Makes urine fully dilute (hypotonic).

reabsorption at the collecting tubule level

how does ADH act on the collecitng tubule?
acts at V2 receptors and promotes the insertion of aquaporin channels on the apical side.

how does aldosterone affect function at the collecting tubule
the CT reabsorbs Na+ in exchange for secreting K+ and H+
aldosterone acts on mineralcorticooid receptors, increasing protein synthesis and causing overall K+ secretion.

role of ADH in cortical collecting duct
The concentration of urine is controlled by antidiuretic hormone, which helps the kidneys to conserve water. Its main effects in the renal tubules is to increase water permeability in the late distal tubule and collecting ducts, increase active transport of sodium chloride in the thick ascending limb of the loop of Henle, and enhance countercurrent multiplication and urea recycling, all of which increase the size of the osmotic gradient.

what transporter is used by the ascending loop of henle (and the PCT) to reabsorb dalts?
the Na/K+ atpase pump. Na+ gets reaborbed. Water stays in urine. urine gets less concentrated.
Reabsorbing sodium, causing more chloride on basolateral side of cell, as well as more adenosine (ATP breakdown). Anatomically, this tubule is right next to afferent arteriole of glomerulus. The entire area is JGA. The production of adenosine of JGA causes a decrease in glomerular filtration rate. Ensures that if the kidney cannot reabsorb sodium, we reduce the amount of sodium going to the kidney in general, preventing excess fluid and salt loss.
Adenosine lowers glomerular filtration rate by constricting afferent arterioles, especially in superficial nephrons, and thus lowers the salt load and transport work of the kidneyconsistent with the concept of metabolic control of organ function.

Tubuloglomerular Feedback
“GFR is in part autoregulated by the rate of fluid delivery to the specialized cells in the macula densa, which begins at the end of the cortical thick ascending limb of the loop of Henle”
- these cells sense change in the delivery and reabsorption of chloride, a process mediated by Na+-K+-2Cl- cotransporters in the apical membrane
- if there is a reduction in renal perfusion pressure, GFR is lowered, less chlroide is then delivered to macula densa, and then a response is done that causes afferent arteriolar dilation, returning the GFR to normal– so that salt reabsorption goes to normal.
- conversely, the afferent arteriole will constrict and GFR will fall in the presence of a rise in renal perfusion pessure that increases GFR.
- the autoregulation of the GFR and distal flow prevents distal reaborptive capacity from being overwhelemd, a prolem that could lead to life-threatening loss of Na and h2O.
-
“It is important to recognize that the macula densa cells have at least two different functions: mediation of tubuloglomerular feedback and regulation of renin release by the juxtaglomerular cells in the afferent arteriole (see Chapter 2). A fall in distal chloride delivery will cause afferent dilatation by tubuloglomerular feedback and increased secretion of renin, leading to efferent constriction. Both of these changes will tend to increase GFR, thereby raising macula densa flow toward normal.”
Excerpt From: Helmut G. Rennke. “Renal Pathophysiology.” Apple Books.

Release of renin from the juxtaglomerular cells
can be induced via 3 mechanisms (RATE- LIMITING STEP)
- decreased stretch of the afferent arteriole (baroreceptors)
- sympathetic nervous systemic stumulation of beta adrenergic receptor stimulation. induced by carotid and aortic bodies baroreceptors
- low Na=/Cl- in the filtrate in the DCT, senses by the macula densa.
outline the RAAS

the __ ___ __ is the site for calcium reabsorption
distal nephron (distal convoluted tubule)



